Abstract
Spinal and bulbar muscular atrophy (SBMA) is an adult-onset, X-linked motor neuron disease characterized by muscle atrophy, weakness, and bulbar involvement. The aim of this study was to analyze the differential change of various outcome measures by comparing the progression of motor impairment in the two independent groups: placebo-treated group (PTG) and natural history group (NHG). For the PTG, we analyzed 99 patients who participated in a previous double-blind phase III clinical trial and received placebo. For the NHG, a total of 34 patients were followed with no specific treatment. The characteristics of both groups did not differ at baseline except for disease duration. Although the 6 min walk distance (6MWD) showed almost the same progression in both groups (−14.7 ± 7.3 m in NHG, −14.0 ± 4.7 m in PTG; NS), there was a significant difference of progression in the ALSFRS-R between the NHG and PTG (−1.18 ± 0.38, −0.14 ± 0.24; p = 0.03). A similar tendency was also seen in the subgroup analysis of the patients whose disease durations were less than 10 years. Although the relationship between the ALSFRS-R and 6MWD at week 48 was similar to that at baseline in the NHG, the slope of the regression at week 48 was significantly milder than at baseline in the PTG (p = 0.04). In conclusion, these two groups demonstrated a large difference in the chronological analysis of a motor function score, but showed similar changes in objective measures of walking capacity. These findings should be thoroughly considered when designing clinical trials for slowly progressive neurodegenerative diseases such as SBMA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal and bulbar muscular atrophy (SBMA) is an adult-onset, hereditary motor neuron disease characterized by muscle atrophy, weakness, and bulbar involvement [1–4]. SBMA is caused by the expansion of a CAG triplet repeat within the first exon of the androgen receptor (AR) gene [5, 6]. SBMA is a male-specific disease and this appears to stem from the testosterone-dependent accumulation of pathogenic AR proteins in affected neurons [7–13]. In SBMA mouse models, surgical castration delays the disease onset and reverses the neuromuscular phenotype [10, 13]. Similar effects emerge when the mice are treated with leuprorelin, a luteinizing hormone-releasing hormone agonist that reduces testosterone release [11]. In a phase II clinical trial, leuprorelin suppressed the accumulation of pathogenic AR and slowed the deterioration of motor function in SBMA patients during an open-labeled follow-up period [14, 15]. However, in a large scale phase III randomized controlled trial, the effects of leuprorelin on clinical endpoints were not clearly demonstrated [16]. These discrepancies appear to be partly attributable to placebo-related effects in the large scale trial [16]. Namely, the decrease in motor functions of placebo-treated patients in the phase III trial was milder than that in previous clinical studies without intervention [15].
The effects of placebo on outcome measures are likely to be an important concern in clinical trials of disease modifying therapies for neurodegenerative disorders, because placebo-related improvements may mask the true efficacy of interventions [17, 18]. It is, however, difficult to precisely estimate the magnitude of the placebo effect. The aim of this study was to analyze the effects of placebo on various outcome measures by comparing the progression of motor impairment in untreated and placebo-treated SBMA patients.
Methods
Patients
We analyzed two independent groups: the natural history group (NHG) and the placebo-treated group (PTG). For the NHG, a total of 34 male patients with a diagnosis of SBMA were recruited consecutively and received no specific treatment. The inclusion criteria for the NHG were as follow: (1) genetically confirmed male Japanese SBMA patients with more than one of the following symptoms: muscle weakness, muscle atrophy, or bulbar palsy; and (2) aged 25–75 years old at the time of informed consent. Patients were excluded if they met any of the following criteria: (1) inability to attend periodical follow-up visits; (2) unable to stand upright for 6 min without assistance; (3) tachycardia (>120/min) or uncontrolled hypertension (>180/100 mmHg); (4) angina pectoris or myocardial infarction; (5) severe bulbar palsy or other severe complications such as malignancy; (6) medical history of allergy to barium; (7) hormonal therapies within 48 weeks before informed consent; (8) castrated; and (9) participated in any other clinical trials within 12 weeks before informed consent. All of the patients were followed in Nagoya University Hospital. Data collected during the 48 weeks from the initial evaluation were used for this study. Data for the NHG patients were collected between January 2007 and May 2008.
For the PTG, we used the data from 99 male patients with SBMA who participated in the previous randomized double-blind phase III clinical trial and received placebo for 48 weeks [16]. The inclusion and exclusion criteria for the PTG were equivalent to those for the NHG [16]. Briefly, patients who were 30–70 years old without a desire to procreate were included.
Both studies conformed to the ethical guidelines for human genome/gene analysis research and those for epidemiological studies endorsed by the Japanese government. The Institutional Review Board of Nagoya University Graduate School of Medicine approved the study, and all of the participants gave their written informed consent.
Clinical evaluations
The common measurements for the NHG and PTG were the revised amyotrophic lateral sclerosis functional rating scale (ALSFRS-R), the 5-item amyotrophic lateral sclerosis assessment questionnaire (ALSAQ-5), a modified quantitative myasthenia gravis score (mQMG score), and the 6 min walk distance (6MWD). These outcome measures were used to evaluate the activities of daily living (ADL), quality of life, motor function, and walking capacity, respectively, and were measured at weeks 0, 24, and 48 in both NHG and PTG.
The ALSFRS is a validated questionnaire-based scale that measures physical function in ALS patients performing the ADL [19]. The revised version of this scale, the ALSFRS-R, was generated to improve the disproportion of weighting given to the limbs and bulbar, as compared to respiratory dysfunction, in the original test. The ALSFRS-R was translated into Japanese and validated [20]. The ALSFRS-R is divided into three domains: bulbar-related, limb- and trunk-related, and respiration-related [20].
The ALSAQ-5 is a subjective health measure that was designed for ALS. This questionnaire was developed from the original version, the ALSAQ-40, through the process of item reduction. The ALSAQ-5 and its original version were developed and validated by Jenkinson et al. [21, 22], and the Japanese translation of this test has also been validated [23].
The QMG score is a measure to detect muscle weakness that was originally designed for myasthenia gravis [24]. We used a modified QMG (mQMG) score that measures the muscle power of the extremities and neck flexion. The best possible score is 0 and the worst possible is 15. The scores of mQMG is shown to correlate well with those of ALSFRS-R in the baseline data of the phase III trial of leuprorelin for SBMA [16].
The 6 min walk test is a popular clinical test that has been used to assess functional capacity. The distance traveled during 6 min, 6MWD, is a parameter that evaluates the global and integrated responses of all the systems involved in walking, including the neuromuscular, pulmonary, and cardiovascular systems. Its validity has been verified in various neuromuscular disorders including SBMA [25–27].
Genetic analysis
Genomic DNA was extracted from the peripheral blood of the SBMA patients using conventional techniques. PCR amplification of the CAG repeat in the AR gene was performed using a fluorescein-labeled forward primer (5′-TCCAGAATCTGTTCCAGAGGTGC-3′) and a non-labeled reverse primer (5′-TGGCCTCGCTCAGGATGTCTTTAAG-3′). The detailed PCR conditions were described previously [28]. Aliquots of the PCR products were combined with a loading dye and separated by electrophoresis with an autoread sequencer (SQ-5500; Hitachi Electronics Engineering, Tokyo, Japan). The size of the PCR standards was determined by direct sequencing, as described previously [28].
Statistical analysis
All variables were summarized using descriptive statistics, including range, mean, standard deviation (SD), and standard error (SE). Relationships between the various values obtained in this study were analyzed using Pearson’s correlation coefficient. The last observation carried forward method was used to impute missing values when the data were missed only at week 48. The data of patients who were neither evaluated at week 24 nor at week 48 were eliminated from the analysis. The difference between the data at weeks 0 and 48 was analyzed using the paired t test. The difference in progression at 48 weeks between the NHG and PTG was evaluated using the unpaired t test. The sample size required for the clinical trials was estimated using the 48 week chronological data of each group (α = 0.05, β = 0.20). The difference in the slope of regression lines was calculated using the t test. Calculations were performed using the statistical software package Dr. SPSS II for Windows (SPSS Japan Inc., Tokyo, Japan).
Results
Clinical backgrounds of SBMA patients and correlations between the outcome measures
The baseline characteristics of the patients are shown in Table 1. There were a total of 133 subjects (NHG 34, PTG 99). The characteristics of both groups did not differ at baseline except for the disease duration from onset, which was shorter in the NHG. All of the four outcome measures, ALSFRS-R, ALSAQ-5, mQMG, and 6MWD, correlated well with each other in the NHG and PTG, indicating the legitimacy of the clinical evaluations used in this study (Table 2).
48 week chronological change of outcome measures
The 48 week chronological changes in each group are shown in Table 3. One patient in the PTG was lost to follow-up at week 48 because the primary end point of the clinical trial was unmeasurable. In the NHG, one patient was lost to follow-up at weeks 24 and 48 and three patients were lost to follow-up only at week 48 because of inability to attend periodical follow-up visits. The values of the 6MWD significantly decreased over 48 weeks in both groups. Although the ALSFRS-R and mQMG significantly deteriorated in the NHG, neither of these measures showed significant changes in the PTG. We then compared the rate of the 48 week chronological change between the NHG and PTG. The results showed that there was a significant difference in the chronological change rate of the ALSFRS-R between the NHG and PTG (p = 0.03). On the other hand, no significant difference was found in the 48 week chronological change between the two groups with respect to the ALSAQ-5, mQMG, or 6MWD. The same analysis was performed on each domain of the ALSFRS-R: bulbar-related, limb- and trunk-related, and respiration-related. Although no significant differences in the bulbar- or respiration-related domains were seen between the two groups, the inter-group difference was significant in the limb- and trunk-related domain (p = 0.02). Similar results were obtained when we analyzed the data of patients who completed 48 week follow-up (Supplementary Table 1, 2).
The difference in disease duration between the two groups at baseline may influence the results of our comparison between the NHG and PTG. To ensure the comparability of the two study groups, we analyzed the subset of patients whose disease duration was less than 10 years in each group. The characteristics of these groups did not differ at baseline (Table 1). The differences of chronological changes in the outcome measures between the NHG and PTG within these subgroups were similar to those in the total cases (Table 3). These results indicate that the difference of background at baseline does not have a critical effect on the results of our comparison between the NHG and PTG.
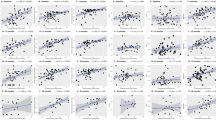
We next investigated the relationship between the 6MWD and ALSFRS-R at weeks 0 and 48 in both groups (Fig. 1). The relationship between these measures at week 48 was similar to that at baseline in the NHG, suggesting that the evaluation of motor function using the ALSFRS-R was plausible at the end of the observation period in this group. However, the slope of the regression line shifted from 0.019 to 0.013 during the 48 week follow-up in the PTG (p < 0.05), suggesting that the placebo treatment affected the evaluation of motor function in these patients.
Relationships between the 6MWD and ALSFRS-R in the NHG and PTG. The slopes of the regression lines in the NHG were not significantly different between week 0 (a) and week 48 (b). On the contrary, the slope of the regression line at week 48 (d) was significantly milder than at week 0 (c) in the PTG (p = 0.04). 6MWD 6 min walk distance, ALSFRS-R the revised amyotrophic lateral sclerosis functional rating scale, NHG natural history group, PTG placebo-treated group
Sample size estimation
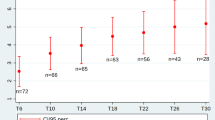
To clarify the influence of the placebo-related effects on the design of clinical trials, we calculated the sample size for placebo-controlled studies using data from the NHG and PTG. Table 4 shows the subject numbers per arm required for clinical trials to demonstrate a 50 or 100% reduction of deterioration in each outcome measure using chronological data. According to the estimation based on the chronological data in the PTG, over 10,000 subjects per arm are necessary to demonstrate a 50% therapeutic effect in the ALSFRS-R. In contrast, only 139 subjects are necessary when we calculate the sample sizes on the basis of the chronological data of the ALSFRS-R in the NHG. On the other hand, sample sizes were similar between the NHG and PTG, when they were calculated on the basis of the chronological data of the 6MWD.
Discussion
In the present study, we assessed the clinical severity of SBMA using quantitative outcome measures: the ALSFRS-R, ALSAQ-5, mQMG, and 6MWT. Two study groups, the NHG and PTG, were independently followed by similar protocols for 48 weeks.
The main aim of this study was to compare disease progression between untreated and placebo-treated patient groups that were evaluated with similar protocols. As the two groups were independent cohorts, and not randomly assigned from a common population, the findings of the present study should be interpreted cautiously. Our results, however, clearly demonstrate that the difference of chronological changes between the NHG and PTG varied according to the outcome measures. Although the 6MWD showed almost the same progression in both groups, there was a statistically significant difference of progression in the ALSFRS-R between the NHG and PTG. Further examination of the ALSFRS-R revealed that there was a significant difference in the limb- and trunk-related domain between the NHG and PTG, although no significant difference was found in either of the other domains. In addition, our results demonstrated that placebo treatment possibly alters the relationship between the ALSFRS-R and 6MWD over 48 weeks. The results of sample size estimation also demonstrated profound differences between the NHG and PTG with respect to the ALSFRS-R.
In the assessment of disease progression in neurodegenerative diseases, we should take several factors that can modify the true progression into account. Above all, the placebo effect should be considered in placebo-treated subjects. Although it is difficult to define the placebo effect, this term can be divided into at least two categories in clinical trials: the improvement due to the pharmacological effect of the placebo itself, and the improvement resulting from psychophysiological effects such as a positive expectation for a new treatment by patients and raters or a subconscious desire to meet the attending doctor’s expectations. Several studies suggested that the placebo effect tends to be prominent in neurological disorders [18, 29]. On the other hand, so-called negative expectations can be generated in the evaluation of natural history without intervention, since the patients or raters may assume that the symptoms must worsen chronologically. The present study indicates that the degree of these biases is larger in the ALSFRS-R than in the other outcome measures of SBMA. Since this functional scale is evaluated by direct interview, its score may be easily affected by the subjectivity of patients and raters. This tendency has also been reported in a systemic review of clinical trials, where placebos demonstrated benefits in studies with continuous subjective outcomes, although they had no significant effects on objective outcomes [17]. Although the degree to which true progression, placebo effect, or negative expectations influence outcome measures is hardly estimated, it is of importance to understand what types of outcome measures tend to be vulnerable to placebo effects and negative expectations, when designing placebo-controlled interventional studies. Knowledge about these subjectivity-related biases is necessary for a correct choice of endpoints in clinical trials.
Although the 6MWD is merely a measure of walking capacity, the ALSFRS-R reflects the total motor function of patients, and thus has been widely used in clinical trials of motor neuron diseases [16, 30–32]. For rare diseases such as SBMA, natural history of motor function is indispensable for designing clinical trials. The data of untreated patients, however, should cautiously be used, given the results of the present study that functional scales such as the ALSFRS-R may have an innate subjectivity-related problem. Several different approaches could be used to overcome these concerns. For example, we should develop a new disease-specific outcome measure that is sensitive to changes in the severity of symptoms and has less intrinsic placebo-related effects. Functional scores in which questionnaires are defined with concrete descriptions and their deliberate inter-rater validation may attenuate subjectivity and mystification in interviews. A combination of subjective and objective measures may be considered. We may also need to construct a new class of clinical trials for neurodegenerative diseases that includes a third arm with no intervention and that avoids the inclusion of a placebo group [33].
In conclusion, placebo-treated and untreated SBMA patient groups demonstrated a large difference in the chronological analysis of a motor functional score, but not for an objective measure of walking capacity. These findings should be thoroughly considered when designing clinical trials for SBMA and other neurodegenerative diseases with a slow progression.
References
Kennedy WR, Alter M, Sung JH (1968) Progressive proximal spinal and bulbar muscular atrophy of late onset. A sex-linked recessive trait. Neurology 18:671–680
Sperfeld AD, Karitzky J, Brummer D et al (2002) X-linked bulbospinal neuronopathy: Kennedy disease. Arch Neurol 59:1921–1926
Sobue G, Hashizume Y, Mukai E, Hirayama M, Mitsuma T, Takahashi A (1989) X-linked recessive bulbospinal neuronopathy. A clinicopathological study. Brain 112(Pt 1):209–232
Atsuta N, Watanabe H, Ito M et al (2006) Natural history of spinal and bulbar muscular atrophy (SBMA): a study of 223 Japanese patients. Brain 129(Pt 6):1446–1455
La Spada AR, Wilson EM, Lubahn DB, Harding AE, Fischbeck KH (1991) Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. Nature 352:77–79
Fischbeck KH (1997) Kennedy disease. J Inherit Metab Dis 20:152–158
La Spada AR, Taylor JP (2010) Repeat expansion disease: progress and puzzles in disease pathogenesis. Nat Rev Genet 11:247–258
Sobue G, Doyu M, Kachi T et al (1993) Subclinical phenotypic expressions in heterozygous females of X-linked recessive bulbospinal neuronopathy. J Neurol Sci 117:74–78
Schmidt BJ, Greenberg CR, Allingham-Hawkins DJ, Spriggs EL (2002) Expression of X-linked bulbospinal muscular atrophy (Kennedy disease) in two homozygous women. Neurology 59:770–772
Katsuno M, Adachi H, Kume A et al (2002) Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35:843–854
Katsuno M, Adachi H, Doyu M et al (2003) Leuprorelin rescues polyglutamine-dependent phenotypes in a transgenic mouse model of spinal and bulbar muscular atrophy. Nat Med 9:768–773
Takeyama K, Ito S, Yamamoto A et al (2002) Androgen-dependent neurodegeneration by polyglutamine-expanded human androgen receptor in Drosophila. Neuron 35:855–864
Chevalier-Larsen ES, O’Brien CJ, Wang H et al (2004) Castration restores function and neurofilament alterations of aged symptomatic males in a transgenic mouse model of spinal and bulbar muscular atrophy. J Neurosci 24:4778–4786
Banno H, Adachi H, Katsuno M et al (2006) Mutant androgen receptor accumulation in spinal and bulbar muscular atrophy scrotal skin: a pathogenic marker. Ann Neurol 59:520–526
Banno H, Katsuno M, Suzuki K et al (2009) Phase 2 trial of leuprorelin in patients with spinal and bulbar muscular atrophy. Ann Neurol 65:140–150
Katsuno M, Banno H, Suzuki K et al (2010) Efficacy and safety of leuprorelin in patients with spinal and bulbar muscular atrophy (JASMITT study): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol 9:875–884
Hróbjartsson A, Gøtzsche PC (2001) Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med 344:1594–1602
Diederich NJ, Goetz CG (2008) The placebo treatments in neurosciences: new insights from clinical and neuroimaging studies. Neurology 71:677–684
The ALS (1996) CNTF treatment study (ACTS) phase I-II study group. The amyotrophic lateral sclerosis functional rating scale. Assessment of activities of daily living in patients with amyotrophic lateral sclerosis. Arch Neurol 53:141–147
Ohashi Y, Tashiro K, Itoyama Y et al (2001) Study of functional rating scale for amyotrophic lateral sclerosis: revised ALSFRS (ALSFRS-R) Japanese version. No To Shinkei 53:346–355
Jenkinson C, Fitzpatrick R, Brennan C, Bromberg M, Swash M (1999) Development and validation of a short measure of health status for individuals with amyotrophic lateral sclerosis/motor neurone disease: the ALSAQ-40. J Neurol 246(Suppl 3):III16–III21
Jenkinson C, Fitzpatrick R (2001) Reduced item set for the amyotrophic lateral sclerosis assessment questionnaire: development and validation of the ALSAQ-5. J Neurol Neurosurg Psychiatry 70:70–73
Yamaguchi T, Ohbu S, Saito M et al (2004) Validity and clinical applicability of the Japanese version of amyotrophic lateral sclerosis–assessment questionnaire 40 (ALSAQ-40). No To Shinkei 56:483–494
Besinger UA, Toyka KV, Hömberg M et al (1983) Myasthenia gravis: long-term correlation of binding and bungarotoxin blocking antibodies against acetylcholine receptors with changes in disease severity. Neurology 33:1316–1321
Takeuchi Y, Katsuno M, Banno H et al (2008) Walking capacity evaluated by the 6-minute walk test in spinal and bulbar muscular atrophy. Muscle Nerve 38:964–971
Montes J, McDermott MP, Martens WB et al (2010) Six-minute walk test demonstrates motor fatigue in spinal muscular atrophy. Neurology 74:833–838
Savci S, Inal-Ince D, Arikan H et al (2005) Six-minute walk distance as a measure of functional exercise capacity in multiple sclerosis. Disabil Rehabil 27:1365–1371
Doyu M, Sobue G, Mukai E, Kachi T, Yasuda T, Mitsuma T, Takahashi A (1992) Severity of X-linked recessive bulbospinal neuronopathy correlates with size of the tandem CAG repeat in androgen receptor gene. Ann Neurol 32:707–710
Rascol O (2009) “Disease-modification” trials in Parkinson disease: target populations, endpoints and study design. Neurology 72:S51–S58
de Carvalho M, Pinto S, Costa J, Evangelista T, Ohana B, Pinto A (2010) A randomized, placebo-controlled trial of memantine for functional disability in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 11:456–460
Pascuzzi RM, Shefner J, Chappell AS et al (2010) A phase II trial of talampanel in subjects with amyotrophic lateral sclerosis. Amyotroph Lateral Scler 11:266–271
Gordon PH, Moore DH, Miller RG et al (2007) Efficacy of minocycline in patients with amyotrophic lateral sclerosis: a phase III randomised trial. Lancet Neurol 6:1045–1053
Pollo A, Benedetti F (2009) The placebo response: neurobiological and clinical issues of neurological relevance. Prog Brain Res 175:283–294
Acknowledgments
We wish to thank all the JASMITT investigators for collecting data of PTG. We acknowledge and thank all patients and their families for participating in this study. We also acknowledge and wish to thank Hiroaki Oe and Shinya Sakai, the biostatisticians of EPS Co., Ltd., for statistical advice. This work was supported by the Program for Improvement of Research Environment for Young Researchers from Special Coordination Funds for Promoting Science and Technology (SCF) commissioned by the Ministry of Education, Culture, Sports, Science, and Technology of Japan; Grant-in-Aids from Ministry of Education, Culture, Sports, Science, and Technology of Japan (grant numbers 21689024 and 22110005); Large Scale Clinical Trial Network Project subsidized by the Ministry of Health, Labour and Welfare (MHLW) and supported by Health and Labour Sciences Research Grants, Japan; and JST, CREST, Japan.
Conflict of interest
G.S. has received research grant and honoraria from Takeda pharmaceuticals. All other authors declare that they have no conflict of interests.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hashizume, A., Katsuno, M., Banno, H. et al. Difference in chronological changes of outcome measures between untreated and placebo-treated patients of spinal and bulbar muscular atrophy. J Neurol 259, 712–719 (2012). https://doi.org/10.1007/s00415-011-6251-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6251-2