Abstract
With an aging population, patients are increasingly likely to present with stroke and pre-existing dementia, which may lead to greater death and disability. The aim of this work was to assess the risk of all-cause mortality and poor functional outcomes after ischemic stroke in patients with and without pre-existing dementia. We conducted a multicenter cohort study of all patients presenting to 12 tertiary care institutions participating in the Registry of the Canadian Stroke Network (RCSN) with a first ischemic stroke between 2003 and 2008. Individuals with pre-existing dementia were matched using propensity-score methods with patients without dementia during their index hospitalization based on the following characteristics: age (within 3 years), sex, stroke severity, stroke subtype (lacunar vs. non-lacunar), level of consciousness, vascular risk factors, dysphagia, glucose and creatinine on admission, Charlson index, residence prior to hospitalization (home vs. other), pre-admission dependency, hospital arrival via ambulance, admission to stroke unit, thrombolysis, and palliative care. A propensity score for all-cause mortality and clinical outcomes was developed. Registry of the Canadian Stroke Network (RCSN) and Registered Persons Database (RPDB). The primary outcome was all-cause mortality at 30 days. Secondary outcomes included mortality at discharge and at 1 year, disability at discharge (modified Rankin scale ≥ 3), medical complications (pneumonia), and discharge disposition. A subgroup analysis assessing the risk of intracerebral hemorrhage among those receiving thrombolysis was also conducted. We matched 877 patients with an acute ischemic stroke and pre-existing dementia to 877 stroke patients without dementia. Patients were well matched. The mean age was 82 years and 58 % were women. Mortality at discharge, 30 days, and 1 year after stroke was similar in patients with and without dementia [for mortality at discharge RR 0.88 [95 % confidence interval (CI) 0.74–1.05]; mortality at 30-days: RR 0.88 (95 % CI 0.75–1.03) and mortality at 1 year: RR 1.01 (95 % CI 0.92–1.11). Patients with pre-existing dementia had similar disability at discharge and home disposition. In the subgroup of patients who received thrombolysis, there were no differences between those with and without dementia in the risk of intracerebral hemorrhage (RR 1.27; 95 % CI 0.69–2.35) and no differences in mortality or disability at discharge. Pre-existing dementia is not independently associated with mortality, disability, or institutionalization after ischemic stroke. Pre-existing dementia may not necessarily preclude access to thrombolytic therapy and specialized stroke care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a devastating medical condition, whose effects may be compounded by pre-existing dementia. The risk of stroke and dementia both increase with age, and, over the next several decades, a greater number of clinicians and caregivers are expected to face the challenge of both conditions presenting together [1–5].
In Canada, over one-third of patients hospitalized for an acute ischemic stroke are 80 years of age or older [2]. According to a recent report, the worldwide costs of dementia will exceed 1 % of global gross domestic product in 2010, estimated at 604 billion USD in physician services, hospital costs, lost wages, and decreased productivity [6, 7].
Previous studies suggest that dementia may be a determinant of both death and poor functional outcomes after stroke [8, 9]. As a result, different paradigms of care (comprehensive assessment vs. case-by-case-based approach) for stroke patients with dementia have been under intense debate [10, 11]. Access to specialized stroke care (i.e., stroke unit admission, thrombolysis, stroke team assessment) is considered crucial in the provision of a high quality of care. On the other hand, there may be an inclination to minimize interventions in older patients with pre-existing dementia, especially if these interventions are not likely to substantially alter outcomes [2], and some studies have reported reduced use of coronary care units, neuroimaging, antibiotics, and feeding tubes in stroke patients with dementia [10, 12]. Organized inpatient stroke care including stroke unit admission and use of thrombolysis can reduce death and disability irrespective of age, stroke severity, and subtype [15–17]. However, it is not clear whether these benefits extend to patients with pre-existing dementia.
Unfortunately, there is little reliable information on whether dementia in itself is associated with an increased incident risk of death and dependency after an acute ischemic stroke.
In this study, our aims were to: (1) determine if pre-existing dementia is an independent predictor of all-cause mortality and disability after ischemic stroke, and (2) to conduct a subgroup analysis to evaluate clinical outcomes after thrombolytic therapy in matched cohorts of ischemic stroke patients with and without dementia.
Participants and methods
We conducted a retrospective, observational study, using the Registry of the Canadian Stroke Network (RCSN), a clinical database that includes patients who have experienced an acute stroke and admitted to participating institutions [18].
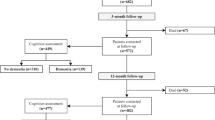
Participants were eligible if they were older than 18 years and admitted to any of 12 regional stroke centers in one of the largest province (Ontario) in Canada with a first acute ischemic stroke between July 2003 and September 2008 (see patient flow chart–supplemental file). Patients with transient ischemic attacks or hemorrhagic strokes were not included in this study since they have different underlying mechanisms, risk factors, and prognosis.
The RCSN, was established in 2001, with over 40,000 patients accrued. In its current phase, data are collected on all consecutive patients with stroke or transient ischemic attack seen in the emergency room or admitted to any of 12 participating stroke centers. The goal of the RCSN is to measure and monitor the quality of hospital stroke care delivery. Clinical data was collected at admission and discharge by neurology research nurses using chart abstraction. Details of the methodology used by the RCSN (www.rcsn.org), data quality and the definitions have been well described in previous publications [2]. All facilities included in this study are considered comprehensive or primary stroke centers as per the recommendations from the Brain Attack Coalition [19].
Baseline characteristics
Demographic characteristics, marital status, living status, and comorbid conditions were available through the RCSN. Stroke severity was assessed on admission using the validated Canadian Neurological Scale (CNS); higher scores using this scale indicate lower severity [20, 21]. Stroke severity was categorized as: mild (CNS > 8), moderate (CNS 5–7), or severe (CNS < 4). Patients were classified as either being admitted to a general ward or a stroke unit, defined as a designated ward where stroke care was provided by a multidisciplinary team. Ischemic stroke subtype was classified as small vessel disease, cardioembolic, large artery atherosclerotic disease, or undetermined based on documentation by the treating physician and the investigations recorded in the chart [2]. Patients who were able to complete all activities of daily living in the 3 months prior to the stroke event were classified as independent. Place of residence prior to admission was classified as home, rehabilitation facility, nursing home, retirement home, or undetermined (n = 27; 0.3 %).
Data quality
Chart validation studies have shown good to excellent agreement with the RCSN database, with kappa scores of >0.8 for key variables (age, sex, stroke type, thrombolysis use, comorbid conditions) (RCSN report; www.rcsn.org) [18].
Ethics and patient consent
Ethics approval was obtained from the St. Michael’s Hospital institutional review board. The RCSN has the designation of a “prescribed registry”, thereby allowing the collection of patient-level information without consent for the purpose of facilitating the provision of stroke care in Ontario.
Definition of dementia
Pre-existing dementia was defined as any type of dementia (degenerative, vascular, mixed) that was identified prior to the index stroke. It includes a chronic loss of mental function or slow, progressive, mental decline for at least 1 month, identified from clinical records, history/physical examination, or on the physician’s admission notes.
Outcome measures
The primary outcome measure was all-cause mortality at 30 days.
Secondary outcomes included death at discharge and at 1 year, disability at discharge, pneumonia, and discharge disposition. Disability at discharge was assessed using the modified Rankin scale (mRS ≥ 3). Stroke-associated pneumonia required radiographic confirmation and development within the first 30 days after stroke.
A pre-specified subgroup analysis was conducted to determine death, disability, and the risk of intracerebral hemorrhage (ICH) for those receiving thrombolysis among those with and without dementia.
Analytical approach
Chi-square tests were used to compare categorical variables; ANOVA or Kruskal–Wallis tests were used to compare mean and median differences for continuous variables in baseline characteristics.
To account for differences in baseline characteristics, we used propensity-score methods to match patients with pre-existing dementia to those patients without pre-existing dementia [22, 23]. This approach would allow determining whether pre-existing dementia is an independent predictor of outcomes, or alternatively the associated comorbidities explained the poorer outcomes in these patients. The clinical variables of interest that were used in the propensity-score model were age, sex, stroke severity, stroke subtype (lacunar vs. other), hypertension, diabetes, hyperlipidemia, atrial fibrillation, previous stroke or TIA, level of consciousness on arrival, dysphagia, glucose and creatinine levels on admission, arrival to hospital from a residence (home vs. other), pre-admission dependency, palliative care, stroke unit admission, thrombolysis, physiotherapy, and arrival by ambulance. A matching algorithm was then used to match patients with pre-existing dementia and those without dementia within a caliper of 0.2 standard deviations of the logit of the propensity score, with matching ratio of 1:1. To determine whether the propensity-score approach achieved balance in potential confounders, we compared the proportions of each covariate considered in the multivariable risk adjustment model between patients with and without dementia [22]. Evidence of imbalance in potential confounders was identified by examining the reduction in absolute standardized differences (Tables 1, 2). Adequate balance was defined as a standardized difference less than 0.1 [24].
For all-cause mortality, 877 patients with pre-existing dementia were matched with 877 patients without dementia. Differences in baseline characteristics after matching are shown in Table 1.
For the analysis of outcomes after thrombolytic therapy (n = 1,668 including 101 patients with pre-existing dementia), there were 99 patients with dementia matched with 99 patients without dementia. Differences in baseline characteristics are presented in Table 2.
In the final propensity-score matched sample, paired t test (continuous variables) and McNemar test (binary variables) were used to compare outcomes. We calculated the adjusted RR in the original study cohort using the multivariable Poisson regression model. Results are reported as adjusted relative risk (RR) with the corresponding 95 % confidence intervals (95 % CI).
Statistical analysis was performed using SAS statistical software version 9.2.2 (SAS Institute Inc., Cary, NC). All tests were two-tailed, and p values <0.05 were considered significant.
Results
Among 10,658 eligible patients with an acute ischemic stroke, 966 (9.1 %) had pre-existing dementia. Patients with pre-existing dementia were older (82 vs. 71 years; p < 0.001), and had more severe strokes (mean CNS score 7.9 vs. 6.3; p < 0.001). Diabetes, atrial fibrillation, coronary artery disease, and prior stroke/TIA were more prevalent in patients with dementia, whereas hyperlipidemia and smoking were more commonly found in patients without dementia. From the entire cohort, 877 (91 %) stroke patients with pre-existing dementia were matched with 877 stroke patients without dementia. Table 1 summarizes differences in baseline characteristics between groups before and after matching. There were no significant differences in baseline characteristics between patients with and without dementia in the matched cohort.
Overall, 1,668 (15.6 %) patients received thrombolytic therapy. Among patients with pre-existing dementia, 101 (10.5 %) received thrombolytic therapy, and 99 (98.0 %) of these were matched with 99 patients without dementia (Table 2).
Clinical outcomes
The main clinical outcome measures are summarized in Table 3 and Fig. 1.
Disability at discharge in stroke patients with and without pre-existing dementia before matching and after matching. This figure illustrates the disability at discharge according to the modified Rankin scale (mRS 0 no symptoms; 6 death) before and after propensity-score matching. The dotted lines show the corresponding category (mRS 0–2 and mRS 5–6) between patients with and without dementia. Before matching, there was a higher disability at discharge (mRS ≥ 3) among stroke patients with pre-existing dementia (p value <0.001). The differences disappeared after matching (RR 1.10, 95 % CI 0.96–1.27) for age, sex, stroke severity, stroke subtype (lacunar vs. non-lacunar), hypertension, diabetes, dyslipidemia, atrial fibrillation, previous stroke or transient ischemic attack, level of consciousness on arrival, dysphagia, glucose and creatinine levels on admission, place from arrival (home vs. other), pre-admission dependency, palliative care, stroke unit admission, thrombolysis, physiotherapy, and arrival by ambulance. Modified Rankin scale (mRS): 0 no symptoms, 1 no significant disability, able to carry out all usual activities, despite some symptoms; 2 slight disability, able to look after own affairs without assistance, but unable to carry out all previous activities; 3 moderate disability, requires some help, but able to walk unassisted; 4 moderately severe disability, unable to attend to own bodily needs without assistance, and unable to walk unassisted; 5 severe disability, requires constant nursing care and attention, bedridden, incontinent; 6 dead
Unmatched entire cohort
Unadjusted analyses of the unmatched cohort suggested lower survival at all points in time in patients with dementia compared to those without (Table 3). Similar findings were observed for death at discharge and at 1 year after stroke (Table 3). However, adjusted analyses revealed non-significant differences.
In an unadjusted analyses, disability at discharge, using the modified Rankin Scale (mRS), was higher in patients with dementia as compared to patients with no dementia (81.4 vs. 61.0 %; p < 0.001 for mRS 3–6) (Fig. 1). Patients with pre-existing dementia coming from home were less likely to be discharged home compared to patients without dementia (18.7 vs. 40.5 %) (Table 3). In addition, stroke patients with dementia appeared to be more likely to develop pneumonia (10.5 vs. 6.4 %; p < 0.001). Patients with dementia had longer mean length of hospital stay (LOS). However, adjusted analyses demonstrated no significant differences in any of these outcomes (Table 3).
Propensity-matched cohort
Similar to the adjusted analyses in the entire cohort, there were no differences in survival at 30 days (RR = 0.88, 95 % CI 0.75–1.03), at discharge (RR = 0.88, 95 % CI 0.74–1.05), or 1 year (RR = 1.01, 95 % CI 0.92–1.11) after stroke between patients with and without dementia (Table 3).
Disability at discharge was similar between patients with dementia and those without dementia (85.2 vs. 82.7 %) (Fig. 1). There was a slight increase in disability (RR = 1.10, 95 % CI 1.02–1.19) when only considering patients discharged alive (mRS 3–5) (Table 3). There were no significant differences in discharge to home, LOS, or risk of pneumonia between patients with and without pre-existing dementia (Table 3).
Clinical outcomes after thrombolytic therapy
In the original cohort, patients with pre-existing dementia were less likely to receive intravenous thrombolysis (10.5 vs. 16.2 %; p < 0.001) than their non-demented counterparts (Table 2).
Overall, 30-day mortality was higher among patients with dementia (26.7 vs. 16.9 %) in the unadjusted analysis, but the differences were not significant in the adjusted analysis (RR = 1.03, 95 % CI 0.67–1.60) (Table 4). Similarly, there were no significant differences in death or disability at discharge, disability at discharge, or disposition in the adjusted analysis in the original cohort. In the matched cohort, the risks of death, disability, and disposition after thrombolysis were similar in those with and without dementia. In addition, patients with and without pre-existing dementia had a comparable risk of ICH and neurological deterioration (Table 4).
Discussion
Stroke care for patients with pre-existing dementia represents a clinical challenge and may raise practical and ethical issues in management [3, 25]. Cerebral infarction is a risk factor for post-stroke dementia [2] and pre-stroke cognitive impairment or dementia itself can be associated with an increased risk of stroke [2]. The complex relationship between stroke and dementia is also known to have a pathological substrate: cortical or subcortical involvement after stroke in patients with Alzheimer pathology accelerates the clinical expression of dementia, affecting both the acute and chronic phase of stroke recovery [26]. There is continuing debate as to how to best manage stroke patients with pre-existing dementia. The lack of data on current processes and outcomes of care and the lack of established guidelines for the management and treatment of stroke patients with dementia contribute to this uncertainty.
In our study, we matched patients with and without pre-existing dementia presenting with an acute ischemic stroke and analyzed clinical and functional outcomes (e.g., disability at discharge and discharge home). We also evaluated outcomes and risks of intracerebral bleeding in a matched cohort of patients with and without dementia receiving thrombolytic therapy.
Patients with a history of dementia tended to be older women, had a higher prevalence of comorbid conditions (e.g., atrial fibrillation, and diabetes) and experienced more severe strokes. Although length of stay, disability, and mortality after stroke were all much higher in patients with dementia compared to those without in the overall sample, there was no significant difference in any of these outcomes in the propensity-matched cohort, suggesting that differences in outcomes after stroke are driven primarily by comorbid conditions rather than by dementia itself. In addition, among patients who received thrombolysis, there were no differences in rates of ICH, death, or disability between those with and without dementia.
In a previous descriptive study, we showed that patients with dementia were less likely to receive intravenous thrombolysis, even in the absence of recognized contraindications [27]. Differences in age, stroke severity, and overall frailty (e.g., disability, comorbidities) may explain why many clinicians decide not to treat these patients with thrombolysis. Excluding other medical reasons, contraindications were more common in patients with pre-existing dementia (13.5 vs. 7.5 %; p < 0.001). Herein, we showed similar clinical and functional outcomes for stroke patients receiving thrombolytic therapy with pre-existing dementia matched with those with no dementia. Interestingly, and despite the clinical perception, pre-existing dementia was not associated with a higher risk of ICH in the matched cohort.
Our study provides “real-world” information to address the question as to whether pre-existing dementia is an independent condition affecting clinical outcomes after ischemic stroke. Certainly, stroke patients with pre-existing dementia are frailer than their non-dementia counterparts. On average, patients with pre-stroke dementia were 11 years older and threefold more likely to be dependent than their non-dementia counterparts at the time of admission. Differences in demography, comorbidity, and disability make these patients highly vulnerable. For example, in the overall sample, death at 30 days or 1 year after stroke were twofold higher in patients with pre-existing dementia compared to those without dementia (Table 3). Similarly, only 18.7 % of dementia patients were discharged home compared to 40.5 % without dementia. However, when these differences in patient demographics and comorbidities were accounted for, we observed no significant differences in clinical and functional outcomes (e.g., disability at discharge, disposition) between patients with pre-existing dementia and those without.
Altogether, these findings suggest that dementia in itself does not explain the observed poorer outcomes in unadjusted analysis. Rather, differences in patient baseline characteristics, stroke severity, and comorbid conditions may better explain these results. Accordingly, pre-existing dementia by itself should not necessarily limit access to thrombolytic therapy or to specialized care (e.g., stroke unit admission, ICU care).
There are some conflicting results in the literature about the individual mortality risk in patients with pre-existing dementia. Our findings differ from previous studies showing higher mortality or disability in patients with dementia [8, 9, 28]. The results of previous studies could be explained by the presence of confounders as observed in our original (unmatched) study cohort. More concisely, propensity-score matching is commonly used in observational studies that have groups with substantial differences in their baseline characteristics, similar to the process of randomization in clinical trials, where groups become more comparable after adjusting for confounders, thus differing only in the exposure to the treatment/intervention [29].
In other studies, differences in mortality were attenuated after adjusting for covariates [8, 28]. Medical complications and vascular death rather than dementia itself were the most common causes of death [28, 30]. These studies had multiple limitations, including small sample sizes (ranging between 202 and 453 patients), limited exposure (low number of patients with prestroke dementia, n = 33 to n = 119), low number of outcomes (total patient deaths were between 29 and 63), and analytic methods (lack of use of propensity matching to reduce residual confounding) [8, 9, 28, 30]. No information was provided on the risk of ICH or outcomes after thrombolytic therapy.
Consistent with our findings, a recently published case-control study using administrative databases found no significantly increased risk between patients with dementia and without dementia with respect to ICH (5.80 vs. 4.51 %; p = 0.45) or death (17.4 vs. 14.5 %; p = 0.31) [31].
Our study has both limitations and strengths. First, the main limitation relates to the definition of dementia pre-stroke, which does not follow a specific cognitive assessment or a scale of activities of daily living activities before stroke to evaluate dependency. Second, as we had no quantitative measure of cognition in patients with dementia, it is possible that patients with mild cognitive impairment or mild dementia were not appropriately identified. This is not an uncommon scenario in clinical practice, where individuals with mild cognitive impairment/dementia are not usually diagnosed until more advanced stages of the disease. Moreover, the similarities in death and disability at discharge as well as in the risk of intracerebral hemorrhage after thrombolysis is reassuring, as we most likely captured patients with moderate to severe dementia. Another limitation includes the scarce information on brain imaging. Finally, the analytical approach—propensity matching—would attenuate the possibility of residual confounding when analyzing different outcome measures.
Despite these limitations, our study shows that over 50 % of stroke patients with pre-existing dementia are alive at 1 year, and 80 % of those discharged alive had greater disability and had a need for institutionalization. However, it is not the dementia itself that explains these outcomes, but rather the associated comorbidities. Specifically, the higher prevalence of diabetes, atrial fibrillation, and previous stroke in conjunction with older age and more severe strokes make stroke patients with dementia more vulnerable. Interestingly, survival, disability and complications (e.g., ICH) after receiving thrombolysis are not different for patients with dementia compared to matched non-demented patients, suggesting that preexisting dementia per-se may not preclude access to thrombolytic therapy.
Some clinicians have reservations, and consequently are less likely to offer, more aggressive stroke care to elderly patients with pre-existing dementia. Our results provide a different perspective regarding the acute treatment, care, and management of stroke patients with concomitant dementia and as well may help clinicians in their treatment care decisions and in facilitating patient and/or family counseling or discussions. In some circumstances, therapeutic decisions should be made on the basis of stroke severity, associated comorbidities, or patient and families’ preferences exclusive of the cognitive status.
Given the longer life expectancy in developed countries, the aging of the population, and recent discussions in health policy, this information will contribute to the ongoing debate pertaining to access to specialized care for this group of stroke patients. Representatives from governments, health care providers, and health insurers need to work together towards specific goals and priorities to facilitate access to stroke care and reduce the impact of stroke in this fragile population.
References
Canadian study of health and aging (1994) Study methods and prevalence of dementia. CMAJ 150:899–913
Public Health Agency of Canada (2009) Tracking heart disease and stroke in Canada. Ottawa
Pimlott NJ, Persaud M, Drummond N, Cohen CA, Silvius JL, Seigel K, Hollingworth GR, Dalziel WB (2009) Family physicians and dementia in Canada: part 2. Understanding the challenges of dementia care. Canadian family physician Medecin de famille canadien 55(508–509):e501–e507
Pimlott NJ, Persaud M, Drummond N, Cohen CA, Silvius JL, Seigel K, Hollingworth GR, Dalziel WB (2009) Family physicians and dementia in Canada: part 1. clinical practice guidelines: awareness, attitudes, and opinions. Canadian family physician Medecin de famille canadien 55(506–507):e501–e505
Rockwood K, Keren R (2010) Dementia services in Canada. Int J Geriatr Psychiatry 25:876–880
Canada PHA (2009) Tracking heart disease and stroke in Canada
Wimo A, Prince M (2010) Alzheimer’s disease international world Alzheimer report 2010: the global economic impact of dementia
Barba R, Morin MD, Cemillan C, Delgado C, Domingo J, Del Ser T (2002) Previous and incident dementia as risk factors for mortality in stroke patients. Stroke 33:1993–1998
Desmond DW, Moroney JT, Sano M, Stern Y (2002) Mortality in patients with dementia after ischemic stroke. Neurology 59:537–543
Ancona C, Arca M, Saitto C, Agabiti N, Fusco D, Tancioni V, Perucci CA (2004) Differences in access to coronary care unit among patients with acute myocardial infarction in Rome: old, ill, and poor people hold the burden of inefficiency. BMC Health Serv Res 4:34
Avendano M, Glymour MM (2008) Stroke disparities in older Americans: Is wealth a more powerful indicator of risk than income and education? Stroke 39:1533–1540
van der Steen JT, Ooms ME, Ader HJ, Ribbe MW, van der Wal G (2002) Withholding antibiotic treatment in pneumonia patients with dementia: a quantitative observational study. Arch Intern Med 162:1753–1760
Bejot Y, Rouaud O, Jacquin A, Osseby GV, Durier J, Manckoundia P, Pfitzenmeyer P, Moreau T, Giroud M (2010) Stroke in the very old: incidence, risk factors, clinical features, outcomes and access to resources–a 22-year population-based study. Cerebrovasc Dis 29:111–121
Finucane TE, Christmas C, Travis K (1999) Tube feeding in patients with advanced dementia: a review of the evidence. JAMA 282:1365–1370
2007 Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. CD000197
Saposnik G, Kapral MK, Coutts SB, Fang J, Demchuk AM, Hill MD (2009) Do all age groups benefit from organized inpatient stroke care? Stroke 40:3321–3327
Smith EE, Hassan KA, Fang J, Selchen D, Kapral MK, Saposnik G (2010) Do all ischemic stroke subtypes benefit from organized inpatient stroke care? Neurology 75:456–462
Kapral MK, Silver FL, Richards JA, Lindsay MP, Fang J, Shi S et al (2005) Registry of the Canadian stroke network. Progress report 2001–2005. Toronto
Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, Koroshetz W, Marler JR, Booss J, Zorowitz RD, Croft JB, Magnis E, Mulligan D, Jagoda A, O’Connor R, Cawley CM, Connors JJ, Rose-DeRenzy JA, Emr M, Warren M, Walker MD (2005) Recommendations for comprehensive stroke centers: a consensus statement from the brain attack coalition. Stroke 36:1597–1616
Bushnell CD, Johnston DC, Goldstein LB (2001) Retrospective assessment of initial stroke severity: comparison of the NIH stroke scale and the Canadian neurological scale. Stroke 32:656–660
Cote R, Battista RN, Wolfson C, Boucher J, Adam J, Hachinski V (1989) The Canadian neurological scale: validation and reliability assessment. Neurology 39:638–643
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107
Austin PC, Grootendorst P, Anderson GM (2007) A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 26:734–753
Mamdani M, Sykora K, Li P, Normand SL, Streiner DL, Austin PC, Rochon PA, Anderson GM (2005) Reader’s guide to critical appraisal of cohort studies: 2 assessing potential for confunding. BMJ 330:960–962
Massoud F, Lysy P, Bergman H (2010) Care of dementia in Canada: a collaborative care approach with a central role for the primary care physician. J Nutr Health Aging 14:105–106
Snowdon DA, Greiner LH, Mortimer JA, Riley KP, Greiner PA, Markesbery WR (1997) Brain infarction and the clinical expression of Alzheimer disease. The nun study. JAMA 277:813–817
Saposnik G, Cote R, Rochon PA, Mamdani M, Liu Y, Raptis S, Kapral MK, Black SE (2011) Care and outcomes in patients with ischemic stroke with and without preexisting dementia. Neurology 77:1664–1673
Appelros P, Viitanen M (2005) What causes increased stroke mortality in patients with prestroke dementia? Cerebrovasc Dis 19:323–327
Austin PC (2008) A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med 27:2037–2049
Henon H, Durieu I, Lebert F, Pasquier F, Leys D (2003) Influence of prestroke dementia on early and delayed mortality in stroke patients. J Neurol 250:10–16
Alshekhlee A, Li C–C, Chuang S-Y, Vora N, Edgell RC, Kitchener JM, Kale SP, Feen E, Piriyawat P, Callison RC, Cruz-Flores S (2011) Does dementia increase risk of thrombolysis? A case–control study. Neurology 76:1575–1580
Acknowledgments
Dr. Saposnik reports research funding from the Heart and Stroke Foundation of Canada, Canadian Institutes for Health Research, Department of Research at St. Michael’s Hospital and Connaught Foundation (University of Toronto); and salary support from the Clinician-Scientist Award from the Heart and Stroke Foundation of Ontario. Dr. Kapral holds a Career Investigator Award from the Canadian Institutes for Health Research and receives funding from the Canadian Stroke Network and the University Health Network Women’s Health Program.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Investigators of the Registry of the Canadian Stroke Network and the Stroke Outcome Research Canada (SORCan) Working Group.
Dr. M. Mamdani, S. E. Black contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saposnik, G., Kapral, M.K., Cote, R. et al. Is pre-existing dementia an independent predictor of outcome after stroke? A propensity score-matched analysis. J Neurol 259, 2366–2375 (2012). https://doi.org/10.1007/s00415-012-6508-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6508-4