Abstract
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease that imposes a great burden on the patient, the patient's family and society. However, we lack information about the total disease burden at a national level, especially regarding costs before and after diagnosis and the consequences for spouses. We aimed to estimate the factual direct and indirect costs of ALS in a national sample. Using records from the Danish National Patient Registry (1998–2009), 2,394 patients with ALS were identified and subsequently compared with 9,575 randomly chosen control subjects matched for age, gender and geographic area/civil status. Direct costs, including frequencies of primary and sector contacts and procedures, and medication from primary and secondary sectors, were obtained from the Danish Ministry of Health, the Danish Medicines Agency, and the National Health Security. Indirect costs included labour supply and social transfer payments, and were based on income data derived from Coherent Social Statistics. Patients with a diagnosis of ALS had poor survival. The average (95 % CI) 5-year survival rate was 0.278 (0.358–0.298) compared with 0.865 (0.858–0.872) among controls. Patients with ALS had significantly higher rates of health-related contact and medication use and higher socioeconomic costs. They also had very low employment rates, while those in employment had a lower income level than control subjects. The annual mean excess health-related cost was €18,918 for each ALS patient. However, spouses showed no excess health usage; in fact, their employment and income rates were higher, and the net cost was reduced by −€3,420. We conclude that ALS has serious mortality, health and socioeconomic consequences for patients. However, the consequences for spouses are complex; they tend to compensate for the social consequences to patients by increasing their net income after ALS diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease characterized by progressive degeneration of motor neurons, leading to muscular atrophy, paralysis and death in 3–5 years from the first appearance of symptoms. ALS is familiar in about 10 % of cases and mutations of the copper–zinc superoxide dismutase 1 (SOD1) enzyme are found in a significant percentage of these cases. Furthermore mutations of the copper–zinc superoxide dismutase 1 (SOD1) enzyme [25] and the gene C9ORF72 [6] is identified in sporadic and familiar cases and are found in a significant percentage of these cases.
Significant progress has been made towards understanding the underlying pathophysiology, improving diagnostic accuracy, and managing this disorder. The pathological disease process is characterized by the progressive destruction of the spinal cord and cortical motor neurons. Future advances are expected to further our understanding of the brain processes underlying the disease. No intervention is currently possible that reduces the severity of the disease and its associated mortality.
Because of its severity, ALS causes significant morbidity and mortality, imposing a major burden on the patient, their family and society, with respect to heath care use, loss of work capabilities [7–9, 16, 17, 24, 27, 30] and caregiving [19, 26].
ALS places a significant burden on caregivers due to resulting limitations, depression and anxiety [26]. However, there are limited data on the factual consequences of ALS on patient health usage, work capability and partners. As the mortality rate is significant, it should be taken into account in the analysis of the burden of disease.
In Denmark, it is possible to calculate health sector costs and productivity losses related to diseases from public and private hospitals and clinics in the primary and secondary sector—including medication, social factors, income, and employment data from all patients—is registered in central databases. The effect of the disease can therefore be estimated before, at, and after diagnosis. We undertook the current study to evaluate the socioeconomic consequences of ALS for patients, their partners, and society, as determined in a national population-based study.
Methods
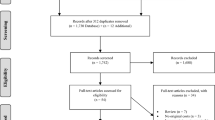
In Denmark, all hospital contacts are recorded in the National Patient Registry (NPR) in terms of the time of contact and information about primary and secondary diagnoses. The NPR includes administrative information, diagnoses, and diagnostic and treatment procedures using several international classification systems, including the International Classification of Disorders (ICD-10). The NPR is a time-based national database that includes data from all inpatient and outpatient contacts, so the data that we extracted are representative of all patients in Denmark who have received a diagnosis of ALS in the primary or secondary sector in public and private hospitals. As data are available throughout the observation period, we can trace patients retrospectively and prospectively relative to the time of their diagnosis. All contacts in the primary sector (general practice and specialist care in the primary sector) and the use of medications are recorded in the databases of the National Health Security and the Danish Medicine Agency, respectively. There is some underestimation of numbers of patients with chronic diseases, as those with a contact in the primary sector but not in the secondary sector are recorded as having had contact but not as having had a diagnosis. However, for a potentially harmful disease like ALS this effect is minimal, as almost all patients are recorded by the hospital system.
The economic consequences of ALS for patients and their partners were estimated by determining the yearly cost of illness per patient diagnosed with ALS (ICD DG122), and comparing that figure with the cost of healthcare in a matched control group. The health cost was then apportioned to annual health sector costs and productivity.
Direct costs included those of hospitalization and outpatient cost, weighted by use, for separate diagnosis-related groups, and specific outpatient costs (DRG tariffs). These costs were all based on data from the Danish Ministry of Health. The use and costs of drugs were derived from data from the National Danish Medicine Agency, consisting of the retail price of each drug (including dispensing costs) multiplied by the number of transactions. The frequencies and costs of consultations with general practitioners and other specialists were based on data from the Danish National Health Security.
Productivity losses because of a reduced labour supply related to diseases comprise income derived from state coffers. Also, all social transfer incomes were measured, including subsistence allowances, pensions, social security, social assistance, publicly funded personal support for education, and others. Productivity losses and social transfer incomes were based on income figures from Coherent Social Statistics.
Cost-of-illness studies measure the economic burden resulting from disease and illness across a defined population. Costs are the value of resources used in the treatment, care, and rehabilitation of people with the condition under study. Productivity losses represent the value of economic resources lost because of disease-related work disability or premature mortality. As patients leave the national data registers at the time of death, the indirect costs estimate comprises only the production loss related to disease-related work disability. It is important to distinguish costs from monetary transfer payments such as disability and welfare payments. These payments represent a transfer of purchasing power to the recipients from the general taxpayers, but do not represent net increases in the use of resources and, therefore, are not included in the total cost estimate.
By reviewing the NPR, we identified all patients who received a first diagnosis of ALS from 1998 to 2009 (excluding ALS cases prior to 1997). Then, using data from the Civil Registration System Statistics Denmark database (which includes information about all social factors, incomes, pensions, etc.), we randomly selected citizens of the same age and sex as the patients. Social compensation was achieved by selecting control subjects of the same civil status who resided in the same area of the country as the patients. The ratio of control subjects to patients was 4:1. Data from patients and matched control subjects who could not be identified in the Coherent Social Statistics database were excluded from the sample. More than 99 % of the observations in the two groups were successfully matched. Patients and matched control subjects were followed from the year of diagnosis until 2009. If a patient or control was not present in the CPR register on January 1st each year, then the corresponding control or patient control was not included in the dataset for that year. Patients who are not in the CPR register are typically deceased, in prison, or have emigrated to another country. All patients’ partners (married or non-married, irrespective of gender) were identified. A similar control group of partners was identified on the basis of age, gender and socio-demographic status.
Costs were measured on a yearly basis and adjusted to 2009 prices using the health sector price index for health sector costs; the general price index was applied to nonmedical costs. All costs were measured in DKK and converted to Euros (€1: DKK 7.45).
The study was approved by the Danish Data Protection Agency. Data were handled in a manner that did not reveal the identity of any patients or control subjects, so neither individual nor ethical approval was required. Statistical analysis was performed using SAS 9.1.3 (SAS, Inc., Cary, NC). Statistical significance of the cost estimates was assessed by nonparametric bootstrap analysis (33).
Results
In total, 2,394 patients with ALS were identified and subsequently matched with 9,575 control subjects. The age distribution of the patients and control subjects is shown in Table 1. Overall, 54.9 % were male, and 63.6 % of the patients were married or cohabiting compared with 63.0 % of the controls subjects (not significant).
Survival in patients with ALS compared with controls
Patients with a diagnosis had a significantly lower survival rate than age-, gender- and demographically matched controls. The mean (95 % confidence interval) survival rate (fraction of 1) was 0.356 (0.336–0.376) versus 0.924 (0.918–0.929) at 3 years, 0.278 (0.358–0.298) versus 0.865 (0.858–0.872) at 5 years, and 0.203 (0.182–0.224) versus 0.711 (0.698–0.724) at 10 years (p < 0.0001 in each comparison).
Direct costs: outpatient clinic, hospital, primary care, and drug costs
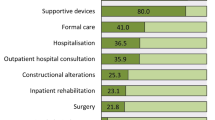
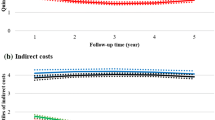
More patients than control subjects were treated in outpatient clinics, were hospitalized, used medication and had contact with the primary care system (Table 2, Fig. 1). The total health cost increased significantly at time of diagnosis, but decreased thereafter (Fig. 2). Patients’ partners did not have higher rates of inpatient or outpatient treatment than control subjects’ partners, but did make slightly less frequent use of healthcare services and medication (Table 3, Fig. 1).
Indirect costs, social costs, employment rate, and income
Fewer patients than controls had income from employment and more often received public transfer income after an ALS diagnosis (Table 2). The employment rate for patients was significantly slightly lower before diagnosis and decreased significantly over time following their diagnosis of ALS (Fig. 1). After the ALS diagnosis, the corresponding income from employment decreased and the public transfer income accordingly increased (Fig. 1). Patients’ partners, by contrast, had a higher employment rate, earned more income from employment and received public transfer income less often after the patient’s diagnosis (Table 3, Fig. 1).
Total annual costs
The sources of information and the average annual healthcare cost per person-year by cost category for patients with ALS in Denmark compared with age- and sex-matched control subjects are presented in Table 4; the corresponding figures for their partners are shown in Table 5. The patients’ total cost was greater prior to an ALS diagnosis, while after diagnosis the net sum of direct net healthcare costs (general practitioner services, hospital services, and medication) and productivity losses (loss of labor market income) were €18,918 for patients with ALS and −€3,420 for their partners compared with controls. In other words, patients’ partners higher income than those of the control group due to a higher employment rate, and also lower social transfer payments.
Influence of age and sex on employment and direct and indirect costs
Male patients and controls had higher incomes than their female counterparts. Age and sex were markedly associated with direct costs, especially with respect to higher expenses due to hospitalization and medication among younger patients, whereas direct and indirect costs were higher among elderly patients, due to increased indirect costs (Fig. 3).
Discussion
The study illustrates several serious consequences of ALS. The mortality is high and patients had significantly higher rates of contact with all sectors of the healthcare system (general practice, outpatient clinics, and in-hospital services). Patients had higher rates of medication use, other treatment devices, and of publicly supported payment for medication. Total costs were higher in the group of patients with ALS than in age- and sex-matched control subjects. Patients with ALS also had lower employment rates and received welfare payments significantly more often; employed patients had lower incomes than employed control subjects. ALS did not cause increased health care use among partners, and partner’s level of income increased. Consequently, the health care costs and the productivity losses were lower for partners of ALS patients (compared to controls). The study demonstrates that ALS has social and economic consequences even before a diagnosis has been established. Thus, ALS has socioeconomic and morbidity impacts on patients, partners and society. However, the health costs reduce over time, probably due to selection, since the reduction in health care costs follows the mortality rate of ALS patients. Use of medication and non-invasive and invasive ventilation are included in the analysis, but have not been evaluated separately. Additional cost analysis to helpers in subgroups of patients treated with invasive ventilator treatment or specific anti-ALS medical treatment needs further analysis.
The presence of a serious, chronic disease like ALS affects partners of patients in several ways: social decline, psychological effects, and a heavier workload [3]. Patients’ neurobehavioral symptoms were related to lower caregivers’ quality of life, depression, and burden [3]. However, we found that ALS is one of the first diseases in which we have found that spouses make less use of health and social services and have a higher income. We believe that such a pattern is specific to a disease like ALS, whereby a healthy partner tends to compensate for the patient’s serious health-related and social decline by increasing their workload. The increasing income among spouses might be explained by a need to maintain a target income for the family after a drop in labour market income among the patients. Another hypothesis could be that the municipalities provide more home care after diagnosis so spouses have more time to join the labour market (diagnosis is often used as a gatekeeping to municipal services), but the data from the municipalities have not sufficient quality to control for that. We have not evaluated the consequences for families with children with ALS; further subgroup analysis of this aspect is needed.
Previous studies examining the burden of ALS have focused on the direct costs, e.g., hospital services and use of treatment procedures, such as medication, surgical intervention, non-invasive ventilation, physiotherapy, the reduction in quality of life [11, 15, 16, 28, 31], and the burden on caregivers [4, 10, 18–20, 26, 29]. There are currently limited data whatsoever regarding the total cost benefit or cost effectiveness of treatment on direct or indirect costs, including education, familial, and societal consequences.
The impact of ALS is considerable. As can be seen in Figs. 1 and 4, even by the time of diagnosis, patients had already experienced significant reductions in their levels of employment. The employment rate was affected before a diagnosis of ALS had been made, and fell even further once it was confirmed. This pattern has been described in other chronic and progressive disorders, such as multiple sclerosis [13], parkinsonism [14] and sleep-disordered breathing [12], but the effect is considerable in the case of ALS due to it serious effect on morbidity. We have not calculated the effect of loss of active years due to increased mortality. We have included all types of treatments including medication and uses of non-invasive ventilation, but not evaluated subtypes of treatment or services provided for municipalities [1, 2, 5, 11, 22, 23].
The current study considered all patients who had received a diagnosis of ALS. In Denmark, most ALS patients have contact with neurological departments and are, therefore, registered. Because of the severity of the disease, no or only few patients are in primary care, and the number identified probably comprises all ALS patients who are in the observation period. Former studies of the registration procedure suggests that 85–90 % of registrations in the NPR are correct [21]. Incorrect diagnoses are due to incorrect registration, variation in the registration procedure, or in diagnostic criteria. As all Danes are registered in national databases using social security codes, including data concerning health (diagnostic and treatment procedures in primary and secondary sector), medication, social factors, and employment are recorded.
The control group was not defined as a group of healthy subjects, rather, they were selected on the basis of age, sex, geography, and social factors. To be included as control subjects they could not have a diagnosis of ALS, but they may very well have had other illnesses. The differences observed between patients and control subjects thus represent those between people with ALS and a random population-based sample.
Consequently, the study presents the objectively determined direct and indirect costs of ALS that were evaluated in a national sample, compared with a control group with a similar age, sex, and social composition, over a 12-year period.
In conclusion, ALS leads to high mortality, higher health-related and social transfer costs, and lower levels of employment and income. The partners of ALS patients are involved in a different way from what has been observed in other neurological diseases: they tend to compensate by taking on a greater workload, and consequently have a higher income. Additional research is needed to evaluate the effects of specific interventions on morbidity, mortality, costs and families.
References
Bromberg MB, Brownell AA, Forshew DA, Swenson M (2010) A timeline for predicting durable medical equipment needs and interventions for amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler 11:110–115
Cazzolli PA, Oppenheimer EA (1996) Home mechanical ventilation for amyotrophic lateral sclerosis: nasal compared to tracheostomy-intermittent positive pressure ventilation. J Neurol Sci 139(Suppl):123–128
Chio A, Vignola A, Mastro E, Giudici AD, Iazzolino B, Calvo A, Moglia C, Montuschi A (2010) Neurobehavioral symptoms in ALS are negatively related to caregivers’ burden and quality of life. Eur J Neurol 17:1298–1303
Chio A, Vignola A, Mastro E, Giudici AD, Iazzolino B, Calvo A, Moglia C, Montuschi A (2010) Neurobehavioral symptoms in ALS are negatively related to caregivers’ burden and quality of life. Eur J Neurol 17:1298–1303
De Vito EL, Suarez AA, Monteiro SG (2012) The use of full-setting non-invasive ventilation in the home care of people with amyotrophic lateral sclerosis-motor neuron disease with end-stage respiratory muscle failure: a case series. J Med Case Reports 6:42
Dejesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, Nicholson AM, Finch NA, Flynn H, Adamson J, Kouri N, Wojtas A, Sengdy P, Hsiung GY, Karydas A, Seeley WW, Josephs KA, Coppola G, Geschwind DH, Wszolek ZK, Feldman H, Knopman DS, Petersen RC, Miller BL, Dickson DW, Boylan KB, Graff-Radford NR, Rademakers R (2011) Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron 72:245–256
Elman LB, Stanley L, Gibbons P, McCluskey L (2006) A cost comparison of hospice care in amyotrophic lateral sclerosis and lung cancer. Am J Hosp Palliat Care 23:212–216
Ginsberg G, Lowe S (2002) Cost effectiveness of treatments for amyotrophic lateral sclerosis: a review of the literature. Pharmacoeconomics 20:367–387
Ginsberg GM, Lev B (1997) Cost-benefit analysis of riluzole for the treatment of amyotrophic lateral sclerosis. Pharmacoeconomics 12:578–584
Goldstein LH, Atkins L, Landau S, Brown R, Leigh PN (2006) Predictors of psychological distress in carers of people with amyotrophic lateral sclerosis: a longitudinal study. Psychol Med 36:865–875
Gruis KL, Chernew ME, Brown DL (2005) The cost-effectiveness of early noninvasive ventilation for ALS patients. BMC Health Serv Res 5:58
Jennum P, Kjellberg J (2011) Health, social and economical consequences of sleep-disordered breathing: a controlled national study. Thorax 66:560–566
Jennum P, Wanscher B, Frederiksen J, Kjellberg J (2011) The socioeconomic consequences of multiple sclerosis: A controlled national study. Eur Neuropsychopharmacol 22:36–43
Jennum P, Zoetmulder M, Korbo L, Kjellberg J (2011) The health-related, social, and economic consequences of parkinsonism: a controlled national study. J Neurol 258:1497–1506
Lechtzin N, Wiener CM, Clawson L, Chaudhry V, Diette GB (2001) Hospitalization in amyotrophic lateral sclerosis: causes, costs, and outcomes. Neurology 56:753–757
Lopez-Bastida J, Perestelo-Perez L, Monton-Alvarez F, Serrano-Aguilar P, Alfonso-Sanchez JL (2009) Social economic costs and health-related quality of life in patients with amyotrophic lateral sclerosis in Spain. Amyotroph Lateral Scler 10:237–243
Messori A, Trippoli S, Becagli P, Zaccara G (1999) Cost effectiveness of riluzole in amyotrophic lateral sclerosis. Italian Cooperative Group for the Study of Meta-Analysis and the Osservatorio SIFO sui Farmaci. Pharmacoeconomics 16:153–163
Mitsumoto H, Rabkin JG (2007) Palliative care for patients with amyotrophic lateral sclerosis: “prepare for the worst and hope for the best”. JAMA 298:207–216
Miyashita M, Narita Y, Sakamoto A, Kawada N, Akiyama M, Kayama M, Suzukamo Y, Fukuhara S (2009) Care burden and depression in caregivers caring for patients with intractable neurological diseases at home in Japan. J Neurol Sci 276:148–152
Miyashita M, Yamaguchi A, Kayama M, Narita Y, Kawada N, Akiyama M, Hagiwara A, Suzukamo Y, Fukuhara S (2006) Validation of the Burden Index of Caregivers (BIC), a multidimensional short care burden scale from Japan. Health Qual Life Outcomes 4:52
Mosbech J, Jorgensen J, Madsen M, Rostgaard K, Thornberg K, Poulsen TD (1995) The national patient registry. Evaluation of data quality. Ugeskr Laeger 157:3741–3745
Moss AH, Oppenheimer EA, Casey P, Cazzolli PA, Roos RP, Stocking CB, Siegler M (1996) Patients with amyotrophic lateral sclerosis receiving long-term mechanical ventilation. Advance care planning and outcomes. Chest 110:249–255
Narayanaswami P, Bertorini TE, Pourmand R, Horner LH (2000) Long-term tracheostomy ventilation in neuromuscular diseases: patient acceptance and quality of life. Neurorehabil Neural Repair 14:135–139
Ng L, Talman P, Khan F (2011) Motor neurone disease: disability profile and service needs in an Australian cohort. Int J Rehabil Res 34:151–159
Orrell RW (2010) Motor neuron disease: systematic reviews of treatment for ALS and SMA. Br Med Bull 93:145–159
Pagnini F, Rossi G, Lunetta C, Banfi P, Castelnuovo G, Corbo M, Molinari E (2010) Burden, depression, and anxiety in caregivers of people with amyotrophic lateral sclerosis. Psychol Health Med 15:685–693
Schepelmann K, Winter Y, Spottke AE, Claus D, Grothe C, Schroder R, Heuss D, Vielhaber S, Mylius V, Kiefer R, Schrank B, Oertel WH, Dodel R (2010) Socioeconomic burden of amyotrophic lateral sclerosis, myasthenia gravis and facioscapulohumeral muscular dystrophy. J Neurol 257:15–23
Tavakoli M, Malek M (2001) The cost utility analysis of riluzole for the treatment of amyotrophic lateral sclerosis in the UK. J Neurol Sci 191:95–102
van Teijlingen ER, Friend E, Kamal AD (2001) Service use and needs of people with motor neurone disease and their carers in Scotland. Health Soc Care Community 9:397–403
Van Der Steen I, Van Den Berg JP, Buskens E, Lindeman E, Van Den Berg LH (2009) The costs of amyotrophic lateral sclerosis, according to type of care. Amyotroph Lateral Scler 10:27–34
Ward AL, Sanjak M, Duffy K, Bravver E, Williams N, Nichols M, Brooks BR (2010) Power wheelchair prescription, utilization, satisfaction, and cost for patients with amyotrophic lateral sclerosis: preliminary data for evidence-based guidelines. Arch Phys Med Rehabil 91:268–272
Acknowledgment
The study is a part of a larger database study supported from several public funds with the purpose of identifying the burden of neurological diseases.
Conflicts of interest
There are no conflicts of interests among the authors.
Ethical standard
All human studies have been approved by the appropiate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helinski.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jennum, P., Ibsen, R., Pedersen, S.W. et al. Mortality, health, social and economic consequences of amyotrophic lateral sclerosis: a controlled national study. J Neurol 260, 785–793 (2013). https://doi.org/10.1007/s00415-012-6706-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6706-0