Abstract
Behavioral and psychological symptoms of dementia (BPSD) represent common manifestations among patients affected by Alzheimer’s disease (AD). Some reports have recently classified BPSD into specific clusters/subsyndromes exploring the internal structure of the Neuropsychiatric Inventory (NPI). We evaluated whether specific behavioral subsyndromes are associated with worsening cognitive function. Mild to moderate AD patients were recruited from the cohort of the Impact of Cholinergic Treatment USe (ICTUS) study. Neuropsychiatric symptoms were classified in three subsyndromes, identified at baseline, grouping different combinations of NPI items: (1) “psychotic” (“delusions” and/or “hallucinations”); (2) “affective” (“agitation” and/or “depression” and/or “anxiety” and/or “irritability”); and (3) “behavioral” (“euphoria” and/or “apathy” and/or “disinhibition” and/or “aberrant motor behavior”). Mixed model analyses were performed to measure six-monthly changes in the ADAS-Cog score over a follow-up of 2 years, according to these subsyndromes. All analyses were stratified according to AD severity as defined by the Clinical Dementia Rating (CDR). A total of 1,375 AD subjects were recruited. No NPI cluster was found to significantly (p < 0.05) affect the rate of cognitive decline across the 3 CDR classes. Our results suggest that the cognitive course of AD is not substantially influenced by the presence of specific neuropsychiatric phenotypes. Further studies are needed to extend the present findings and identify possible biological and clinical bases for behavioral subsyndromes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behavioral and psychological symptoms of dementia (BPSD) are common features in patients with Alzheimer’s disease (AD) [1]. BPSD have been associated with several negative outcomes (including worsened quality of life [2], functional impairment [3], greater caregiver’s burden [4], and higher hospitalization rates [5]). BPSD represent extremely dynamic conditions. Their severity does not linearly progress, but exponentially increases over the course of the disease [6]. Their clinical manifestation may be influenced by different factors such as the patient’s age at the onset of dementia (BPSD are less likely in patients with early-onset AD) [7], gender (for example, hallucinations and delusions are more common in women) [8], and concomitant pharmacological treatments. Moreover, each BPSD symptom is characterized by different biological [9], neuropathological [10], and psychosocial [11] correlates. Finally, specific BPSD symptoms (e.g. apathy [12] or psychosis [13]) have shown to predict the risk of faster cognitive decline in AD. Therefore, BPSD represent a group of major factors contributing to the heterogeneous expression of the AD phenotype. Despite the above mentioned clinical variability, BPSD are mostly considered in literature as a single manifestation and rarely investigated while taking into account potential confounders (e.g. severity of dementia) by stratifying the study samples. This may have interfered with the correct assessment of their capacity to predict different clinical trajectories over the course of AD.
During the last two decades, several studies have been conducted with the aim of identifying possible AD subsyndromes defined according to the presence of different BPSD. Most of these studies were based on the exploration of the internal structure of the Neuropsychiatric Inventory (NPI) [14], the most widely adopted and recommended [15] clinical tool for evaluating BPSD. The idea of combining specific symptoms into clusters and subsyndromes may provide novel markers of risk, facilitate the understanding of the neuropathophysiological foundation of the disease, and help at better targeting preventive and therapeutical interventions.
The present study is aimed at evaluating whether specific subsyndromes composed by the combinations of different behavioral symptoms are associated with steeper decline of cognitive function in a cohort of mild to moderate AD patients. Therefore, we measured the longitudinal modifications (during a follow-up of 2 years) of the Alzheimer’s Disease Assessment Scale-Cognitive subscale (ADAS-Cog) [16] score according to three BPSD subsyndromes derived from the 10-item version of the NPI [14] in the Impact of Cholinergic Treatment USe (ICTUS) study.
Methods
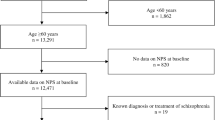
The ICTUS study has been previously described elsewhere [17]. Briefly, the ICTUS study is a prospective, multicenter cohort study aimed at evaluating the natural history, treatment outcomes, and socioeconomic impact of AD in Europe. All the 29 participating centers from 12 European countries were members of the European Alzheimer Disease Consortium (EADC), a network of clinical and research institutions specialized in the diagnosis and treatment of AD. The participating centers were grouped into four clusters (Northern, Western, Eastern and Southern Europe) according to the established UN-classification of European countries [18]. Clustering was used as a proxy for the healthcare- and welfare-system reflecting the European North-to-South gradient [19].
The following inclusion criteria were adopted in the ICTUS study: (1) diagnosis of probable AD made according to National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) criteria [20]; (2) Mini Mental State Examination (MMSE) [21] score ranging from 10 to 26; (3) living in the community with the presence of a well-identified, informal caregiver; (4) absence of known conditions reducing to less than 2 years the patient’s life expectancy; and (5) ability to sign an informed consent. After the baseline assessment (occurred between February 2003 and July 2005), participants received follow-up for 2 years with mid-term re-evaluations every 6 months.
The study was approved by the Ethics Committee of the Toulouse University Hospital (coordinating center) and at individual centers by local or national ethical committees. All the study participants provided written informed consent.
At the baseline assessment and at each follow-up visit, a comprehensive clinical and neuropsychological assessment was performed. In particular, the following scales and questionnaires were administered to evaluate the neurological, functional, and social factors of participants: Clinical Dementia Rating (CDR) [22], MMSE [21], ADAS-Cog [16], Zarit Burden Interview (ZBI) [23], NPI [14], Activities of Daily Living scale (ADL) [24], and Instrumental Activities of Daily Living scale (IADL) [25]. Moreover, at every visit, concomitant pharmacological treatments were recorded.
Cohort stratification
For the present analyses, we chose to stratify the study sample into three groups according to the severity of dementia, consistently with the different manifestations of BPSD occurring over the AD course. The severity of dementia was defined by the CDR score, and the three groups of severity were identified as (1) CDR equal to 0.5, (2) CDR equal to 1, and (3) CDR equal to or higher than 2.
Independent variables
In the ICTUS study, BPSD were assessed with the 12-item NPI version [26]. The NPI consists of a retrospective (up to 1 month) assessment of ten (in its original version [14]) or twelve (in a subsequent version [26]) neuropsychiatric symptoms commonly present in dementia. Each symptom is rated, when present, in terms of severity (ranging from 1, “mild”, to 3, “severe”) and frequency (ranging from 1, “occasionally”, to 4, “very frequently”). If the symptom is absent, the domain scores equals zero. The score of each item is then calculated by multiplying severity x frequency, thus obtaining a score ranging between 0 and 12. The total NPI score is finally obtained by adding all the single item scores (thus, ranging from 0 to 120 or 144, according to the adopted version) with higher scores indicating greater psychopathology. In our study, each symptom was considered only if “clinically relevant”, that is, defined by a NPI frequency × severity score equal to or higher than 4.
The NPI items were grouped at baseline into three subsyndromes previously identified in the literature [27], composed by different combinations of the following symptoms: (1) “psychotic” cluster (“delusions” and/or “hallucinations” items); (2) “emotional” cluster (“agitation/aggression” and/or “depression/dysphoria” and/or “anxiety” and/or “irritability” items); (3) “behavioral” cluster (“elation/euphoria” and/or “apathy” and/or “disinhibition” and/or “aberrant motor behavior” items). The items “sleep and night-time behavior disorders” and “appetite and eating disorders” were not adopted in the present analyses because they were not included in the subsyndromes derived by Garre-Olmo and colleagues [27] on the basis of the 10-item version of the NPI. In this context, we observed that among studies exploring the internal structure of the NPI in order to define behavioral syndromes, more consistent results were obtained by adopting the 10-item version of the NPI rather than the more recent 12-item one.
Dependent variable
Modifications of the ADAS-Cog [16] score were considered as outcome variables of interest. The ADAS-Cog represents the most widely adopted cognitive outcome measure in AD trials. It includes eleven items assessing different cognitive domains (memory, language, and praxis). The scores of each item are summed to generate a total score, indicating the severity of the cognitive impairment. The total ADAS-Cog score ranges from 0 to 70, with higher scores indicating greater cognitive impairment.
Covariates
The following variables were considered as potential confounders to be included in the adjusted statistical models: age, sex, education.
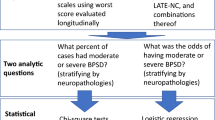
Statistical analysis
In order to compare the baseline characteristics between the 3 CDR subgroups, we used χ2 or Fisher’s exact (for expected values <5) test for categorical variables, Fisher tests for quantitative variables with Gaussian (normal) distributions, and non-parametric tests (Kruskal–Wallis test) for quantitative variables without normal distributions.
In order to compare changes over time for ADAS-Cog scores between patients with NPI symptoms and patients without NPI symptoms for each group of CDR score, we used linear mixed-effect models with random intercepts and random slopes to take into account the heterogeneity of baseline scores and individual slopes over time. In the group of CDR score = 0.5, the terms time2 and time3 were significant, showing that the ADAS-Cog slope is cubic. In the group of CDR score = 1, only the term time2 was significant, showing that the ADAS-Cog slope is quadratic in this group. In the group of CDR score ≥2, the terms time2 and time3 were not significant, showing that the progression of ADAS-Cog is linear in this group.
Two models were used. Model 1 was an unadjusted model and included the following variables as fixed effects: NPI symptom, time and NPI symptom × time interaction term. Model 2 was adjusted including the same terms as model 1, as well as potential confounders (PC) and their interaction with time. The PC was gender, age and education (number of years of formal education including primary school).
p values were based on two-sided tests and were considered statistically significant if p < 0.05.
Statistical analyses were performed using SAS 9.3 software (SAS Institute Inc., Cary, NC, USA).
Results
The main characteristics of the study sample at the baseline assessment are shown in Table 1. A total of 1,375 AD subjects (64.7 % women) were recruited in the ICTUS study. Nevertheless, the present analyses were conducted on 1,372 subjects due to missing data in three patients. The sample population had a mean age of 76.3 (SD 7.7) years. Patients showed a moderate cognitive impairment (mean MMSE and ADAS-Cog scores of 20.4, SD 3.9, and 21.0, SD 9.6, respectively). The sample had a mean NPI score of 13.0 (SD 13.7). Almost 90 % of participants had a CDR score equal to 0.5 or 1, whereas only 13.3 % had more severe stages of AD. The three CDR subgroups were significantly different for age (p < 0.001) and gender (p = 0.02), but comparable for AChE-I treatment (p = 0.54).
The “psychotic” subsyndrome was identified in 145 (10.7 %) subjects, the “emotional” subsyndrome in 607 (44.6 %) subjects, and the “behavioral” subsyndrome in 528 (38.9 %) subjects. Nearly 40 % of patients didn’t exhibit any BPSD. As expected, the prevalence of all the neuropsychiatric subsyndromes increased with the severity of dementia.
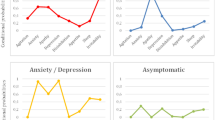
The evolution of ADAS-Cog scores from baseline to 24 months according to the three behavioral subsyndromes of interest is presented in Table 2. Overall, all participants presented a worsening of the ADAS-Cog score after 2 years of follow-up, with worse results for those having more severe stages (i.e., CDR ≥ 2) of the Alzheimer’s disease at the baseline. The differences in ADAS-Cog scores between patients exhibiting and not-exhibiting specific subsyndromes at each follow-up assessment are shown in Table 3. No statistical significance was reported for the ADAS-Cog differences between participants with and without specific subsyndromes over the follow-up across the three different CDR groups (all p values >0.05). Nevertheless, suggestive results (p < 0.1) were found. In the group of participants with CDR equal to 0.5, subjects with the “psychotic” subsyndrome were found to cognitively decline more rapidly compared to CDR 0.5 participants without psychotic symptoms only at the 12-month assessment [ADAS-Cog modification +2.33, standard error, (SE) 1.29; p = 0.07]. However, such a trend was not confirmed at the following evaluations. More interestingly, in participants with a CDR ≥ 2, the presence of the “behavioral” subsyndrome was associated with a faster cognitive decline at each follow-up visit compared to participants in the same CDR group but without behavioral symptoms. In fact, the ADAS-Cog difference between participants with and without the subsyndrome was +1.09 (SE 0.60) at 6 months (p = 0.07), +2.18 (SE 1.20) at 12 months (p = 0.07), +3.26 (SE 1.80) at 18 months (p = 0.07), and +4.35 (SE 2.40) at 24 months (p = 0.07). After adjusting for potential confounders, results were substantially confirmed (Table 3).
Discussion
To our knowledge, this is the first study evaluating the impact of different neuropsychiatric subsyndromes on the rate of cognitive decline in a large cohort of mild to moderate AD patients. In our study, we did not find statistically significant relationships between neuropsychiatric clusters and cognitive decline, indicating that the cognitive progression of AD seems to be scarcely affected by the presence of specific behavioral syndromes. However, the suggestive relationships we found for the “behavioral” subsyndrome in patients with most advanced stages of disease may support the utility of grouping BPSD in different clinical phenotypes.
Identifying clinical predictors of a rapid cognitive progression currently represents a major challenge in the approach to treating AD patients. In fact, the typical manifestation of the disease as a slowly progressive course is not always present. A significant heterogeneity of cognitive decline trajectories has been demonstrated, and different phenotypic categories proposed (e.g., “rapidly progressive AD” [28]). Several risk factors for more aggressive forms have already been identified [28]. In this context, some BPSD, like apathy [12] and psychosis [13], have been shown to individually predict the accelerated worsening of cognitive performances in AD patients.
To our knowledge, only one study [29] investigated BPSD after grouping them into neuropsychiatric clusters using the NPI. In this paper, 20 AD patients affected by a “psychotic” subsyndrome (“delusions” + “hallucinations” + “agitation/aggression” + “irritability”) were found to exhibit a faster dementia progression, while 14 subjects with a “frontal” subsyndrome (“elation/euphoria” + “disinhibition”) showed a slower rate of decline. By focusing on clinical phenotypes (defined as groups of symptoms frequently occurring together) rather than on single symptoms, the evaluation of BPSD might be promoted in clinical practice and the prognostic accuracy improved. Unfortunately, there is currently no consensus about the proper definition of behavioral subsyndromes. The available studies exploring the internal structure of the NPI in the attempt to identify neuropsychiatric clusters in AD show a very low concordance in their results. In the present study, we adopted the three subsyndromes previously defined by Garre-Olmo and colleagues [27] for the following reasons: (1) the ICTUS population was very similar to the one in which these subsyndromes were identified (in terms of subjects’ mean age, NPI total score, and clinical setting); (2) both studies enrolled only mild to moderate ambulatory AD patients; and (3) the identified clusters were derived from repeated longitudinal evaluations confirming their internal consistency.
Some limitations may have potentially influenced our results. First, BPSD represent extremely dynamic conditions. They are known to not progress linearly and to markedly fluctuate during the course of the disease. This may have affected the stability over time of the adopted behavioral clusters (e.g. some patients may have changed their neuropsychiatric phenotype during the follow-up). Second, we considered for the composition of subsyndromes only “clinically relevant” behavioral symptoms, defined in line with previous studies [30–32]. It may be hypothesized that BPSD might more significantly influence the progression of cognitive decline when reaching a higher severity. Third, we observed in our cohort a rate of dementia progression, measured as variations in ADAS-Cog scores, that was significantly slower than other observational studies. The progression of the disease in mild to moderate AD patients has been estimated as a gain of 5.5 points on the ADAS-Cog per year for a population with a mean baseline value of 25 [33]. In our cohort, we observed a slower progression of the disease (mean ADAS-Cog modification per year: +3.62 in the first year, +4.58 in the second year of follow-up) which may have underestimated our findings.
Besides these limitations, our study still has several strengths. First, our analyses were conducted in a large sample size of AD patients, followed over a relatively long follow-up. These characteristics of the ICTUS study are not common in the literature, given the difficulties of conducting research projects in patients with dementia [34]. Moreover, the study design with semi-annual clinical assessments provided a detailed monitoring of cognitive changes. Finally, our analyses were stratified according to dementia severity, allowing the correct investigation of cognitive decline, given the well-established tendency of BPSD to increase over the course of the disease.
In conclusion, our study represents the first attempt at evaluating BPSD subsyndromes in the prediction of different cognitive decline trajectories in AD patients. Our findings, despite some suggestive results, indicate that the identification of specific behavioral phenotypes does not allow for accurate prediction of the rate of cognitive decline. In consideration of their relevant heterogeneity, BPSD and, consequently, neuropsychiatric subsyndromes, should always be investigated taking into account potential confounders by stratifying the study samples. In particular, their marked variability over time should be necessarily held in high consideration. Further studies are needed to confirm our findings and specifically explore the predictive value of behavioral subsyndromes in AD patients.
References
Finkel SI, Costa e Silva J, Cohen G, Miller S, Sartorious N (1996) Behavioral and psychological signs and symptoms of dementia: a consensus statement on current knowledge and implications for research and treatment. Int Psychogeriatr 8(Suppl 3):497–500
Missotten P, Squelard G, Ylieff M, Di Notte D, Paquay L, De Lepeleire J, Buntinx F, Fontaine O (2008) Relationship between quality of life and cognitive decline in dementia. Dement Geriatr Cogn Disord 25:564–572
Peters KR, Rockwood K, Black SE, Bouchard R, Gauthier S, Hogan D, Kertesz A, Loy-English I, Beattie BL, Sadovnick AD, Feldman HH (2006) Characterizing neuropsychiatric symptoms in subjects referred to dementia clinics. Neurology 66:523–528
Germain S, Adam S, Olivier C, Cash H, Ousset PJ, Andrieu S, Vellas B, Meulemans T, Reynish E, Salmon E, ICTUS-EADC Network (2009) Does cognitive impairment influence burden in caregivers of patients with Alzheimer’s disease? J Alzheimers Dis 17:105–114
Voisin T, Andrieu S, Cantet C, Vellas B (2010) Predictive factors of hospitalizations in Alzheimer’s disease: a two-year prospective study in 686 patients of the REAL.FR study. J Nutr Health Aging 14:288–291
Thompson C, Brodaty H, Trollor J, Sachdev P (2010) Behavioral and psychological symptoms associated with dementia subtype and severity. Int Psychogeriatr 22:300–305
Toyota Y, Ikeda M, Shinagawa S, Matsumoto T, Matsumoto N, Hokoishi K, Fukuhara R, Ishikawa T, Mori T, Adachi H, Komori K, Tanabe H (2007) Comparison of behavioral and psychological symptoms in early-onset and late-onset Alzheimer’s disease. Int J Geriatr Psychiatry 22:896–901
Schneider LS, Dagerman KS (2004) Psychosis of Alzheimer’s disease: clinical characteristics and history. J Psychiatr Res 38:105–111
Robert PH, Verhey FRJ, Byrne EJ, Hurt C, De Deyn PP, Nobili F, Riello R, Rodriguez G, Frisoni GB, Tsolaki M, Kyriazopoulou N, Bullock R, Burns A, Vellas B (2005) Grouping for behavioral and psychological symptoms in dementia: clinical and biological aspects. Consensus paper of the European Alzheimer disease consortium. Eur Psychiatry 20:490–496
Casanova MF, Starkstein SE, Jellinger KA (2011) Clinicopathological correlates of behavioral and psychological symptoms of dementia. Acta Neuropathol 122:117–135
de Vugt ME, Stevens F, Aalten P, Lousberg R, Jaspers N, Winkens I, Jolles J, Verhey FR (2004) Do caregiver management strategies influence patient behaviour in dementia? Int J Geriatr Psychiatry 19:85–92
Starkstein SE, Jorge R, Mizrahi R, Robinson RG (2006) A prospective longitudinal study of apathy in Alzheimer’s disease. J Neurol Neurosurg Psychiatr 77:8–11
Wilkosz PA, Seltman HJ, Devlin B, Weamer EA, Lopez OL, DeKosky ST, Sweet RA (2010) Trajectories of cognitive decline in Alzheimer’s disease. Int Psychogeriatr 22:281–290
Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J (1994) The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 44:2308–2314
Jeon Y-H, Sansoni J, Low L-F, Chenoweth L, Zapart S, Sansoni E, Marosszeky N (2011) Recommended measures for the assessment of behavioral disturbances associated with dementia. Am J Geriatr Psychiatry 19:403–415
Rosen WG, Mohs RC, Davis KL (1984) A new rating scale for Alzheimer’s disease. Am J Psychiatry 141:1356–1364
Reynish E, Cortes F, Andrieu S, Cantet C, Olde Rikkert M, Melis R, Froelich L, Frisoni GB, Jönsson L, Visser PJ, Ousset PJ, Vellas B, ICTUS Study Group (2007) The ICTUS Study: a prospective longitudinal observational study of 1,380 AD patients in Europe. Study design and baseline characteristics of the cohort. Neuroepidemiology 29:29–38
Anon (2004) World Population Prospects. The 2004 Revision, CD-ROM Edition (United Nations publication, Basic Dataset, Sales No. E.05.XIII.10; Comprehensive Dataset, Sales No. E.05.XIII.11; Extended Dataset, Sales No. E.05.XIII.12)
Wimo A, Winblad B, Jönsson L (2010) The worldwide societal costs of dementia: estimates for 2009. Alzheimers Dement 6:98–103
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34:939–944
Folstein MF, Folstein SE, McHugh PR (1975) « Mini-mental state » . A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Morris JC (1993) The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 43:2412–2414
Zarit SH, Reever KE, Bach-Peterson J (1980) Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 20:649–655
Katz S, Ford AB, Moskovitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychological function. JAMA 185:914–919
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Cummings JL (1997) The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology 48(5 Suppl 6):S10–S16
Garre-Olmo J, López-Pousa S, Vilalta-Franch J, de Gracia Blanco M, Vilarrasa AB (2010) Grouping and trajectories of the neuropsychiatric symptoms in patients with Alzheimer’s disease, part I: symptom clusters. J Alzheimers Dis 22:1157–1167
Schmidt C, Wolff M, Weitz M, Bartlau T, Korth C, Zerr I (2011) Rapidly progressive Alzheimer disease. Arch Neurol 68:1124–1130
Frisoni GB, Rozzini L, Gozzetti A, Binetti G, Zanetti O, Bianchetti A, Trabucchi M, Cummings JL (1999) Behavioral syndromes in Alzheimer’s disease: description and correlates. Dement Geriatr Cogn Disord 10:130–138
Aalten P, de Vugt ME, Jaspers N, Jolles J, Verhey FRJ (2005) The course of neuropsychiatric symptoms in dementia. Part I: findings from the two-year longitudinal Maasbed study. Int J Geriatr Psychiatry 20:523–530
Aalten P, Verhey FRJ, Boziki M, Bullock R, Byrne EJ, Camus V, Caputo M, Collins D, De Deyn PP, Elina K, Frisoni G, Girtler N, Holmes C, Hurt C, Marriott A, Mecocci P, Nobili F, Ousset PJ, Reynish E, Salmon E, Tsolaki M, Vellas B, Robert PH (2007) Neuropsychiatric syndromes in dementia. Results from the European Alzheimer Disease Consortium: part I. Dement Geriatr Cogn Disord 24:457–463
Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S (2002) Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA 288:1475–1483
Ito K, Ahadieh S, Corrigan B, French J, Fullerton T, Tensfeldt T, Alzheimer’s Disease Working Group (2010) Disease progression meta-analysis model in Alzheimer’s disease. Alzheimers Dement 6:39–53
Pahor M, Cesari M (2012) Study design: randomized controlled trials. In: Newman AB, Cauley JA (eds) The epidemiology of aging. Springer, New York (in press)
Acknowledgments
The ICTUS study was partially supported by a grant from the European Commission within the 5th framework program and partially from an unrestricted equal grant from each of Eisai, Jansen, Lundbeck, and Novartis pharmaceutical companies. The pharmaceutical companies had no role in study design, data collection, data analysis, or data interpretation. Promotion of the ICTUS study was supported by the University Hospital Centre of Toulouse. The data sharing activity was supported by the “Association Monegasque pour la recherche sur la maladie d’Alzheimer”(AMPA) and the UMR 1027 Unit INSERM-University of Toulouse III.
Conflicts of interest
None.
Ethical standard
Authors declare that all the described procedures have been approved by the appropriate ethics committee and therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Members of the group ICTUS/DSA Group is listed in Appendix.
Appendix: ICTUS/DSA Group refers to
Appendix: ICTUS/DSA Group refers to
ICTUS study Group: Vellas B., Reynish E., Ousset PJ., Andrieu S. (Toulouse), Burns A. (Manchester), Pasquier F. (Lille), Frisoni G. (Brescia), Salmon E. (Liège), Michel J.P., Zekry D.S. (Geneva), Boada M. (Barcelona), Dartigues J.F. (Bordeaux), Olde-Rikkert M.G.M. (Nijmejen), Rigaud A.S. (Paris), Winblad B. (Huddinge), Malick A., Sinclair A. (Warwick), Frölich L. (Mannheim), Scheltens P. (Amsterdam), Ribera C. (Madrid), Touchon J. (Montpellier), Robert P. (Nice), Salva A. (Barcelona), Waldmar G. (Copenhagen),Bullock R. (Swindon), Costa-Tsolaki M. (Thesaloniki), Rodriguez G. (Genoa), Spiru L. (Bucharest), Jones R.W. (Bath), Stiens G., Stoppe G. (Goettingen), Eriksdotter Jönhagen M. (Stockholm), Cherubini A. (Perugia), Lage P.M., Gomez-Isla T. (Pamplona), Camus V. (Tours), Agüera-Morales E., Lopez F. (Cordoba).
DSA Group: Andrieu S., Savy S., Cantet C., Coley N.
Rights and permissions
About this article
Cite this article
Canevelli, M., Adali, N., Cantet, C. et al. Impact of behavioral subsyndromes on cognitive decline in Alzheimer’s disease: data from the ICTUS study. J Neurol 260, 1859–1865 (2013). https://doi.org/10.1007/s00415-013-6893-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-013-6893-3