Abstract
Multiple sclerosis (MS) is a demyelinating disease affecting the central nervous system, frequently associated with cognitive impairments. Damages of the cerebellum are very common features of patients with MS, although the impact of this clinical factor is generally neglected. Recent evidence from our group demonstrated that MS patients with cerebellar damages are characterized by selective cognitive dysfunctions related to attention and language abilities. Here, we aimed at investigating the presence of neuroanatomical abnormalities in relapsing–remitting MS patients with (RR-MSc) and without (RR-MSnc) cerebellar signs. Twelve RR-MSc patients, 14 demographically, clinically, and radiologically, matched RR-MSnc patients and 20 controls were investigated. All patients underwent neuropsychological assessment. After refilling of FLAIR lesions on the 3D T1-weighted images, VBM was performed using SPM8 and DARTEL. A correlation analysis was performed between VBM results and neuropsychological variables characterizing RR-MSc patients. Despite a similar clinical status, RR-MSc patients were characterized by more severe cognitive damages in attention and language domains with respect to RR-MSnc and controls. With respect to controls, RR-MSnc patients were characterized by a specific atrophy of the bilateral thalami that became more widespread (including motor cortex) in the RR-MSc group (FWE < 0.05). However, consistent with their well-defined neuropsychological deficits, RR-MSc group showed atrophies in the prefrontal and temporal cortical areas when directly compared with RR-MSnc group. Our results demonstrated that RR-MS patients having cerebellar signs were characterized by a distinct neuroanatomical profile, mainly involving cortical regions underpinning executive functions and verbal fluency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For several decades, the cerebellum has been considered to be involved strictly in motor control. With the advent of modern functional neuroimaging techniques, increasing attention has been given to mapping the involvement of the cerebellum in cognition. In fact, a broad range of studies has demonstrated the key role of the cerebellum in: executive functions, working memory, visuo-spatial functions, language, procedural learning and attention (for a review, see [1]). The “cognitive profile” of the cerebellum is dependent upon the existence of well-established anatomical connections between this sub-cortical area and a number of high-level cortical regions [2–6].
Clinically speaking, patients with lesions confined to the cerebellum often present with cerebellar motor syndrome, characterized by dysmetria, dysarthia, and ataxia. Furthermore, cerebellar damage might also result in the well-defined “cerebellar cognitive affective syndrome” [6], a complex syndrome that includes executive dysfunction, language deficits, and impairments in spatial cognition. Anatomically, several neuroimaging studies have provided evidence for the existence of distinct topographical organizations (anterior vs. posterior lobule) aimed at regulating the motor and cognitive profiles of the cerebellum [7].
Multiple sclerosis (MS) is an extremely heterogeneous neurological disorder, both at the clinical and pathological level, characterized by motor and cognitive dysfunctions. The vast majority of cross-sectional studies on MS-related cognitive impairments have shown that 40–60 % of cases have prominent deficits in memory, language, attention and information processing speed [8, 9]. Damages to the cerebellum is a very common feature of patients with MS. It has been estimated that approximately 30 % of patients with relapsing–remitting MS (RR-MS) present at least one lesion within the cerebellum, while in roughly 11 % of MS patients the motor cerebellar symptoms and signs (dysmetria, dysarthria and ataxia) represent the predominant clinical manifestation [10].
At this moment, whether and how cerebellar damages impact on the cognitive profile of patients with MS still remains unclear. Recently, we demonstrated that cognitive impairment is more severe in patients with cerebellar symptoms (RR-MSc) compared with patients without cerebellar dysfunction (RR-MSnc) and that these deficits belong to the domains of attention and language [11], contributing to the view that the cerebellum is specifically enrolled in these cognitive functions [1–6].
The investigation of MS patients with cerebellar damage offers a unique opportunity to disentangle the contribution of the cerebellum in brain-related cognitive dysfunctions in MS patients. It is reasonable to assume that there is a strict relationship between the severity of cognitive impairment and the presence and extension of MS pathology. In the literature, the relationship between cognitive decline and the presence and extent of MS pathology are often elusive [9, 12]. For this reason, determining more precisely the intimate link between specific brain circuits and distinct cognitive profiles may be an important advancement for future refinements of MS diagnosis. Given these premises, it appears important to clarify the pathophysiological role of cerebellar damages in determining the distinct cognitive profile of MS patients with and without cerebellar signs. For this reason, we employed voxel-based morphometry (VBM), a fully automated quantitative magnetic resonance imaging (MRI) technique, extensively employed to reveal in vivo neuropathological changes in the neurological brain. More importantly, a different MS population with respect to our previous studies [11, 13] has been investigated in order to improve the statistical power of our findings.
Methods
Subjects
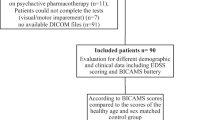
Our sample consisted of 62 patients with RR-MS according to McDonald and Polman criteria [14]. All subjects were recruited from the Neurology Unit of the University “Magna Graecia” of Catanzaro. Patients’ inclusion criteria were: (1) no concomitant therapy with antidepressant or psychoactive drugs; (2) no evidence of dementia (MMSE ≤ 24; (3) Expanded Disability Status Scale (EDSS) [15] score from 0 to 5; and (4) no history of psychiatric problems, according to the Structured Clinical Interview of the DSM-IV [16]. All patients were clinically evaluated by two neurologists (RN, DP), blind to any other result and with over 15 years of experience in MS. The clinical assessment also included the Fatigue Severity scale (FSS) [17].
From the initial cohort, 12 MS patients with predominant cerebellar symptoms (RR-MSc) and with evident lesion load (as assessed by structural MRI scanning) within the cerebellum were selected. In the RR-MSc group, the most common manifestations were gait ataxia and dysmetria, followed by tremor and dysdiadochokinesis and nystagmus. These patients were matched for clinical variables with 14 MS patients without any cerebellar dysfunction (RR-MSnc). Fifty healthy volunteers with no previous history of neurological/psychiatric diseases and with normal MRI of the brain were matched for demographic variables with MS patients. All participants gave written informed consent, which was approved by the Ethical Committee of the University ‘Magna Graecia’ of Catanzaro, according to the Helsinki Declaration.
Neuropsychological assessment
All patients completed an extensive battery of neuropsychological tests [11] administered by an experienced clinical neuropsychologist blinded to clinical results. The neuropsychological tests assessed: (a) verbal memory: immediate and delayed recall and recognition of lists of words (IR, DR and Rec) (Rey Auditory-Verbal Learning Test, RAVLT); (b) spatial memory: immediate and delayed recall (IR and DR) (Rey–Osterrieth Complex Figure Test, ROCFT); (c) visuo-spatial processing: Judgment Line Orientation Test (JLO) and Rey–Osterrieth Complex Figure Test Copy (ROCFT Copy); (d) sustained attention and processing speed (Symbol Digit Modalities Test) (SDMT); (e) verbal fluency (Controlled Oral Word Association Test, COWAT) and (f) abstract/conceptual reasoning (Modified Card Sorting Test Categories Achieved and Perseverative Errors, MCST CA and PE). None of the subjects had been previously exposed to this neuropsychological evaluation. Finally, global cognitive function was tested using the Mini Mental State Examination (MMSE). Results were compared with Italian published norms [18, 19].
Magnetic resonance imaging
Brain MRI was performed according to our routine protocol by a 1.5-T unit (Signa NV/I; GE Medical Systems, USA). 2D fast fluid-attenuated inversion-recovery (FLAIR) axial images (TR 8,000 ms, TE 120 ms; 256 × 224 image matrix, FOV: 24 cm; 24 slices, 4-mm slices, 1-mm gap) were used to calculate hyperintense lesion volume. Structural MRI data were acquired using a 3D T1-weighted spoiled gradient (SPGR) echo sequence with the following parameters: TR = 15.2 ms; TE = 6.7 ms; flip angle 15°; matrix size 256 × 256; FOV = 24 cm; slice thickness = 1.2 mm.
Lesion load quantification
Total lesion load (TLL) quantification was performed using a supervised automated segmentation method [20] that used the image intensities of the FLAIR images to train a classifier (cellular neural network (CNN)-based approach). The resulting final lesion load probability map was anatomically subdivided into cerebellar and supratentorial compartments. An experienced neuroradiologist (blind to any other result of this study) double-checked CNN-related final maps and manually performed lesion load quantification using MRIcro software (http://www.mricro.com).
Voxel-based morphometry
Data were processed using the SPM8 software (http://www.fil.ion.ucl.ac.uk/spm), where we applied VBM implemented in the VBM8 toolbox, incorporating the DARTEL toolbox that was used to obtain a high-dimensional normalization protocol [21]. Images were bias-corrected, tissue classified, and registered using linear (12-parameter affine) and non-linear transformations, within a unified model. Subsequently, the warped gray matter (GM) segments were affine-transformed into MNI space and were scaled by the Jacobian determinants of the deformations (modulation). Finally, the modulated volumes were smoothed with a Gaussian kernel of 8 mm.
To avoid MS lesion misclassification, a validated approach was employed [22]. Specifically, white matter (WM) lesions were masked out from the GM maps and reassigned to WM maps after each segmentation was run. To this end, a lesion mask from the automated segmented lesions visible on FLAIR images was created (by using our validated approach), co-registered to the 3D T1-weighted space, using the rigid transformation calculated between the FLAIR and the 3D T1-weighted images, and normalized into the MNI space, using the nonlinear transformation previously calculated. To exclude from the statistical analysis pixels assigned by the segmentation to GM with a low probability value and pixels with a low intersubject anatomic overlay after normalization, GM normalized maps from all the subjects were eroded (erosion of the first-line outer voxels) and used to create a GM mask, which was thresholded at a value of 0.75 (pixels with computed GM fraction values 75 % were selected) and then used as explicit mask during the statistical analysis [22].
The GM volume maps were statistically analyzed using the general linear model based on Gaussian random field theory. Statistical analysis consisted of an analysis of covariance with age and total intracranial volume (ICV) as covariates of no-interest. To evaluate co-variation between GM volume changes and clinical/cognitive data we performed correlation analysis using the multiple regression function of SPM8. The statistical threshold was set at p < 0.05 family-wise error (FWE) correction at a whole brain level.
Automated cerebellar volumetry
To corroborate voxel-based findings we further performed automated labelling and quantification of cerebellar volume using FreeSurfer v5.0 ((http://surfer.nmr.mgh.harvard.edu). The automated procedures for volumetric measuring of several deep GM structures have been previously described [23, 24]. This procedure automatically provided segments and labels for up to 40 unique structures and assigned a neuroanatomical label to each voxel in an MRI volume based on probabilistic information estimated automatically from a manually labeled training set. The automated subcortical segmentation performed by Freesurfer required the following steps: first, an optimal linear transform is computed that maximizes the likelihood of the input image, given an atlas constructed from manually labeled images. A nonlinear transform is then initialized with the linear one, and the image is allowed to further deform to better match the atlas. Finally, a Bayesian segmentation procedure is performed, and the maximum a posteriori estimate of the labeling is computed. This approach provides advantages similar to manual ROI drawing [24] without the potential for rater bias, offering an anatomically accurate rendering of regional volumes. ICV was calculated and used to correct the regional brain volume measurements. Normalized cerebellar GM values were calculated as follows: [raw cerebellar volume/ICV]*1,000.
Statistical analysis
Statistical analyses were performed with STATISTICA Version 6.0 (www.statsoft.com). Demographic, radiological and neuropsychological differences between groups were tested with unpaired ttest and one-way ANOVAs. For ordinal variables (i.e., EDSS subscales and educational level), the Mann–Whitney U test was used to assess differences between groups. All statistical analyses had two-tailed alpha levels of <0.05 for defining significance.
Results
All groups were matched for demographic variables and, within the two MS groups, no significant differences were detected for clinical variables (Table 1). As concerns MRI data, no significant differences in supratentorial TLL, as well as in cerebellar GM volume, were detected between MS groups. In contrast, RR-MSc patients obviously showed a greater lesion load within the cerebellum with respect to the RR-MSnc group (Table 1). The most commonly affected regions were the pons and the cerebellar peduncles.
As concerns cognitive evaluation, RR-MSc displayed significant lower performance in attention (SDMT), verbal fluency (COWAT) and spatial memory tests (ROCFT) (Table 1), either with respect to RR-MCnc patients or to controls (post hoc analysis—Tukey t test—p’s < 0.05).
VBM analysis revealed that patients with RR-MSnc and RR-MSc showed a similar pattern of GM atrophy involving mainly the thalamus when compared with controls. RR-MSc group was further characterized by additional loci of atrophy involving the putamen and the primary motor cortex bilaterally (Table 2; Fig. 1). However, when we compared MS groups between them, RR-MSc showed a reduced volume in the right supramarginal gyrus, bilateral superior temporal gyrus (STG) and in the right dorsolateral prefrontal cortex (DLPFC, Fig. 2a).
3D/2D surface renders showing the significant clusters deriving from the direct comparison between RR-MS groups and healthy controls superimposed onto the T1-weighted standard template (MNI) by means of: a FSL package (http://www.fmrib.ox.ac.uk/fsl/) and b SPM8 (http://www.fil.ion.ucl.ac.uk/spm). The significant differences are found within the bilateral thalamus for both groups, whereas in the RR-MSc the neurodegenerative patterns involved also the putamen and the motor cortex bilaterally. RR-MSc: relapsing-remitting multiple sclerosis patients with cerebellar symptoms. RR-MSnc: relapsing–remitting multiple sclerosis patients without cerebellar symptoms
a Three-dimensional surface renders showing the significant clusters deriving from the comparison between RR-MSnc and RR-MSc groups. Specifically, the RR-MSc patients showed reduced GM volume in the bilateral superior temporal gyrus (STG) and in the right dorsolateral prefrontal cortex (DLPFC) with respect to RR-MSnc group. b Simple regression results. Scatter plots show the distribution of the mean GM volumes (y axis) and the cognitive scores (x axis), which resulted in being significantly correlated in the RR-MSc group. In particular, either SDMT or COWAT scores resulted in being positively correlated with the GM volume of the right DLPFC and left STG, respectively. The regression line (red) and the 95 % confidence intervals (black lines) are shown
Finally, regression analyses performed within RR-MSc group revealed a significant correlation between SDMT scores with GM volume in the right DLPFC (t value = 6.4, cluster (k) = 154, P FWE-corr = 0.03) and COWAT scores with GM volume in the left STG (t value = 5.81, cluster (k) = 331, P FWE-corr = 0.04)(Fig. 2b). Otherwise, within the RR-MSnc group, COWAT scores resulted in being correlated with the GM volume of the STG and inferior frontal cortex without reaching statistical threshold corrected for multiple comparisons. Correlating SDMT scores showed a significant relationship that was only detected with GM volume changes in the right superior parietal lobule (t value = 5.51, cluster (k) = 146, P FWE-corr = 0.04). No significant association was detected between EDSS scores and GM pathology in either MS group.
Although no significant differences in clinical factors were detected between groups, the RR-MSc group showed more heterogeneity in disease duration. For this reason, all previous analyses were re-analysed using disease duration scores as a covariate of no-interest. The overall pattern of findings remained the same.
Discussion
Our study provides the first evidence of distinct neurodegenerative processes characterizing the RR-MSc patients with respect to demographically, clinically, and radiologically matched RR-MSnc patients. Although both groups display a similar neurodegenerative pattern with respect to controls, confirming the involvement of the thalamus in the pathophysiological mechanisms of RR-MS [22, 25], the main finding is the detection of GM abnormalities when comparing MS groups between them. In fact, despite a similar clinical status, RR-MSc patients show significant atrophies in associative cortical areas that result to be consistent with the reported cognitive deficits in attention and language domains (Fig. 2b).
Crucial to the concept of a cognitive profile in the cerebellum is the existence of tight anatomical connections between the cerebellum and regions of the brain that support higher functions. Strong activation within the right posterior-lateral cerebellum has been described during several language paradigms, including word generation, semantic processing, phonological processing and verbal fluency task [26]. Moreover, agrammatism has been reported in patients with focal cerebellar lesions [27]. Apart from linguistic cognitive deficits, cerebellar lesions can give rise to the “ataxic dysarthria” that pertains to the motor aspect of speech. Indeed, the cerebellar dysarthria is mainly characterized by slowed tempo of spoken language [28]. All these findings are in agreement with our data where we demonstrated a decline of language abilities (verbal fluency) only in MS patients with cerebellar signs, which resulted in being correlated with GM loss in the superior temporal cortex. This latter finding confirms that the integrity of cerebellar-cortical loops might underlie poorer performance on measures of language functions in MS patients.
A similar interpretation might be proposed for the presence of poor performance during the SDMT in the RR-MSc group. The SDMT primarily assesses information processing speed, as well as sustained attention and working memory. Current knowledge of the neural networks involved in processing speed, attention and working memory suggests that these functions rely on the integrity of several cortical and subcortical structures distributed throughout the brain [29], mainly involving the cerebellum, the inferior/superior parietal lobules and the entire prefrontal cortex [30]. Generally, the vast majority of RR-MS patients reported deficits in attention/working memory as measured by SDMT, mainly in the early phase of disease [31], which resulted in being dependent upon the extension of pathology in the prefrontal cortex [12]. Indeed, Nocentini et al. [12] using VBM, demonstrated a strong correlation between loss of GM volume in the prefrontal cortex and lower performance during SDMT in RR-MS patients. This evidence would seem to confirm our results, where a similar relationship was detected in RR-MS patients having cerebellar signs. However, a significant correlation between SDMT performance and brain pathology within parietal cortex was also detected in RR-MSnc patients. This finding is unsurprising, because a very recent neuroimaging study demonstrated that MS’s performance during SDMT strongly rely on integrity of the white matter fiber tracts in the occipito-parietal cortex [32]. As concerns the specific role of the cerebellum, several neuroimaging studies proposed that the posterior part of the cerebellum represents part of the cortico-subcortical circuit that is involved in the articulatory control system [33, 34], which serves to sub-vocally refresh the contents of the phonological store during working memory. Following this evidence, our group demonstrated an altered cortico-cerebellar functional coupling in RR-MSc patients during a working memory task [13]. Furthermore, several studies highlighted the role of the cerebellum in attention processes. In particular, some authors proposed the cerebellum as a primate candidate for pathophysiological mechanisms underlying patients with attention-deficit hyperactivity disorders (ADHD), who are characterized by reduced cerebellar volumes [35]. Again, altered functional connectivity between the cerebellum and the DLPFC region was found in RR-MS patients during attention tasks [36].
However, the lack of cerebellar GM loss in the RR-MSc patients, who are characterized by evident white matter lesions within this region, poses important reflections. The cerebellum exhibits strong interconnections with the controlateral cerebral hemisphere either in feed-forward and feedback directions [6, 7]. Higher-order cerebral regions, such as the DLPFC, the parietal and the superior temporal cortices project to the cerebellum through the pontine nuclei [2–4]. Moreover, a recent VBM study [37] demonstrated that focal cerebellar lesions lead to both specific cognitive deficits (in attention, language and spatial memory domains) and atrophies in the frontal and temporal cortices, without loss of GM volume in the cerebellum. All these evidences strengthen the idea that the detected GM tissue loss in associative cortical areas, as well as the specific cognitive decline, may arise from Wallerian degeneration and diaschisis induced by cerebellar WM lesions characterizing the RR-MS patients with cerebellar symptoms. The demonstration of a discrepancy between GM/WM loss in the brain of MS patients with cerebellar symptoms is in line with the pathological description of cerebellar cortical demyelination associated with a relative axonal and neuronal preservation [38].
Some limitations of this study need to be discussed. First, we believe that our patient sample size and, consequently, small variability in the current clinical sample may have underpowered the ability to detect additional significant correlations between individual differences in the structural measures and clinical/cognitive scores. In fact, GM pathology is an important component of the MS-related disease process. Accelerated GM atrophy has been observed in MS patients [39], but its relationship to neurological disability remains elusive. Recent evidence demonstrated that the Multiple Sclerosis Functional Composite (MSFC) defined disability progression as more closely linked to brain atrophy than EDSS defined disability progression [40]. Future studies are needed to demonstrate the relevance of MSFC in prediction of GM pathology in MS patients with cerebellar signs.
In conclusion, our neuropsychological and neuroimaging data support the hypothesis, already raised by our previous studies [11, 13], that cerebellar symptoms may define a distinct clinical subtype being characterized by a more severe and widespread cortical pathology with respect to RR-MSnc patients. The confirmation of specific and selective cognitive deficits characterizing RR-MSc patients employing a different sample with respect to our previous studies [11, 13], represents a fundamental step for increasing our knowledge about the disease’s mechanisms and for improving treatments (i.e., cognitive rehabilitation)[41] that specifically target these MS-related symptoms.
References
Tedesco AM, Chiricozzi FR, Clausi S, Lupo M, Molinari M, Leggio MG (2011) The cerebellar cognitive profile. Brain 134:3669–3683
Schmahmann JD, Pandya DN (1989) Anatomical investigation of projections to the basis pontis from posterior parietal association cortices in rhesus monkey. J Comp Neurol 289:53–73
Middleton FA, Strick PL (2000) Basal ganglia and cerebellar loops: motor and cognitive circuits. Brain Res Brain Res Rev 31:236–250
Krienen FM, Buckner RL (2009) Segregated fronto-cerebellar circuits revealed by intrinsic functional connectivity. Cereb Cortex 19:2485–2497
Habas C, Kamdar N, Nguyen D, Prater K, Beckmann CF, Menon V, Greicius MD (2009) Distinct cerebellar contributions to intrinsic connectivity networks. J Neurosci 29:8586–8594
Schmahmann JD, Sherman JC (1998) The cerebellar cognitive and affective syndrome. Brain 121:561–579
Stoodley CJ, Schmahmann JD (2010) Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex 46:831–844
Bobholz JA, Rao SM (2003) Cognitive dysfunction in multiple sclerosis: a review of recent developments. Curr Opin Neurol 16:283–288
Amato MP, Zipoli V, Portaccio E (2006) Multiple sclerosis-related cognitive changes: a review of cross-sectional and longitudinal studies. J Neurol Sci 245:41–46
Rot U, Ledinek AH, Jazbec SS (2008) Clinical, magnetic resonance imaging, cerebrospinal fluid and electrophysiological characteristics of the earliest multiple sclerosis. Clin Neurol Neurosurg 110:233–238
Valentino P, Cerasa A, Chiriaco C, Nisticò R, Pirritano D, Gioia M, Lanza P, Canino M, Del Giudice F, Gallo O, Condino F, Torchia G, Quattrone A (2009) Cognitive deficits in multiple sclerosis patients with cerebellar symptoms. Mult Scler 15:854–859
Nocentini U, Bozzali M, Spanò B, Cercignani M, Serra L, Basile B, Mannu R, Caltagirone C, De Luca J (2012) Exploration of the relationships between regional grey matter atrophy and cognition in multiple sclerosis. Brain Imaging Behav [Epub ahead of print]. doi:10.1007/s11682-012-9170-7
Cerasa A, Passamonti L, Valentino P, Nisticò R, Pirritano D, Gioia MC, Chiriaco C, Mangone G, Perrotta P, Quattrone A (2012) Cerebellar-parietal dysfunctions in multiple sclerosis patients with cerebellar signs. Exp Neurol 237:418–426
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, Lublin FD, Metz LM, McFarland HF, O’Connor PW, Sandberg-Wollheim M, Thompson AJ, Weinshenker BG, Wolinsky JS (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria” [review]. Ann Neurol 58:840–846
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452
Steinberg M (1994) Interviewers guide to the structured clinical interview for DSM-IV disorders (SCID). American Psychiatric Press, Washington
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46:1121–1123
Gioia MC, Cerasa A, Liguori M, Passamonti L, Condino F, Vercillo L, Valentino P, Clodomiro A, Quattrone A, Fera F (2007) Impact of individual cognitive profile on visuo-motor reorganization in relapsing–remitting multiple sclerosis. Brain Res 1167:71–79
Cerasa A, Fera F, Gioia MC, Liguori M, Passamonti L, Nicoletti G, Vercillo L, Paolillo A, Clodomiro A, Valentino P, Quattrone A (2006) Adaptive cortical changes and the functional correlates of visuo-motor integration in relapsing–remitting multiple sclerosis. Brain Res Bull 69:597–605
Cerasa A, Bilotta E, Augimeri A, Cherubini A, Pantano P, Zito G, Lanza P, Valentino P, Gioia MC, Quattrone A (2012) A cellular neural network methodology for the automated segmentation of multiple sclerosis lesions. J Neurosci Method 203:193–199
Ashburner J (2007) A fast diffeomorphic image registration algorithm. Neuroimage 38:95–113
Mesaros S, Rocca MA, Absinta M, Ghezzi A, Milani N, Moiola L, Veggiotti P, Comi G, Filippi M (2008) Evidence of thalamic gray matter loss in pediatric multiple sclerosis. Neurology 70:1107–1112
Fischl B, Dale AM (2000) Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci USA 97:11050–11055
Cerasa A, Messina D, Nicoletti G, Novellino F, Lanza P, Condino F, Arabia G, Salsone M, Quattrone A (2009) Cerebellar atrophy in essential tremor using an automated segmentation method. Am J Neuroradiol 30:1240–1243
Ceccarelli A, Rocca MA, Pagani E, Colombo B, Martinelli V, Comi G, Filippi MA (2008) A voxel-based morphometry study of grey matter loss in MS patients with different clinical phenotypes. Neuroimage 42:315–322
Stoodley CJ (2012) The cerebellum and cognition: evidence from functional imaging studies. Cerebellum 11:352–365
Fabbro F, Tavano A, Corti S, Bresolin N, De Fabritiis P, Borgatti R (2004) Long-term neuropsychological deficits after cerebellar infarctions in two young adult twins. Neuropsychologia 42:536–545
Ackermann H, Mathiak K, Riecker A (2007) The contribution of the cerebellum to speech production and speech perception: clinical and functional imaging data. Cerebellum 6:202–213
Stoodley CJ, Schmahmann JD (2009) Functional topography in the human cerebellum: a meta-analysis of neuroimaging studies. Neuroimage 44:489–501
Lazeron RH, Rombouts SA, de Sonneville L, Barkhof F, Scheltens P (2003) A paced visual serial addition test for fMRI. J Neurol Sci 213:29–34
Deloire MS, Salort E, Bonnet M, Arimone Y, Boudineau M, Amieva H, Barroso B, Ouallet JC, Pachai C, Galliaud E, Petry KG, Dousset V, Fabrigoule C, Brochet B (2005) Cognitive impairment as marker of diffuse brain abnormalities in early relapsing remitting multiple sclerosis. J Neurol Neurosurg Psychiatry 76:519–526
Rossi F, Giorgio A, Battaglini M, Stromillo ML, Portaccio E, Goretti B, Federico A, Hakiki B, Amato MP, De Stefano N (2012) Relevance of brain lesion location to cognition in relapsing multiple sclerosis. PLoS ONE 7:e44826. doi:10.1371/journal.pone.0044826
Chen SH, Desmond JE (2005) Cerebrocerebellar networks during articulatory rehearsal and verbal working memory tasks. Neuroimage 24:332–338
Desmond JE, Chen SH, De Rosa E, Pryor MR, Pfefferbaum A, Sullivan EV (2003) Increased frontocerebellar activation in alcoholics during verbal working memory: an fMRI study. Neuroimage 19:1510–1520
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, Blumenthal JD, James RS, Ebens CL, Walter JM, Zijdenbos A, Evans AC, Giedd JN, Rapoport JL (2002) Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA 288:1740–1748
Bonnet MC, Allard M, Dilharreguy B, Deloire M, Petry KG, Brochet B (2010) Cognitive compensation failure in multiple sclerosis. Neurology 75:1241–1248
Clausi S, Bozzali M, Leggio MG, Di Paola M, Hagberg GE, Caltagirone C, Molinari M (2009) Quantification of gray matter changes in the cerebral cortex after isolated cerebellar damage: a voxel-based morphometry study. Neuroscience 162:827–835
Kutzelnigg A, Faber-Rod JC, Bauer J, Lucchinetti CF, Sorensen PS, Laursen H, Stadelmann C, Brück W, Rauschka H, Schmidbauer M, Lassmann H (2007) Widespread demyelination in the cerebellar cortex in multiple sclerosis. Brain Pathol 17:38–44
Chard DT, Griffin CM, Rashid W, Davies GR, Altmann DR, Kapoor R, Barker GJ, Thompson AJ, Miller DH (2004) Progressive grey matter atrophy in clinically early relapsing–remitting multiple sclerosis. Mult Scler 10:387–391
Rudick RA, Lee JC, Nakamura K, Fisher E (2009) Gray matter atrophy correlates with MS disability progression measured with MSFC but not EDSS. J Neurol Sci 282:106–111
Cerasa A, Gioia MC, Valentino P, Nisticò R, Chiriaco C, Pirritano D, Tomaiuolo F, Mangone G, Trotta M, Talarico T, Bilotti G, Quattrone A (2012) Computer-assisted cognitive rehabilitation of attention deficits for multiple sclerosis: a randomized trial with fMRI correlates. Neurorehabil Neural Repair doi:10.1177/1545968312465194
Acknowledgements
This study has been supported by FISM—Fondazione Italiana Sclerosi Multipla—Cod. 2010/R/11.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cerasa, A., Valentino, P., Chiriaco, C. et al. MR imaging and cognitive correlates of relapsing–remitting multiple sclerosis patients with cerebellar symptoms. J Neurol 260, 1358–1366 (2013). https://doi.org/10.1007/s00415-012-6805-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6805-y