Abstract
Cerebellar adult onset ataxia is a heterogeneous condition. The aim of this study was to ascertain if there is a heightened autoimmune background in patients with sporadic cerebellar ataxia of unknown origin, and if autoimmunity correlates with a more rapid evolution of the ataxia. We selected patients with sporadic progressive adult onset cerebellar ataxia with a follow-up of >5 years. As controls we included 43 patients with genetically demonstrated hereditary ataxia. All patients were tested for a panel of neuronal (onconeuronal, glutamate-decarboxylase [GAD], IgG/IgA transglutaminase 6 antibodies) and systemic non-neuronal antibodies (including IgG/IgA gliadin and transglutaminase 2, thyroperoxidase, thyroglobulin, antinuclear, striational, smooth muscle, mitochondrial, liver kidney microsomal, and parietal gastric cells antibodies). Correlation between the antibodies and disease progression was studied with Cox regression models and Kaplan–Meier plots. Forty-four patients were included. All patients were negative for onconeuronal or GAD antibodies. There were no significant differences between patients and controls in the prevalence of transglutaminase 6, 2, gliadin, or thyroid antibodies. However, when we studied the panel of systemic non-neuronal autoantibodies as a group, antibodies were more frequent in patients with sporadic ataxia (p = 0.018). The presence of one or more systemic non-neuronal antibodies correlated with a faster evolution to stage 2 (loss of independent gait) (p = 0.03) and shorter survival (p = 0.03) in patients with sporadic ataxia. We conclude that there is probably a heightened autoimmune background in some patients with sporadic cerebellar ataxia of unknown origin. The presence of systemic non-neuronal autoantibodies is a prognostic marker.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physicians dealing with patients presenting with sporadic adult-onset cerebellar ataxia are challenged to recognize treatable conditions [1, 2.] There is evidence that autoimmunity leads to neuronal loss in paraneoplastic cerebellar degeneration (PCD), and these patients may benefit from aggressive immune (and antineoplastic) treatment. It has also been suggested that autoimmunity underlies subacute non-paraneoplastic cerebellar ataxia. However, because of the lack of serological markers and the unclear nosologic limits of this condition it is often difficult to make early treatment decisions. An exception is the presence of anti-glutamic acid decarboxylase (GAD) antibodies in some patients that usually have a slower progression of the cerebellar symptoms. The role of autoimmunity in other chronic forms of sporadic adult-onset ataxia remains speculative. As an example, there is controversy as to whether silent celiac disease can be presented solely with cerebellar ataxia. Some investigators have suggested that ataxia in these patients is immune mediated and proposed to name this disorder “gluten ataxia” [3, 4].
We studied a panel of neuronal and systemic autoantibodies in a series of patients with sporadic cerebellar ataxia to ascertain if there is a heightened autoimmune background, and if autoimmunity correlates with a more rapid evolution of the ataxia.
Methods
Patients
We studied patients referred to the ataxias unit of our center between 1995 and 2005 with progressive cerebellar ataxia, onset after the age of 20 years and a follow-up of at least 5 years. Exclusion criteria were the following: (1) abnormal brainstem or cerebellar MRI findings other than cerebellar atrophy; (2) clinical or MRI features of multiple system atrophy, progressive myoclonic ataxia, fragile-X-associated tremor/ataxia syndrome, MERRF (myoclonic epilepsy with ragged-red fibers), MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes) or NARP (neuropathy, ataxia, and retinitis pigmentosa); (3) exposure to alcohol or other toxins on the cerebellum; (4) vitamin B12 or E deficiency; (5) clinical, laboratory or MRI evidence of HIV, syphilis, prionopathy, or Whipple disease; (6) positive family history of ataxia or parental consanguinity; (7) positive genetic test (all patients were screened for Friedreich ataxia, dentatorubropallidoluysian ataxia, SCA1,2,3,6,7, and 8 genes; when clinically indicated FMR1 premutation was studied). To study disease progression we defined the following stages (modified from reference [5]): stage 0 = no gait difficulties; stage 1 = disease onset, as defined by onset of gait difficulties; stage 2 = loss of independent gait, as defined by permanent use of a walking aid or reliance on a supporting arm; stage 3 = confinement to wheelchair, as defined by permanent use of a wheelchair; stage 4 = confinement to bed; stage 5 = death. As a control group for our study we selected 43 patients with genetically demonstrated hereditary ataxia: 20 Friedreich ataxia, 1 SCA2, 11 SCA3, 10 SCA6, 1 SCA7. Serum was obtained in the first visit or admission under informed consent and kept frozen at −80°C. We received approval from the ethical standards institutional committee. Written informed consent for research was obtained from all patients participating in the study.
Immunological studies
Serum samples of all patients were tested for the following antibodies:
Antineuronal antibodies
Well characterized onconeuronal, Tr, and GAD antibodies were studied with indirect immunofluorescence (IF) as previously described [6]. Positive samples were confirmed with immunoblots of whole rat cerebellum extracts or human recombinant proteins. Neuronal transglutaminase 6 IgG/IgA (TG6) antibodies were studied with ELISA following manufacturers instructions (Zedira, Darmstadt, Germany).
Panel of systemic non-neuronal antibodies
Gliadin, transglutaminase 2 IgG/IgA (TG2), thyroperoxidase and thyroglobulin antibodies were studied with ELISA. Standard indirect immunofluorescence on rat tissues was used for testing the following antibodies: antinuclear antibodies (ANA), striational antibodies, anti-smooth muscle antibodies, anti-mitochondrial antibodies, anti-liver kidney microsomal antibodies (ALKM), anti-parietal gastric cell antibodies (APGC).
Statistical analysis
To compare the demographic characteristics and frequency of antibodies between groups, the χ2 or t Student tests were used accordingly. Cox multivariate regression model and Kaplan–Meier plots were used to evaluate the association between systemic antibodies and disease progression.
Results
Patients and immunological associations (Table 1)
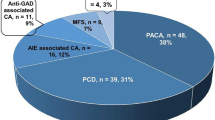
Fifty patients fulfilled the inclusion criteria for our study. Five patients developed cancer within 5 years of the onset of the ataxia (PCD). Three had well characterized onconeuronal antibodies (Abs) (two anti-Yo and ovarian cancer, one anti-Hu and lung cancer); one of the patients with anti-Yo Abs had also TG6 antibodies. One patient had GAD Abs and thymic carcinoid (previously reported [7]), and another patient had cerebellar ataxia, Lambert–Eaton myasthenic syndrome, and lung cancer. These patients were excluded from further analysis. We also excluded a woman with anti-Yo antibodies and no cancer after a follow-up of 5 years. None of the remaining 44 patients with sporadic ataxia or 43 control patients with genetic ataxia had onconeuronal or GAD antibodies. Nine patients with sporadic ataxia and four controls had atypical reactivities on IF on rat cerebellum (p = 0.145). We found eight patients with TG6 antibodies (Table E-1): five patients with sporadic ataxia of unknown origin, two patients with Friedreich ataxia, and one patient with SCA3. When analyzed as a group, the presence of one or more of the systemic non-neuronal auto-antibodies was more frequent in patients with sporadic ataxia (p = 0.018). No significant statistical differences were found when gliadin IgG/IgA, TG2 IgG/IgA, or thyroid antibodies were analyzed independently.
Analysis of the influence of autoimmunity on disease progression and survival (Fig. 1)
Kaplan–Meier longitudinal analysis showed that in patients with sporadic ataxia, the presence of one or more of the systemic non-neuronal antibodies correlated with a faster evolution to reach stage 2 (loss of independent gate) (p = 0.03; log rank 5.35) and shorter survival (p = 0.03; log rank 7.8). The mean latency to reach stage 2 was 4.3 years (Fig. 1a) for patients with one or more antibodies, and was shorter (2.1 years, p < 0.01; log rank 14.7) for patients with a higher autoimmune “load” (two or more positive antibodies). The Cox multivariate regression analysis adjusted for age and sex confirmed the presence of systemic non-neuronal antibodies as the only independent prognostic factor for reaching stage 2 (odds ratio-OR- 2.4, 95% CI 1.1–5.3, p = 0.031) and death (OR 6.3, 95% CI 1.3–33.6, p = 0.030).
Kaplan–Meier graphs. a Latency to reach stage 2 (loss of independent gait) in patients with sporadic ataxia positive for one or more systemic non-neuronal autoantibodies versus seronegative patients (p = 0.03). b Idem, patients positive for two or more systemic non-neuronal autoantibodies versus the rest (p < 0.01). c Mortality of patients with sporadic ataxia positive for one or more systemic non-neuronal autoantibodies versus seronegative patients (p = 0.03)
Significant differences persisted when the six patients who had subacute cerebellar ataxia (time to reach stage 2 of less than 4 months) were excluded from this analysis (Fig. E-1).
Discussion
In this study the presence of systemic autoantibodies was related to a higher risk of disability progression and death in patients with sporadic ataxia of unknown origin. While autoimmunity may have played a role in the progression of neuronal destruction, we failed to demonstrate specific neuronal autoimmunity in these patients. Because of the similarities with PCD, and the recent finding of implicated neuronal antigens [8], it is believed that subacute sporadic cerebellar ataxia is immune mediated. Although our findings support this hypothesis, there was no clear cut between patients with less/more than 4 months of evolution (the most widely accepted temporal criteria for subacute ataxia) [9]. In fact, the prognostic impact of systemic autoimmunity persisted in patients with more than 4 months of evolution.
When systemic antibodies as a group were studied, they were more frequently found in patients with sporadic ataxia as compared with genetic ataxia. Although age-related increase in autoantibody prevalence can be in part responsible for this difference [10], these antibodies are probably markers of a heightened autoimmune background in some patients with sporadic ataxia. This hypothesis is further strengthened by the correlation between systemic antibodies and the more rapid evolution of the symptoms and shorter survival. Of interest, the individual frequency of gliadin, tranglutaminases 2/6 or thyroid antibodies did not reach significant differences between patients with sporadic and genetic ataxias. These data argue against specific entities such as Hashimoto [11] or gluten ataxia [3]. Recently, it has been reported that antibodies against the neuronal specific transglutaminase (TG6) are markers of gluten ataxia [12]. We were not able to replicate this finding as we found anti-TG6 antibodies in patients with paraneoplastic, sporadic and genetic ataxias, including Friedreich ataxia and Machado–Joseph disease. TG6 antibodies might be secondary to neuronal damage, rather than being pathogenic. Of interest, neuronal transglutaminase interact with abnormally expanded polyglutamine tracts in patients with SCA3 [13]. Whether the immune system recognizes neuronal protein aggregates in patients with polyglutamine expansion diseases needs further investigation.
We conclude that there is probably a heightened autoimmune background in some patients with sporadic cerebellar ataxia of unknown origin. The presence of systemic non-neuronal autoantibodies is a prognostic marker. Further research is needed to identify reliable serological markers of patients with autoimmune non paraneoplastic ataxias.
References
Klockgether T (2010) Sporadic ataxia with adult onset: classification and diagnostic criteria. Lancet Neurol 9:94–104
Bürk K, Wick M, Roth G et al (2010) Antineuronal antibodies in sporadic late-onset cerebellar ataxia. J Neurol 257:59–62
Hadjivassiliou M, Grünewald R, Sharrack B et al (2003) Gluten ataxia in perspective: epidemiology, genetic susceptibility and clinical characteristics. Brain 126:685–691
Abele M, Schöls L, Schwartz S, Klockgether T (2003) Prevalence of antigliadin antibodies in ataxia patients. Neurology 60:1674–1675
Klockgether T, Lüdtke R, Kramer B et al (1998) The natural history of degenerative ataxia: a retrospective study in 466 patients. Brain 121:589–600
Rubio-Agusti I, Perez-Miralles F, Sevilla T et al (2011) Peripheral nerve hyperexcitability: a clinical and immunological study of 38 patients. Neurology 76:172–178
Bataller L, Valero C, Diaz R et al (2009) Cerebellar ataxia associated with neuroendocrine thymic carcinoma and GAD antibodies. J Neurol Neurosurg Psychiatry 80:696–697
Zuliani L, Sabater L, Saiz L et al (2007) Homer 3 autoimmunity in subacute idiopathic cerebellar ataxia. Neurology 68:239–240
Abele M, Bürk K, Schöls L et al (2002) The aetiology of sporadic adult-onset ataxia. Brain 125:961–968
Ramos-Casals M, García-Carrasco M, Brito MP et al (2003) Autoimmunity and geriatrics: clinical significance of autoimmune manifestations in the elderly. Lupus 12:341–355
Selim M, Drachman DA (2001) Ataxia associated with Hashimoto’s disease: progressive non-familial adult onset cerebellar degeneration with autoimmune thyroiditis. J Neurol Neurosurg Psychiatry 71:81–87
Hadjivassiliou M, Aeschlimann P, Striqun A et al (2008) Autoantibodies in gluten ataxia recognize a novel transglutaminase. Ann Neurol 64:332–343
Violante V, Luongo A, Pepe I et al (2001) Transglutaminase dependent formation of protein aggregates as possible biochemical mechanism for polyglutamine diseases. Brain Res Bull 56:169–172
Acknowledgment
The authors thank Emilia Cabañero for excellent technical assistance, and Francesc Graus, Hospital Clinic, Barcelona, Spain for confirmation of positive onconeuronal antibody tests. Grant PS09/01350, Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Madrid, Spain.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sivera, R., Martín, N., Boscá, I. et al. Autoimmunity as a prognostic factor in sporadic adult onset cerebellar ataxia. J Neurol 259, 851–854 (2012). https://doi.org/10.1007/s00415-011-6266-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6266-8