Abstract
The goal of this study was to describe specifically the clinical characteristics of migraine with aura in patients over the age of 50. During 1 year, three neurologists working in a tertiary headache center included all patients aged 50 years and over presenting migraine with aura in a prospective registry. Fifty-seven patients with migraine with aura aged 50 years and over were interviewed using a standardized questionnaire during a consultation. Auras were visual for all the patients, paresthesic for 16 patients, and aphasic for 16. One patient had a sporadic hemiplegic migraine. The headache followed the aura in a large majority of patients and fulfilled the International Headache Society criteria for migraine headache for 38 patients. Typical aura without headache was described in 26 patients and was the only expression of the disease for five patients. Two groups can be defined: in the first one, migraine with aura began before 50 years (39 patients). Thirty-one patients had typical aura with migraine headache and 15 complained of typical aura without headache. The second group (18 patients) included patients who developed migraine with aura over 50 for the first time. Among them, patients may have typical aura with migraine headache (seven patients), typical aura with non-migraine headache (eight patients) and/or typical aura without headache (11 patients). Late-life onset transient visual phenomena are not rare. These symptoms may occur for the first time after 50, in the absence of headache. When migraine with aura began after 50 years, headache has more often the characteristics of typical aura with non-migraine headache, or migraine may have the presentation of typical migraine without headache.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is one of the most common neurological disorders, affecting about 11% of adult populations worldwide [1, 2]. Approximately one-third of individuals with migraine experience aura symptoms, usually consisting of transient visual, and also sensory, aphasic, or motor disturbances.
Migraine may occur at all ages, from the very young to the old, but is most common in the 3rd–5th decades of life. The prevalence of migraine is higher between the ages of 20 and 55 years, peaking at about age 40 and declining thereafter [3]. It has been suggested that both the prevalence and the characteristics of migraine change with age [4–6]. Migraine may attenuate over time (reduced frequency, severity, and/or duration). In middle-aged and elderly adults, vegetative symptoms (nausea, vomiting) are less prominent, and less intense pain, mostly localized in the neck, is frequently reported. Typical aura may also be experienced more frequently without headache [7].
In the literature, very few papers focus on migraine, and especially migraine with aura, in middle-aged adults. Thus, Marseille’s prospective registry was set up with the aim of describing the clinical characteristics of migraine with aura in a clinic-based sample of patients aged 50 years and over. Results from this study are presented below.
Methods
These cases were identified among patients participating in the French ‘Observatory of Migraine and Headaches’ (OMH), which is a national clinical research network on headache and facial pain set up in 2002 by the French Headache Society.
The national OMH network involves 16 tertiary care headache clinics and one specialized headache emergency department and overall covers approximately two-thirds of the French metropolitan territory. The setting up of the OMH database was declared to and approved by the French Commission on Data Processing and Liberties. Only, one center amongst the 16 centers, the Marseille’s center, participate to this registry.
During a 1-year period, three neurologists from the tertiary headache center of Marseille recruited patients presenting migraine with aura according to the International Classification of Headache Disorders, 2nd edn (ICHD-II) criteria, category 1.2 [8] and aged 50 years and over among all patients attending a consultation for headache/migraine. Data from these patients were included in the prospective Marseille’s registry.
For each patient included, neurologists completed a questionnaire that captured information about (1) patient’s demography and history (age, sex, age at the time of migraine onset, whether the patient also presents attacks without aura, and family history of headache); (2) headache characteristics (headache location, usual frequency, and accompanying symptoms); (3) aura characteristics (age at the time of aura onset, type of aura symptoms, duration of aura symptoms, whether aura symptoms are associated with headache, whether aura symptoms precede or accompany the headache, duration and type of associated headache); and (4) whether headache had already been investigated by computed tomography (CT) scan or magnetic resonance imaging (MRI). All of the participants gave informed consent to take part in the study.
Quantitative variables were summarized by descriptive statistics (mean ± standard deviation, median, and range) and qualitative variables were expressed as effectives and percentages. Two subgroups of patients were defined according to age at onset of migraine with aura: onset age <50 years and onset age ≥50 years. Comparisons between the two subgroups were performed using Student’s t test for quantitative variables and Chi-square or Fisher’s exact tests for frequencies. All tests were two-sided. Statistical significance was considered at p < 0.05. Statistical analyses were performed using the SPSS version 15.0 software package (SPSS Inc. Chicago, IL, USA).
Results
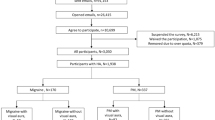
Among the 3,773 consecutive migraineurs attending the tertiary headache center of Marseille in the period September 2009–August 2010, 978 (26%) had migraine with aura (Fig. 1). Of these, 57 (6%) were aged 50 years or over and were included in the Marseille’s registry. The main characteristics of these patients are described in Table 1.
The registry population consisted mainly of elderly women. Two-thirds of patients reported a family history of headache, mostly probable migraine.
Aura always manifested by visual symptoms, mainly scintillating scotoma: 27 patients, blindness in half of a visual field (hemianopsia): 16 patients, foggy or blurred vision: 11 patients, teichopsia: five patients, or “like a kaleidoscope”: two patients. Eleven patients had various expression of their visual aura: hemianopsia and “like a kaleidoscope”: one patient; scotoma and blurred vision: two patients; scotoma and hemianopsia: six patients; teichopsia and blurred vision: one patient; teichopsia and hemianopsia: one patient.
Sensory (paresthesic), aphasic and motor aura were also reported. The various combinations of aura symptoms are illustrated in Fig. 2. Only visual aura frequently occurred in isolation, whereas sensory, motor, and aphasic symptoms were always experienced with visual aura (Fig. 2). One patient had a sporadic hemiplegic migraine.
Duration of aura ranged from 5 min to 1 h. Only two patients described the duration of the aura to be several hours. These two patients belong to the group of patients in which migraine began before 50. The headache followed the aura in a large majority of patients, lasting from 1 to 72 h, and fulfilled the International Headache Society criteria for migraine headache for 38 patients (Table 1). Auras without headache were described in 26 patients and were the only expression of the disease for five patients (Table 1). Acute-onset aura was never described.
Depending on the patient, frequency of migraine headache ranged from isolated episodes to daily attacks. In fact, five patients described daily headache. The clinical presentation was those of a migraine aura status. For three patients, it appears after the introduction of beta-blockers. For two patients, no precipitating factors were described. No medication overuse was reported. Thirty-six of the 57 patients diagnosed with migraine with aura (63%) also reported migraine attacks without aura (26 patients), and/or tension-type headache (nine patients).
Twenty-two patients had neither nausea and nor vomiting; 27 patients complain of nausea (but not systematically), but neither complained of vomiting. Only eight patients had severe migraine attacks, with both nausea and vomiting.
For most patients (72%), headache had already been investigated by CT scan (17 patients, 30%) or MRI (24 patients, 42%). Only three patients (7%) presented abnormal imaging findings: white matter hyperintensities (one patient), small ischemic lesion of the internal capsule (one patient), and vascular leucopathy related to arterial hypertension (one patient).
Two groups of patients can be defined depending on whether migraine with aura began before age 50 years or not. In the first group (migraine began before 50 years), consisting of 39 patients, the female-to-male ratio was 31/8 and mean age was 60.4 ± 9.6 years. Thirty-one patients complained of typical aura with migrainous headache. Typical aura without headache was reported by 15 patients (38.4%) and was the only expression of the disease for two patients (5%).
Group 2: migraine began after 50
Comparatively, in the second group of 18 patients (migraine began after 50 years) (female-to-male ratio 14/4; mean age 66.6 ± 10.9 years), typical aura with migrainous headache was reported by seven patients, typical aura with non-migraine headache by eight patients, and typical aura without headache was reported by 11 patients (61%, not significantly different) and was the only expression of the disease for three (17%, not significantly different).
Among the patients who presented typical aura with headache (37 in group 1 and 15 patients in group 2), a striking between-group difference was highlighted regarding the type of headache associated with aura symptoms. In the group of patients who developed migraine with aura before 50, typical aura was associated with migraine headache in 31 patients (79.5%), compared to only seven patients (38.9%) in the group of patients who developed migraine with aura over 50 for the first time. The remaining eight patients (44.44%) presented typical aura with non-migraine headache.
Family history of headache was significantly less frequently reported in patients with onset of migraine with aura after 50 years old, than in patients with onset of migraine with aura before 50 years.
Finally, in the group of patients in which migraine began after 50, 17 patients of 18 were investigated. CT scan (seven patients) and cerebral MRI (ten patients) were always normal, except for vascular leucopathy (one patient). Only one patient (a women aged 82) was not investigated, but the clinical symptoms were typical, and the patient had a history of migraine with aura since 32 years.
Discussion
To our knowledge, Marseille’s registry is the first survey that aimed at evaluating the symptomatology of migraine with aura in patients over 50 years of age. Over a 1-year period, a cohort of 57 patients aged 50 and older presenting migraine with aura according to the ICHD-II criteria was constituted, i.e., a prevalence of 1.5% among migraineurs in general, and of 5.8% among patients with migraine with aura in particular.
The patients included in Marseille’s registry consisted mainly of women (79%) and can be divided into two subgroups according to age at onset of migraine with aura: patients with early onset disease (onset age <50 years) and patients with late-onset disease (onset age ≥50 years). About one-third of the patients (18/57 patients) experienced migraine with aura for the first time after 50 years, i.e., a prevalence of 1.8% among patients with migraine with aura. This is in accordance with results from previous epidemiological studies that reported that only a small percentage (2–3%) of midlife patients experienced their first migraine after age 50 years [3].
Patients of Marseille’s registry presented usual patterns of auras. Auras preceded the headache in 92% of patients, and were most frequently characterized by visual symptoms (100% of patients), followed by sensory (28%), aphasic (28%), and motor (2%) symptoms. These frequencies of visual, sensory, aphasic, and motor auras are consistent with those reported in the literature [9, 10]. As described by Kelman [11], visual aura is the overwhelming aura symptom. Regarding the timing of the aura, most of our patients noted that migraine visual auras occurred mainly before the headache [12]. Recently, Queiroz [12] underline that blurred vision is the most frequently reported visual symptom. We confirm that this type of visual aura is not so rare.
Results regarding the migraine component, however, warrant further discussion. Of the 57 patients who suffer migraine with aura, 30 (53%) presented exclusively attacks of aura with headache, 22 (38%) had attacks of both aura with headache and aura without headache, and 5 (9%) had exclusively attacks of aura without headache. That is, typical aura without headache was experienced by 47% of patients included in Marseille’s registry, with 9% of them presenting aura without headache in every attack. These figures are quite high compared to those reported in the literature [11].
Population-based studies reported prevalence of typical aura without headache ranging from 0.2 in 40-year-old subjects from the general population [10] to 3.2–6.5% in adult primary eye care population (age range 6–95 years) [13, 14]. Results from cohorts of patients with migraine with aura showed higher prevalence, but still lower than those observed in our study. By example, in the study by Jensen et al. [9], headache was absent in 20% of aura attacks. In another cohort of 64 patients with migraine with aura aged 12–69 years, 12% of patients reported both types of aura attacks (with or without headache) and 6% exclusively aura without headache at first visit, while aura without headache was reported by about 30% of patients during the 6- to 15-month follow-up period [15].
Furthermore, five patients described a migrainous aura status. Migraine aura status was not included among the sub-types of migraine [8]. For three patients, this aura status appeared after the introduction of beta-blockers, as previously described [16].
The higher proportion of patients presenting aura without headache in our study may be due to the fact that Marseille’s registry involved older patients. Indeed, it is a general experience that attacks of aura without headache become increasingly frequent with age [14, 17, 18]. Some studies also suggested that such phenomenon may occur significantly more frequently in males than in females [15, 18]. Our results did not confirm this observation, however, probably due to the low number of male patients included in Marseille’s registry.
Another striking finding in our cohort of middle-aged and elderly migraineurs comes from the fact that some patients (and especially those with late-onset disease) experienced typical aura with a headache not fulfilling the full criteria for migraine (44.44% of patients who developed migraine with aura over 50 for the first time had typical aura with non-migraine headache, compared to 18% of those who developed migraine with aura before 50.
All together, these observations suggest that when patients with migraine with aura become older, their headache may partially lose the migraine characteristics or disappear completely even though auras continue. This bears out the findings and supports the conclusions that the characteristics of migraine change with age and that migraine attacks are less typical in the elderly.
Episodes of migrainous visual symptoms in mid or late life are not rare, and have been described as late-life migrainous accompaniments by others [19, 20]. Such episodes of transient visual, sensory, motor, or behavioral neurological manifestations are similar or identical to the auras of migraine with aura [21, 22]. They may occur for the first time after age 50 years, in the absence of headache, and a history of recurrent headaches may not be present. In these cases, diagnosis of migraine with aura remains largely based on the clinical features of the episodes, but requires the exclusion of other diagnoses, in particular, transient ischemic attacks (TIAs) or seizures.
In these cases, the diagnosis of migraine with aura remains largely based on the clinical features of the episodes; however, the usual diagnostic evaluation for transient ischemic attacks (TIAs) or seizures may be indicated to exclude vascular disease in cases with an atypical presentation. Indeed, aura symptoms, such as aphasia, visual scotoma, and paresthesias may closely mimic TIAs. Therefore differentiating TIA from aura becomes challenging in those patients in the stoke-age bracket (over age 50), since a large body of literatures supports an association between migraine with aura and vascular event including ischemic stroke and myocardial infarction [23–26]. Moreover, cephalic pain is frequent and often inaugural in cerebral vascular disease (carotid dissection, cerebral venous thrombosis) and can be the only sign [27, 28].
Our study is limited by the fact that it was performed in a clinic-based population from a single headache clinic in France, which might have introduced a selection bias. However, all patients attending the headache clinic over a 1-year period and fulfilling the inclusion criteria (diagnosis of migraine with aura, and age ≥50 years) were included. Moreover, the prevalence of migraine with aura among migraineurs (26%) does not appear to differ from that usually reported (less than one-third), suggesting that our sample of patients may be representative of the overall population of migraineurs with aura over 50 years of age. Finally, the number of patients studied is relatively small, and further studies are needed to confirm or complete these data.
Conclusion
The results of our study indicate that late-life onset transient visual phenomena are not rare. These symptoms may occur for the first time after 50, in the absence of headache and/or in presence of a headache that has mostly the characteristics of typical aura with non-migraine headache. Therefore, this study supports the concept of decreasing features of migraine occurring as the migraineur ages. This has clinical implications, since accurate diagnosis is crucial for disease management. In the elderly headache patient, diagnosis of migraine with aura should be based on the clinical features of the attacks and on the exclusion of TIA and seizure disorders.
Abbreviations
- ICHD-II:
-
International Classification of Headache Disorders, 2nd edition
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- TIAs:
-
Transient ischemic attacks
References
Lantéri-Minet M, Valade D, Géraud G, Chautard MH, Lucas C (2005) Migraine and probable migraine—results of FRAMIG 3, a French nationwide survey carried out according to the 2004 IHS classification. Cephalalgia 25:1146–1158
Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, Steiner T, Zwart JA (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27:193–210
Lipton RB, Diamond S, Reed M, Diamond ML, Steward WF (2001) Migraine diagnosis and treatment: results from the American migraine study II. Headache 41:638–645
Mattsson P, Svärdsudd K, Lundberg PO, Westerberg CE (2000) The prevalence of migraine in women aged 40–74 years: a population-based study. Cephalalgia 20:893–899
Wöber-Bingöl C, Wöber C, Karwautz A, Auterith A, Serim M, Zebenholzer K, Aydinkoc K, Kienbacher C, Wanner C, Wessely P (2004) Clinical features of migraine: a cross-sectional study in patients aged three to sixty-nine. Cephalalgia 24:12–17
Kelman L (2006) Migraine changes with age: IMPACT on migraine classification. Headache 46:1161–1171
Reinisch VM, Schankin CJ, Felbinger J, Sostak P, Straube A (2008) Headache in the elderly. Schmerz 22(Suppl. 1):22–30
Headache Classification Subcommittee of the International Headache Society (2004) The international classification of headache disorders, 2nd edition. Cephalalgia 24(Suppl 1):9–160
Jensen K, Tfelt-Hansen P, Lauritzen M, Olesen J (1986) Classic migraine. A prospective recording of symptoms. Acta Neurol Scand 73:359–362
Russell MB, Olesen J (1996) A nosographic analysis of the migraine aura in a general population. Brain 119:355–361
Kelman L (2004) The aura: a tertiary care study of 952 migraine patients. Cephalalgia 24:728–734
Queiroz LP, Friedman DI, Rapoport AM, Purdy RA (2011) Characteristics of migraine visual aura in southern Brazil and northern USA. Cephalalgia 31(16):1652–1658
Fleming JB, Amos AJ, Desmond RA (2000) Migraine aura without headache: prevalence and risk factors in a primary eye care population. Optometry 71:381–389
Aiba S, Tatsumoto M, Saisu A, Iwanami H, Chiba K, Senoo T, Hirata K (2010) Prevalence of typical migraine aura without headache in Japanese ophthalmology clinics. Cephalalgia 30:962–967
Cologno D, Torelli P, Cademartiri C, Manzoni GC (2000) A prospective study of migraine with aura attacks in a headache clinic population. Cephalalgia 20:925–930
Tfelt-Hansen P, Rolan P (2006) Beta adrenoreceptor blocking drugs in migraine prophylaxis. In: Olesen J, Goadsby PJ, Ramadan NM, Tfelt-Hansen P, Welch KMA (eds) The headaches, 3rd revised edn. Lippincott Williams and Wilkins, Philadelphia, p 526
Hedges TR (1973) Isolated ophthalmic migraine: its frequency, mechanisms, and differential diagnosis. In: Smith JL (ed) Neuro-ophthalmology. Symposium of the University of Miami and the Bascom Palmer Eye Institute, St Louis, MO, Mosby, pp 140–150
Cologno D, Torelli P, Manzoni GC (1998) Migraine with aura: a review of 81 patients at 10–20 years’ follow-up. Cephalalgia 18:690–696
Wijman CAC, Wolf PA, Kase CS, Kelly-Hayes M, Beiser AS (1998) Migrainous visual accompaniments are not rare in late life: the Framingham study. Stroke 29:1539–1543
Fisher CM (1999) Late-life (migrainous) scintillating zigzags without headache: one person’s 27-year experience. Headache 39:391–397
Fisher CM (1980) Late-life migraine accompaniments as a cause of unexplained transient ischemic attacks. Can J Neurol Sci 7:9–17
Fisher CM (1986) Late-life migraine accompaniments: further experience. Stroke 17:1033–1042
Kurth T, Schürks M, Logroscino G, Buring JE (2009) Migraine frequency and risk of cardiovascular disease in women. Neurology 73:581–588
Scher AI, Gudmundsson LS, Sigurdsson S, Ghambaryan A, Aspelund T, Eiriksdottir G, van Buchem MA, Gudnason V, Launer LJ (2009) Migraine headache in middle age and late-life brain infarcts. JAMA 301:2563–2570
Bigal ME, Kurth T, Santanello N, use D, Golden W, Robbins M, Lipton RB (2010) Migraine and cardiovascular disease: a population-based study. Neurology 74:628–635
Gudmundsson LS, Scher AI, Aspelund T, Johannsson M, Thorgeirsson G, Launer L, Gudnason V (2010) Migraine with aura and risk of cardiovascular disease and all cause mortality in men and women: prospective cohort study. BMJ 341:c3966
Biousse V, D’Anglejan-Chatillon J, Massiou H, Bousser MG (1994) Head pain in non-traumatic carotid artery dissection: a series of 65 patients. Cephalalgia 14(1):33–36
Cumurciuc R, Crassard I, Sarov M, Valade D, Bousser MG (2005) Headache as the only neurological sign of cerebral venous thrombosis: a series of 17 cases. J Neurol Neurosurg Psychiatry 76(8):1084–1087
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donnet, A., Daniel, C., Milandre, L. et al. Migraine with aura in patients over 50 years of age: the Marseille’s registry. J Neurol 259, 1868–1873 (2012). https://doi.org/10.1007/s00415-012-6423-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6423-8