Abstract
The aim of this study was to investigate the presence of thoughts or wishes for the end of life in patients with Huntington’s disease (HD) or identified gene carriers (further mentioned together as patients). A custom-made questionnaire, based on previous qualitative research, was sent out to 242 patients with HD and identified gene carriers. Presence of wishes was investigated and correlated to demographic and clinical characteristics. A total of 134 patients (55 %) returned the questionnaire. 101 respondents (75 %) reported to have some kind of thoughts or wishes for the end of life. For 15 respondents (11 %) these thoughts concerned care; 86 respondents (64 %) reported to have also thoughts about euthanasia or physician-assisted suicide (PAS). The presence of any thoughts about the end of life was significantly related to being familiar with HD in the family, but not related to any other demographic or clinical variable. Participants with thoughts specifically about euthanasia or PAS were of higher education and in earlier stages of the disease than participants without such thoughts. Thoughts or wishes for the end of life are present amongst patients with HD. These thoughts include euthanasia or PAS in a majority of the respondents. It is suggested that prudential addressing of these issues may enhance the doctor–patient relationship.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Euthanasia and physician-assisted suicide (PAS) are legal in The Netherlands since the law of 2002 passed, but under strict conditions [1]. Euthanasia is defined as death brought upon by a physician at the patient’s explicit request, either voiced orally or based upon a written advance directive [2]. Approximately 2 % of all annual deaths in The Netherlands result from euthanasia or PAS [3]. In The Netherlands we recognize several kinds of advance directives. We recognize advance treatment directives, for example “Do not resuscitate”, which a physician must abide to. A request for euthanasia or PAS, documented in a written advance directive is not a right of a patient but a request, without binding legal consequences [4]. Physicians generally do not initiate a conversation about end-of-life wishes and have difficulty handling an advance directive even though situations for which the advance directive was intended were recognized [5–8].
Huntington’s disease (HD) is an inherited neurodegenerative disease, characterized by movement disorders such as chorea and hypokinesia, by cognitive decline leading to dementia, and by psychiatric symptoms. The localizing gene was identified in 1993 and this discovery made genetic testing possible [9]. In The Netherlands the prevalence is approximately 1,700 patients and another 6,000–8,000 people are at risk [10]. Between 50 and 60 patients suffering from HD die each year [11]. Since 2005, 6–10 HD patients died every year after euthanasia or PAS [12].
Qualitative research, by means of in-depth semi-structured interviews with physicians familiar with HD and HD patients preceded this study [13, 14]. From these studies we concluded that most physicians leave it up to the patient to initiate a conversation about their wishes for the end of life. Furthermore we learned that some patients have specifically articulated their intentions, usually to family members. Other patients already had some ideas or wishes for the future, but did not know if it was possible to document these already or hesitated to discuss these, because their thoughts and wishes were not clear to them yet. We also found that patients underestimated the important role of their physician in the process of documenting wishes for the end of life and in the process of having these wishes fulfilled.
For the purpose of the present study we developed a questionnaire to explore the presence of end-of-life wishes, the reasons for having these wishes, the presence of advance directives and the conversations about end-of-life wishes in a larger group of HD patients or identified gene carriers (further mentioned together as patients) in The Netherlands. The first aim of this study was to explore whether there is any way to predict which patients are most likely to benefit from discussion of end of life issues. We wanted to explore if end-of-life wishes are present in the Dutch HD population, what the wishes include and if the presence of wishes is related to demographic or disease specific characteristics, such as cognition, quality of life and severity of motor symptoms. To investigate if wishes are related to any characteristics, we distinguish two groups, a group of respondents with wishes and a group without any wishes. Furthermore, we make a (second) distinction between respondents considering euthanasia or PAS and respondents with other types of wishes. The second aim was to investigate if HD patients or identified gene carriers use advance directives and if they talk to family or a physician about their wishes.
Methods
Study population
The study was a single center study in the Leiden University Medical Center, which is a national referral center for HD. Patients visiting our out-patient clinics are requested to register in the International HD registry. Those who consented to be included in the registry could also consent to being approached for participation in scientific studies. For this study we screened 296 patients that were included in the registry database since the database was set up. We screened between September and December 2011. Inclusion criteria were: a genetically proven status of HD gene carrier, age above 18, able to communicate either oral or in writing. Exclusion criteria were: no informed consent, suffering from severe depression according to the medical record, absence of a medical record, addiction to alcohol or drugs or having suicidal ideations at present. 55 patients were excluded because they declined informed consent to be approached for scientific research, had severe depression or suicidal ideations or because their last visit was too long ago (>3 years) and we missed accurate information about their present condition.
In addition five patients were included via the Dutch HD patients’ association after posting an announcement in their quarterly. 242 questionnaires were sent out in January 2012. A reminder was sent to non-responders in March 2012.
Instruments and data collection procedure
A custom-made questionnaire was developed for this study. The items were based on clinical experience, literature, and qualitative research that preceded this study [15, 16].
First, information on demographic characteristics was collected. Age was calculated on January 2012, when the questionnaire was sent out. Educational level was evaluated using a nine-point scale that was subsequently categorized into three categories, lower, middle and higher education (according to the categories used in the registry European HD Network questionnaire). Data on the subject’s religion were collected. The importance of religion for the patient was dichotomized into not important and important. Familiarity with HD was assessed by asking if the respondent was familiar with HD in the family and which parent is or was ill.
Second, to explore any wishes about the end of life, the first question concerned if respondents ever thought about the end of life and what the contents of these thoughts were. This question provided several options and the respondent could give multiple answers. In addition, reasons for having these wishes and conversations about the wishes, either with family members or with the general practitioners were assessed. Third, several questions assessed the presence of advance directives for end-of-life wishes. Items regarding the end of life in HD patients addressed euthanasia or PAS, tube feeding, admittance to a nursing home, care at home or treatment for other diseases. We categorized the responses to these items into no wishes, wishes except euthanasia or PAS and wishes including euthanasia or PAS.
Quality of life was evaluated using a nine-point numeric scale ranging from 1 (really bad) to 9 (excellent) (modified from SF-36 [17]).
In addition to the custom-made questionnaire, global functioning was assessed using the total functioning capacity (TFC) subscale of the Unified Huntington’s diseases rating scale (UHDRS). The TFC consists of five questions assessing employment, the capacity to handle financial affairs, manage domestic chores and perform activities of daily living; and the care level provided [18]. Motor function was assessed using the UHDRS motor score (UHDRS-M), ranging from 0 to 124 points [19]. A score below 5 denotes no motor abnormalities. Mini mental state examination (MMSE) data were collected to assess global cognitive functioning [20]. The TFC and UHDRS-M are performed by a neurologist and the MMSE is performed by a neuropsychologist, both experienced with HD, at every visit to our out-patient clinic as part of the registry data collection. The TFC, UHDRS and MMSE scores used in the present study were those that were obtained at the time point closest to the date the questionnaire was completed (or sent), and had to have been collected within the previous 12 months. If the last available test score was more than 1 year earlier, the result was recorded as missing.
Statistical analysis
Data were analyzed with SPSS 20.0. Data are presented as n (%) or mean (SD) as appropriate. The Chi-square test (or Fisher’s Exact test, when appropriate) was used to test for group differences with respect to categorical data, whereas t tests for independent samples were used for normally distributed continuous data and Mann–Whitney U tests for samples with non-normally distributed continuous data. The significance level was set at p < 0.05.
Results
General respondent information
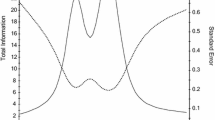
One hundred and thirty-four out of 242 questionnaires were returned, a response rate of 55.4 %. One respondent returned the questionnaire with negative remarks, indicating that this was a subject the respondent did not want to discuss (Fig. 1). If a respondent decided not to answer to a specific question, the result was recorded as missing. Respondent and non-responder characteristics are summarized in Table 1. The non-responders that were deceased or moved were not included in the analysis.
Thirty-four respondents have the maximum TFC score of 13. Thirty-one respondents have the maximum MMSE score of 30 and 36 respondents have a motor score of 5 or lower.
Non-responders were younger and of lower education than responders, but were not different considering gender, having a partner, or disease specific characteristics such as TFC and UHDRS-M.
Thoughts about the end of life
Thirty respondents indicated to have no thoughts about or wishes concerning the end of life. Three respondents did not answer this question. The remaining 101 respondents indicated to have some thoughts about the end of life. Thoughts are for example: “Not the way my mother suffered” or “as soon as I become dependent on others, than it is time to pull the plug” or “euthanasia, yes, but to come to that point, things have to be a lot worse” (for further qualitative statements: see reference 14).
Having witnessed HD in close relatives was significantly associated with the presence of wishes for the end of life. The presence of wishes for the end of life was not associated with gender, age, marital status, education, considering oneself as a religious person, TFC, UHDRS-M, MMSE or quality of life (Table 2).
Respondents with thoughts about or wishes for the end of life
Of the respondents who reported to have thought about the end of life, 86 indicated that wishes concerned thoughts about euthanasia or PAS together with other wishes for example about the possibilities of care. Fifteen respondents indicated that wishes concerned only the possibility of care, either at home or in a nursing home and possibilities of tube feeding and other medical treatments. The reason most often mentioned why thoughts about the end of life emerged was the loss of personal dignity.
Of the respondents who reported to have thought about the end of life, 78 (77.2 %) discussed these wishes with partner or family members. Forty-three (42.6 %) respondents reported to have discussed their wishes with their general practitioner and 58 (57.4 %) did not. Reasons for not talking about end of life wishes were not being ready for it in 26 (45 %) of these respondents and the fact that they had little or no contact with their general practitioner in 16 (28 %) respondents.
Respondents considering euthanasia or physician-assisted suicide
Eighty-six out of 134 respondents had wishes concerning euthanasia or PAS at some point in the disease process (Table 3). The respondents with wishes concerning euthanasia or PAS were of higher education and had lower motor scores, compared to the patients with wishes concerning only care. There was a trend towards higher overall functioning on the TFC for respondents who thought about euthanasia or PAS. Furthermore, respondents with wishes concerning euthanasia or PAS discussed their wishes more often with both family and their general practitioner than respondents with wishes concerning only care. There was a trend towards considering oneself more often as a religious person for respondents with wishes concerning only care at the end of life.
Advance directives
Forty-two respondents (31.3 %) had an advance directive; in 33 cases this is a euthanasia request, together with other kinds of advance directives, for example not to resuscitate (DNR) or a treatment prohibition, and in eight cases this is a euthanasia request only. One respondent did not specify what kind of advance directive he/she had. Respondents with an advance directive are slightly older than respondents without, 54.6 versus 49.2 years of age (p = 0.038) and consider themselves more often as non-religious (p = 0.029).
Discussion
This study shows that, when asked, the majority of HD patients visiting our out-patient clinic have thoughts about their end-of-life. The presence of wishes was not correlated with any demographic variable with the exception of familiarity with the disease in close relatives. The majority of HD patients did discuss their thoughts or wishes for the end of life with their family members, but less than half discussed these with a physician. The majority of the wishes consists of wishes concerning euthanasia or PAS. The presence of advance directives is limited.
This study shows that, at least on the basis of the variables included here, it is not possible for a physician to distinguish, in advance, between patients who have wishes and patients who do not. For this reason physicians should prudentially discuss wishes for the end of life. It is our experience that such attention for intimate issues may enhance and deepen the doctor–patient relationship.
Presence of wishes
Seventy-one percent of respondents in a large Dutch study in the general population (n = 1980) about end-of-life wishes indicated that they have thought about medical treatment and decision making for the end of life [21]. Mean age of the respondents was 53.7 years. 41 % of respondents indicated that they had discussed this subject with family members, and only 4 % with their physician. Respondents in that Dutch study were of higher education than in the general population [21]. Respondents in our study were about the same age. The percentage of respondents that have some kind of end of life wishes in our study is consistent with the national survey, indicating that in The Netherlands wishes for the end of life are present both in healthy citizens and in patients suffering from a neurodegenerative disease. We can conclude that patients with HD do not think about the end of life more or less frequent than persons from the general population, but that there are specific characteristics in HD patients that lead to these thoughts such as being familiar with the disease and motor signs and symptoms.
A larger percentage of respondents in our study discussed their wishes with either family members and/or their physician than in the general population. Most HD families have witnessed the disease course in more than one generation and many of the family members face the disease themselves which may have raised ongoing discussions about what to do in the last stages of the disease.
Both respondents in the national survey and in our study were of higher education than non-responders. On the other hand, level of education was not correlated with the presence of wishes in our study and, therefore, it is unlikely that this potential source of bias influenced our results.
Advance directives
In The Netherlands 95 % of people know about the existence of a law concerning the end of life and 75 % know what the term euthanasia means and includes [21]. 7 % of Dutch inhabitants have an advance directive, usually a euthanasia request in case of dementia [21, 22]. The percentage of patients with an advance directive is higher in our study sample than in the general population. This can be explained by the fact that we investigated a selected sample of known mutation carriers and HD patients. These patients with HD usually witnessed the appalling disease course in one or more close relatives. The need for control and having a say in their own future was reported as a reason for making an advance directive and considering specific arrangements for the end of life (for further reading see the results of our qualitative study in reference 14). Staying in control of one’s life and death and making one’s own medical decisions is part of autonomy and is part of a patient’s identity [23, 24]. The fear of losing autonomy and dignity are described as reasons for asking for euthanasia or making other decisions for the end of life [25, 26]. Research in the USA showed that the prevalence of advance directives increases with age or when people become ill. People seem to formulate an advance directive when it is likely they will need one [27]. Other research showed that discussing end-of-life choices by healthcare workers resulted in a selection of those choices by HD patients, relatives or legal representatives in 75 % of individuals [28].
Religion
In our study considering oneself a religious person was not correlated with the absence or presence of wishes for the end of life, in contrast to other research where religious persons and patients have objections towards euthanasia [29–31].
The Netherlands is a highly secularized country and the debate about euthanasia started in the 1960s [4]. The number of inhabitants visiting a church has been decreasing since 1960. Estimates are that around 2020 more than 70 % of Dutch inhabitants will not be affiliated with any religion [32]. However, in respondents who have wishes, there was a trend among religious patients to think more often about care than about euthanasia or PAS.
The strengths of this study are the relatively large study population of HD patients and identified gene carriers and the fact that we applied few exclusion criteria. There are some limitations that warrant discussion. First, the response rate was 55 %. Analysis of non-responder characteristics showed that non-responders are younger and of lower education, but their disease characteristics do not differ, thus indicating that age could be relevant but disease stage, gender and marital status are not; however, given that age was only marginally related to the presence of wishes, this seems unlikely. We can only speculate about the reasons for not filling in the questionnaire. It cannot be ruled out that particularly those patients who do not want to discuss end of life circumstances decided not to return their questionnaire, which may then have led to some overestimation. Additionally respondents of lower education may be less aware that they can already express their wishes without explanation from their physician first. Together this may have resulted in some selection bias and the study may thus not be regarded as representative for the Dutch HD patients. However, it may also be that non-response is not selective, given that the characteristics of non-responders in our population are similar to those in the general population, i.e., that they are also younger and less well educated. Unfortunately we have no information on the reasons for non-participation.
Second, the majority of respondents still live at home. The group of respondents that live in a nursing home and are in the latter stages of the disease is relatively small. Most patients who have been diagnosed with HD are still able to visit our out-patient clinic. Bias can occur because the wishes of relatively healthy respondents are included in this study and we have limited information of the wishes of more severely affected HD patients. On the other hand, consistent with studies in the USA, it is plausible that when patients become more severely affected and in possible need of an advance directive, and when patients and relatives are educated about the choices, the number of patients who think about the end of life and make choices, increases.
To our knowledge this is the first large study among HD patients to investigate end-of-life wishes and the first study where a relatively unselected large cohort of patients diagnosed with a neurodegenerative disease or knowing that the disease will develop in the future was directly asked about their advanced care planning and wishes surrounding the end of life. We conclude that many HD patients have end-of-life wishes and that we were not able to identify a certain group of patients to whom these questions should be specifically directed. Although HD is a neurodegenerative disease with cognitive decline, it is evident that many patients think about their future, the end of life and about ways to have a say in the end of life. Furthermore, because HD and other neurodegenerative diseases are relentless and result in difficulties with decision making in due course, we advise to discuss end-of-life wishes early in the disease and recommend that physicians initiate these conversations with every patient. The fact that less advanced patients, with higher education level more frequently refer to euthanasia or PAS shows that it is important to talk about these wishes from the earliest stages of HD but also of other neurodegenerative diseases when cognition is still intact and decisions can be made, based on the fact that as disease advances patients progressively loose insight. The finding that less than half discussed their wishes with a physician but many with family members shows that physicians should raise the awareness that the topic is of interest and of importance to the physician.
We recommend that these conversations should not only be held with patients in The Netherlands, where euthanasia and PAS are legal, but also in every other country, because we feel that nearly all patients, irrespective of the country where they reside, will have thoughts or wishes about the end of life. We expect that also patients in countries where euthanasia and PAS are illegal or under debate think about staying in control of their life and want to retain quality of life. For this reason we suggest physicians should ask every patient with HD or any other neurodegenerative disease early in their disease course about their fears, their wishes and thoughts for the future. When talking about euthanasia or PAS is not an option, a physician may discuss, for example, the desirability of tube feeding or the use of antibiotics in the later stages of their disease. In the Netherlands physicians are designated to make medical decisions about starting or withholding treatment and following treatment directives and non-treatment directives, therefore, physicians should hold these conversations. Law and practice in other countries determine which health care professional is the designated person to initiate these conversations.
Furthermore we suggest that wishes for the end of life other than euthanasia or PAS should be studied in patients with HD to examine which questions to ask patients in the early stages of the disease. We suggest that these studies should be carried out using qualitative techniques at first.
References
(2002) Termination of life on request and assisted suicide act
van Tol DG, Rietjens JA, van der Heide A (2012) Empathy and the application of the ‘unbearable suffering’ criterion in Dutch euthanasia practice. Health Policy 105(2–3):296–302
van der Heide A, Onwuteaka-Philipsen BD, Rurup ML, Buiting HM, van Delden JJ, Hanssen-de Wolf JE et al (2007) End-of-life practices in the Netherlands under the Euthanasia act. N Engl J Med 356(19):1957–1965
Griffiths J, Weyers H, Adams M (2008) Euthanasia and Law in Europe. Oxford and Portland. Hart publishing, Oregon
Borgsteede SD, Deliens L, Graafland-Riedstra C, Francke AL, van der Wal G, Willems DL (2007) Communication about euthanasia in general practice: opinions and experiences of patients and their general practitioners. Patient Educ Couns 66(2):156–161
de Boer ME, Hertogh CM, Droes RM, Jonker C, Eefsting JA (2010) Advance directives in dementia: issues of validity and effectiveness. Int Psychogeriatr 22(2):201–208
de Boer ME, Droes RM, Jonker C, Eefsting JA, Hertogh CM (2011) Advance directives for euthanasia in dementia: how do they affect resident care in Dutch nursing homes? Experiences of physicians and relatives. J Am Geriatr Soc 59(6):989–996
Dees MK, Vernooij-Dassen MJ, Dekkers WJ, Elwyn G, Vissers KC, van WC (2013) Perspectives of decision-making in requests for euthanasia: a qualitative research among patients, relatives and treating physicians in the Netherlands. Palliat Med 27(1):27–37
(1993) A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. The Huntington’s Disease Collaborative Research Group. Cell 72(6):971–983
Fisher ER, Hayden MR (2013) Multisource ascertainment of Huntington disease in Canada: prevalence and population at risk. Mov Disord
http://www.cbs.nl. 2014
Booij SJ, Engberts DP, Rodig V, Tibben A, Roos RA (2013) A plea for end-of-life discussions with patients suffering from Huntington’s disease: the role of the physician. J Med Ethics 39(10):621–624
Booij SJ, Rödig V, Engberts DP, Tibben A, Roos RAC (2013) Euthanasia and advance directives in Huntington’s disease: qualitative analysis of interviews with patients. J Huntingtons Dis 2(3):323–330
Britten N (1995) Qualitative interviews in medical research. BMJ 311(6999):251–253
Strauss AL, Corbin J (1998) Basics of qualitative research: techniques and procedures for developing grounded theory. Sage Publications, London
Groenvold M, Petersen MA, Aaronson NK, Arraras JI, Blazeby JM, Bottomley A et al (2006) The development of the EORTC QLQ-C15-PAL: a shortened questionnaire for cancer patients in palliative care. Eur J Cancer 42(1):55–64
Shoulson I, Fahn S (1979) Huntington disease: clinical care and evaluation. Neurology 29(1):1–3
Unified Huntington’s Disease Rating Scale: reliability and consistency. Huntington Study Group. Mov Disord 1996 Mar;11(2):136-42
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
van Delden JJ, van der Heide A, van de Vathorst S, Weyers H, van Tol DG (2011) Kennis en opvattingen van publiek en professionals over medische besluitvorming en behandeling rond het einde van het leven Het KOPPEL-onderzoek. ZonMW, Den Haag
Rurup ML, Pasman HR, Onwuteaka-Philipsen BD (2010) Advance euthanasia directives in dementia rarely carried out. Qualitative study in physicians and patients. Ned Tijdschr Geneeskd 154:A1273
Dupuis HM (2000) Professional autonomy: a stumbling block for good medical practice. an analysis and interpretation. Theor Med Bioeth 21(5):493–502
Jochemsen H, Ten Have H (2000) The autonomy of the health professional: an introduction. Theor Med Bioeth 21(5):405–408
Gastmans C, De Lepeleire J (2010) Living to the bitter end? A personalist approach to euthanasia in persons with severe dementia. Bioethics 24(2):78–86
Hardwig J (1997) Is there a duty to die? Hastings Cent Rep 27(2):34–42
Rurup ML, Onwuteaka-Philipsen BD, van der Heide A, van der Wal G, Deeg DJ (2006) Frequency and determinants of advance directives concerning end-of-life care in The Netherlands. Soc Sci Med 62(6):1552–1563
Dellefield ME, Ferrini R (2011) Promoting excellence in end-of-life care: lessons learned from a cohort of nursing home residents with advanced Huntington disease. J Neurosci Nurs 43(4):186–192
Aghababaei N, Wasserman JA (2013) Attitude Toward Euthanasia Scale: Psychometric Properties and Relations With Religious Orientation, Personality, and Life Satisfaction. Am J Hosp Palliat Med 30:781–785
Leppert W, Gottwald L, Majkowicz M, Kazmierczak-Lukaszewicz S, Forycka M, Cialkowska-Rysz A, et al. (2012) A comparison of attitudes toward euthanasia among medical students at two Polish Universities. J Canc Educ:1–8
Bulow HH, Sprung CL, Baras M, Carmel S, Svantesson M, Benbenishty J et al (2012) Are religion and religiosity important to end-of-life decisions and patient autonomy in the ICU? The Ethicatt study. Intensive Care Med 38(7):1126–1133
Becker J, Hart dJ (2006) Godsdienstige veranderingen in Nederland. Verschuivingen in de binding met de kerken en de christelijke traditie. Den Haag: Sociaal en Cultureel Planbureau
Acknowledgments
We thank all patients for their participation in this study. There was no funding involved.
Ethical standards
The study protocol was approved by the Medical Ethics Committee of the Leiden University Medical Center (MEC LUMC registration number P11.035).
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Booij, S.J., Tibben, A., Engberts, D.P. et al. Thinking about the end of life: a common issue for patients with Huntington’s disease. J Neurol 261, 2184–2191 (2014). https://doi.org/10.1007/s00415-014-7479-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7479-4