Abstract
Sodium blockade with lamotrigine is neuroprotective in animal models of central nervous system demyelination. This study evaluated the effect of lamotrigine on magnetisation transfer ratio (MTR), a putative magnetic resonance imaging measure of intact brain tissue, in a group of subjects with secondary progressive multiple sclerosis (MS). In addition, the utility of MTR measures for detecting change in clinically relevant pathology was evaluated. One hundred seventeen people attending the National Hospital for Neurology and Neurosurgery or the Royal Free Hospital, London, UK, were recruited into a double-blind, parallel-group trial. Subjects were randomly assigned by minimisation to receive lamotrigine (target dose 400 mg/day) or placebo for 2 years. Treating and assessing physicians and patients were masked to treatment allocation. Results of the primary endpoint, central cerebral volume, have been published elsewhere. Significant differences between the verum and placebo arms were seen in only two measures [normal appearing grey matter (NAGM) p = 0.036 and lesion peak height (PH) p = 0.004], and in both cases there was a greater reduction in MTR in the verum arm. Significant correlations were found of change in MS functional composite with all MTR measures except lesion and normal appearing white matter (NAWM) PH. However, the change in MTR measures over 2 years were small, with only NAGM mean (p = 0.001), lesion peak location (p = 0.11) and mean (p < 0.0001) changing significantly from baseline. These data did not show that lamotrigine was neuroprotective. The clinical correlation of MTR measures was consistent, but the responsiveness to change was limited.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetisation transfer imaging is a quantitative magnetic resonance imaging (MRI) technique which involves using an off-water-resonance radiofrequency pulse to saturate water molecules bound to larger complex molecules. Comparing pre- and post-saturation images gives the magnetisation transfer ratio (MTR), with a higher value corresponding to a higher concentration of complex molecules [1]. Higher MTR has been shown to correlate with the higher myelin and axonal content in both multiple sclerosis (MS) lesions and normal appearing white matter (NAWM) in post mortem samples [2, 3] and to correlate with N-acetyl aspartate, a spectroscopic marker of neuro-axonal content, in vivo [4]. MTR is therefore of particular interest in progressive MS, where neuro-axonal loss and grey matter damage have been shown to be prominent [5], and is a potentially useful marker of pathology in the evaluation of putative neuroprotective treatments.
One possible neuroprotective agent is lamotrigine, a sodium channel blocker that has been shown to ameliorate neurological dysfunction and prevent neuro-axonal loss in the experimental allergic encephalomyelitis (EAE) animal model [6]. It is thought that there is upregulation of voltage-gated sodium channels on demyelinated axons [7–9] and that subsequent intra-axonal sodium accumulation can lead to reversal of the sodium–calcium exchanger and cell death [10–12]. By blocking sodium entry it may be possible to prevent intra-axonal sodium accumulation, and through this mechanism lamotrigine may protect chronically demyelinated axons.
This study comprises data from a randomised, double-blinded, placebo-controlled trial of lamotrigine in secondary progressive MS. No significant difference of change in central cerebral volume, which was the primary end-point for the trial, was seen between the verum and placebo arms over the 2 years of the trial, although early reduction in a secondary, whole brain atrophy endpoint in the verum arm suggested that this may in part be due to an osmotic or anti-inflammatory effect of lamotrigine [13]. In this study we evaluated one of the secondary endpoints, comparing change in MTR measures in brain normal appearing white matter (NAWM), normal appearing grey matter (NAGM) and T2 hyperintense lesions over 2 years in a group of subjects with secondary progressive MS, the hypothesis being that, if lamotrigine were neuro-protective, one would see a greater reduction in MTR in the placebo group.
The data from the trial were also used to assess the utility of MTR as a measure of clinically relevant pathology in secondary progressive MS by calculating the responsiveness of MTR measures to change over a 24-month period, i.e. the longitudinal correlation of MTR measures with MS functional composite (MSFC) and the association of MTR measures with a sustained increase in expanded disability status scale (EDSS).
Methods
Subjects
This study comprises 117 subjects from a double-blinded, placebo-controlled trial of neuroprotection with lamotrigine in secondary progressive MS who had MRI and clinical assessment at baseline. Inclusion criteria for the trial were: age 18–65 years, EDSS 4.0–6.5, with documented progression rather than relapse being the principle cause of disability over the 2 years prior to the start of the trial. Exclusion criteria were: eligibility for disease-modifying treatment; contraindications to lamotrigine or MRI; severe concurrent medical problems not related to MS; pregnancy; severe temperature-dependent symptoms; exposure to sodium or calcium channel blocking drugs in the previous 2 weeks, corticosteroids in the previous 2 months, immunomodulatory drugs in the previous 6 months, or mitoxantrone in the previous year. From a list of 354 people with secondary progressive MS, who were patients at the National Hospital for Neurology and Neurosurgery (NHNN) or the Royal Free Hospital (RFH), London UK, and had expressed an interest in taking part in clinical trials, 124 were found to meet the eligibility criteria, of whom 120 consented to take part. Three subjects experienced severe progression of MS prior to baseline imaging and withdrew from the study.
Subjects were randomised using minimisation with a web-based protocol (http://www.thesealedenvelope.com, Sealed Envelope Ltd., London UK) into equal-sized parallel groups to take lamotrigine or visually identical placebo, escalated to the highest tolerated dose up to a maximum of 400 mg daily, for 24 months. Age (≤45 years and >45 years), sex, centre (NHNN or RFH), evaluating physician and EDSS (≤5.5 or ≥6.0) were the binary minimisation variables.
The trial was approved by the Joint University College London and University College London Hospitals Committee on the Ethics of Human Research. All participants gave written informed consent before entry into the study.
The target sample size of 48 patients per group was based on a power of 80% to detect a treatment effect of 60% reduction in the rate of loss of central cerebral volume at the 5% significance level. This was based on data from the placebo group of the European trial of interferon beta-1b in secondary progressive MS [14] allowing for a combined rate of loss to follow-up and non-adherence of 20%.
Clinical data
Clinical data were: EDSS and MSFC comprising 25 foot timed walk (TW), nine-hole peg tests (9HPT) and paced auditory serial addition test-3 s protocol (PASAT-3).
Clinical data were collected on all subjects at three time points: baseline, 12 and 24 months. All clinical data were collected by two physicians who underwent appropriate training prior to the start of the study. Where possible all data from a given subject were collected by the same investigator, an assessing physician, who was given no information about the subject’s clinical history [investigational medicinal product (IMP) dose, side-effects etc.]. Clinical data were collected at the NHNN, RFH or the nuclear magnetic resonance (NMR) unit in the Institute of Neurology (ION), UCL, London, UK.
Adherence to treatment was estimated by counting the number of returned tablets and measuring serum lamotrigine levels at each visit. Both physicians and subjects were blinded to treatment allocation and to the results of the serum lamotrigine levels.
MRI acquisition and analysis
MRI and clinical data presented in this study were acquired at baseline, 12 and 24 months. All MRI data were collected using a single 1.5-T MRI scanner (General Electric, Milwaukee, WI, USA) and analysed by two trained raters on Sunblade 150 workstations (Sun Microsystems, Mountain View, CA, USA). Appropriate quality assurance procedures, involving regular scanning of control subjects with no known neurological deficit and phantoms, were undertaken for the whole 24-month period in keeping with departmental policy.
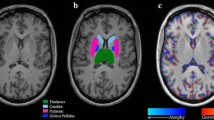
MTR histograms for T2 lesions, NAGM and NAWM were derived using four interleaved two-dimensional (2D) image sets each of 28 × 5 mm contiguous axial slices: PD, T2 weighted, with and without MT saturation—a total of 112 slices. Repetition time was 1,730 ms, echo time 30/80 ms, MT saturation pulse 14.6 µT, 64 ms in duration, 1 kHz off resonance, field of view 240 × 180 mm, matrix 256 × 128.
The grey matter–white matter contrast was too low on the images from the MTR sequence to allow accurate segmentation. Therefore, NAGM and NAWM masks were created using a three-dimensional (3D) T1-weighted fast-spoiled gradient recall inversion recovery (FSPGR-IR) scan: 124 contiguous 1.5 mm coronal slices, TR 10.9 ms, TE 4.2 ms, TI 450 ms. The images from the FSPGR-IR scans were reformatted to the same orientation and slice thickness as the MTR sequences and co-registered with the MTR images. NAWM and NAGM were then segmented using an automated segmentation tool—Statistical Parametric Mapping (SPM5) [15], which co-registers images to the Montreal Neurological Imaging group standard brain template (MNI152) [16], then calculates the probability for each voxel being white matter, grey matter or cerebrospinal fluid (CSF) depending on site and signal intensity. For this study a probability threshold of 75% was used. MTR, expressed as percentage units (pu), was then calculated for each voxel in the region covered by the masks. To minimise the contribution from partial volume voxels, we excluded any voxels with an arbitrary MTR value of <10 pu and also included a two-voxel erosion on the white matter segments and a one-voxel erosion for grey matter.
According to convention, MTR histograms are summarised using mean, mode [peak location (PL)] and the number of normalised brain units at the modal MTR value [peak height (PH)]. It is not known which is the most sensitive or specific measure for detecting clinically important pathology [17] so all three measures were included in the analysis and are reported below.
Statistics
Change in MRI and clinical measures
The change in MRI and clinical measures were calculated by subtracting baseline values from the values at 24 months, thus a negative value indicates a fall in that measure over 24 months; a negative value for the clinical measure indicated neurological deterioration. Paired Student’s t tests were used to determine whether any changes measured over 24 months were significant.
The effect of treatment with lamotrigine
Differences in change in MTR measures between the placebo and verum arms were assessed using independent samples Student’s t tests. Intention-to-treat analysis was used in this study, with all randomised subjects invited for every scan irrespective of whether they were still taking the investigational medicinal product. Two additional, post hoc, per protocol analyzes were employed: a comparison of tablet-adherent subjects, defined as those who had taken 80% of prescribed tablets and were still being prescribed tablets at 24 months; and a serum-adherent comparison, which compared subjects in the verum arm who had detectable serum lamotrigine at 24 months with the entire placebo arm. An 80% threshold for treatment adherence is widely used in clinical trials [18] and is in line with the lower levels of adherence seen with established disease-modifying treatments in MS [19].
Reliability of the MTR measures
The scan–reposition–rescan reproducibility of the MRI measures was estimated using MRI scans from three healthy controls, each of whom was scanned on five occasions over a 4-week period. Coefficients of variability were calculated for the MTR measures.
Longitudinal correlation between MTR measures and MSFC
Longitudinal correlation of MTR measures with MSFC and component scores was assessed in the placebo arm using a random intercept mixed effect linear regression model with age, gender, disease duration and time as covariates. A second model was calculated evaluating the correlation of MSFC with an interaction variable—[MTR measure] × time. The first model shows the correlation of MTR and clinical measures at any given time point. The second shows the correlation of the clinical measure with the change in the MTR measure.
The association between MTR measures and EDSS
Subjects in the placebo arm were divided into those who did or did not experience a sustained increase in EDSS over 24 months, defined as an increase of ≥0.5 points from baseline observed at two consecutive assessment visits over 6 months in subjects with baseline EDSS ≥6.0 or of 1.0 points in subjects with baseline EDSS ≤5.5. Differences in baseline MTR values and change in MTR were assessed using binary logistic regression with age, gender and disease duration as covariates.
Results
Recruitment started in January 2006 and lasted 8 months. The final 24-month scans were completed in September 2008. MRI data were collected on all subjects at baseline, 105 subjects (55 placebo, 50 verum) at 12 months and 108 subjects (56 placebo, 52 verum) at 24 months. Figure 1 is a participant flow diagram showing reasons for withdrawal and loss to follow-up. Baseline clinical and MRI measures are presented in Table 1; some of the demographic data have previously been published [13]. The mean absolute and annualised change in MTR measures are presented in Table 2. The change in clinical measures has been published previously [13].
Responsiveness and reproducibility
In the placebo arm, NAGM mean decreased over 24 months, but lesion PL and mean MTR both increased significantly; none of the other MTR measures changed over time (Table 2). The standardised response means (mean change/standard deviation of the change) were relatively low, ranging from 0.05 to 0.56, indicating limited responsiveness and signal-to-noise ratio.
The scan–reposition–rescan reproducibility of the MTR measures in the control group is shown in Table 3. The coefficient of variation was small, ranging from 0.16% to 2.54% with NAWM mean MTR the most reliable parameter. However, the variability still exceeded the mean annualised change in the trial study group (Table 2).
The effect of treatment with lamotrigine: intention-to-treat analysis
The results of Student’s t tests comparing change in MTR measures in the placebo and verum arms with intention-to-treat analysis are presented in Table 2. There were significant differences between the two groups in two parameters, NAGM PH and lesion PH. Both measures decreased in the verum arm, but did not change significantly in the placebo arm.
NAWM, NAGM and lesion PH also decreased significantly in the verum arm, while no significant change was seen in the placebo arm. However, the difference in change between the two groups was not significant for any of the three measures. Finally, there was a significant increase in lesion mean MTR in the verum arm, which was smaller than the corresponding increase seen in the placebo arm, but the difference between the two groups was not significant.
None of these results would support the hypothesis that lamotrigine was neuroprotective.
The effect of treatment with lamotrigine: per protocol analysis
At 24 months, 32 of 52 subjects in the verum arm were receiving lamotrigine (mean dose 78 mg) and 45 of 56 in the placebo arm (mean dose 240 mg) were tablet compliant (χ 2 p = 0.018). Twenty-five of 52 subjects in the verum arm were serum compliant [mean serum concentration 14.1 mg/L (standard deviation 8.6 mg/L)].
The results of the per protocol analysis were similar to the intention-to-treat analysis. In the ‘tablet-adherent’ analysis there was a significantly larger reduction of NAGM PH in the verum arm compared with the placebo arm (mean change −0.55%/pu versus 0.19%/pu, p = 0.005). There was mean decrease in lesion PH in the verum arm, compared with an increase in the placebo arm (−0.63%/pu versus −0.125/pu, p = 0.013), but there was a significantly smaller reduction of NAWM PH in the verum arm compared with the placebo arm (mean change −0.17 versus −1.44 pu, p = 0.028).
In the ‘serum-adherent’ analysis the only significant difference observed was for mean lesion PH, with a reduction in the verum arm (−0.52%/pu) compared with an increase in the placebo arm (0.16%/pu, p = 0.008).
Longitudinal correlations of MTR and MSFC measures
Longitudinal correlations of MTR measures with MSFC and component scores are shown in Table 4. The model used shows the correlation of the MTR measure with the clinical measure at any given time point, adjusting for age, sex and disease duration. There were significant correlations of PL and mean for all three tissue types with MSFC, PASAT-3 and 1/9HPT. NAGM mean was the only MTR parameter which correlated with 1/TW. In all cases the correlations were positive; i.e. the higher the MTR measure, the better the performance in the clinical measure.
Using the second model, significant correlations were seen of change in NAWM PH and mean with PASAT-3 (β = 0.009, p = 0.035, β = 0.011, p = 0.044) and of NAWM mean with 1/9HPT (β = 0.009, p = 0.026). In all cases the correlations were positive, indicating that an increase in the MTR measure was associated with better performance in the clinical task and a reduction in MTR with poorer performance in the clinical task.
Relationship of MTR measures with a sustained increase in EDSS
Eleven subjects in the placebo arm (20%) experienced a sustained increase in EDSS during the 24-month follow-up period. Change in two MTR variables was found to significantly predict those subjects who experienced an increase in EDSS; lesion MTR PL [p = 0.049, standardised odd ratio (OR) = 0.924] and lesion mean MTR were associated with a sustained increase in EDSS (p = 0.002, OR = 1.699). In both cases the baseline value was lower, although not significantly so, in the group that experienced a sustained increase in EDSS: PL 33.07 pu [standard error (SE) 0.22] versus 33.97 pu (SE 0.42, p = 0.07); mean 29.74 pu (SE 0.33) versus 30.71 pu (SE 0.35, p = 0.16); with a larger increase over 24 months in the group who did experience a sustained increase in EDSS: PL 0.97 pu (SE 0.42) versus 0.39 pu (SE 0.22, p = 0.25), mean 0.79 pu (SE 0.18) versus 0.30 (SE 0.10, p = 0.035). Graphs illustrating the change in lesion PL and mean in the two groups are shown in Fig. 2.
Discussion
The aim of this study was twofold, firstly to evaluate the neuroprotective potential of lamotrigine in secondary progressive MS and secondly to assess the utility of brain MTR measures (reproducibility, responsiveness to change and the longitudinal correlation of MTR measures with neurological function and disability) as a marker of brain pathology in clinical trials of MS.
Overall the results of the study do not show that lamotrigine has a neuroprotective effect. While the scan–reposition–rescan reproducibility in the non-MS controls was good, the magnitude of the change over time in the MS group was small compared with the variability, perhaps indicating that the responsiveness of MTR measures to change was relatively limited. There were significant correlations of MTR measures with measures of neurological impairment, indicating that MTR does detect clinically relevant brain pathology.
The effect of treatment with lamotrigine
The only measures differing significantly between the two treatment arms were lesion and NAGM MTR PH. In both cases there was a significantly greater decrease in MTR in the verum arm (in fact there was a non-significant increase in lesion PH in the placebo group). Since higher MTR is thought to represent higher myelinated axon content [2, 3, 20–22], treatment with a neuroprotective drug should have the opposite effect, i.e. a greater decrease in the placebo group. It is possible that lamotrigine is neurotoxic rather than neuroprotective and causes increased neuro-axonal damage. However, clinical data from this trial suggest relative preservation of neurological function in the verum arm [13], which would tend to refute this explanation.
Another possible explanation is that lamotrigine has another physiological effect on brain tissue, which results in a fall in MTR without a reduction in axonal number; for example, MTR has been shown to correlate with axonal expression of Na+/K+ ATPase in MS lesions [23]. Reduced axonal sodium content brought about through lamotrigine-mediated channel blockade could potentially lead to reduced expression of this enzyme and hence a fall in MTR. It would be interesting to evaluate this possibility in EAE, for example.
Responsiveness of MTR measures to change and reliability
The changes in MTR measures seen in this study were small compared with those reported from previous studies [24–26]. To minimise the contribution of partial volume voxels to the MTR histograms in this study, all voxels with MTR value <10 pu were excluded and an erosion was imposed on normal appearing brain tissue masks. The exclusion of this tissue from the histogram analysis may partly explain why MTR changes in this study were smaller than those in previously published reports.
The scan–reposition–rescan variability of MTR measures in the non-MS controls was good, being comparable to previously published values for whole brain MTR measures acquired using a similar MRI sequence [27]. However, the period over which scans were acquired in the MS group was markedly greater than that in the control group, and it is known that increasing lesion volume can also lead to changes in segmentation [28], so the variability caused by positioning and segmentation was likely to be somewhat higher in the MS subject group than in the non-MS controls.
Longitudinal association of MTR measures with MSFC and component measures
Despite the relatively limited sensitivity of MTR changes, there were still significant longitudinal correlations with clinical measures in the placebo arm.
Higher MTR in normal appearing brain tissue and lesion MTR was associated with poorer performance in the PASAT-3 and the 9HPT. Consistent correlation of NAGM and NAWM MTR with cognitive and arm function was previously seen in the baseline cross-sectional analysis [29] and has been observed in other study groups [20, 30–33]. It may represent neurological impairment due to neuro-axonal loss, particularly since grey and white matter volume and atrophy have also been shown to correlate with deficits in these areas of neurological function [34–38].
Correlation of MTR measures with mobility have also previously been reported [20, 31, 39]. Where tissue types have been analysed in isolation, it is primarily grey matter MTR measures which have been found to correlate with and predict mobility [24, 39, 40]. This study corroborates these findings, with only NAGM MTR mean correlating with TW. The consistent correlation of changing NAGM mean MTR with change in all three components of the MSFC highlights the likely importance of grey matter pathology in determining neurological dysfunction in secondary progressive MS.
Using the second model, looking at the association between change in MTR measures with performance in the MSFC and component measures, there were significant correlations observed of change in NAWM MTR mean and PH with performance in the PASAT-3 and 9HPT. These were all positive correlations, indicating that an increase in MTR was associated with better performance in the clinical test and a reduction in MTR with a poorer performance. However, the β values were very small, indicating that a very large reduction in MTR would be associated with a very small decrease in the clinical measure, and of 36 comparisons made, only 3 were significant, so one should not put too much weight on these findings.
Change in lesion MTR measures is associated with a sustained increase in EDSS
A larger increase in mean lesion MTR over 24 months was associated with an increased probability of a sustained increase in EDSS. This is a surprising result for two reasons: firstly one would not expect lesion MTR to increase in people with secondary progressive MS, and secondly it is the opposite of what of what one would expect if lesion MTR mean is a measure of myelinated axon content; a fall in mean MTR should correspond to an increase in disability.
One possible explanation for the increase in lesion MTR PH and PL in the placebo arm and MTR mean in both arms is that within lesions factors other than just the myelinated axon content, such as resolution of oedema or changes to the structure or function of axons, may influence MTR. In addition to low myelinated axon content, low MTR in lesions has been shown to be associated with larger axonal diameter [22], lower expression of Na+/K+ ATPase in demyelinated axons [23] and the presence of parenchymal T cell and chemokine expression in microglia and macrophages [7]. Hence, it is possible that those subjects who experienced a sustained increase in disability had higher levels of inflammation, axonal oedema and axonal dysfunction at baseline and that the increase in MTR represents resolving oedema and attrition of dysfunctional axons. The mean lesion MTR mean and PL were lower at baseline in those patients who experienced a sustained increase in EDSS than in those who did not, which would be consistent with this sort of process. However, the differences were not statistically significant, so one should not place too much emphasis on this result.
Limitations of the study
The main limitation of this study was the relative insensitivity of the MTR measures. MTR was a secondary end-point, and the power calculations were based on central cerebral volume change, which is more reproducible [41] and responsive [42]. Replicating the study with a larger population may generate more reliable results, but the magnitude of the change in MTR measures would remain very small. A recent study in relapsing-remitting MS suggests that specifically targeting new lesions may improve the sensitivity of MTR measures [43]. The lamotrigine trial was not optimised to detect inflammatory activity, one of the eligibility criteria was that subjects should be relatively free of disabling relapses for at least 2 years prior to recruitment and no gadolinium was given, making the identification of new lesions somewhat less certain, so we have decided not to do this. However, future studies of potentially neuroprotective drugs in relapsing-remitting MS employing MTR as one of the MRI measures would be advised to consider treating new and chronic lesions separately.
As previously reported [13] non-adherence in the verum arm was higher than expected and disproportionate to the placebo arm. This may have influenced the outcome of the study, but it is difficult to envisage a good way to prevent this.
Finally, the design of the study failed to take into account the possible unintended effects of the drug on the outcome measures. This is increasingly recognised as a problem in MS studies [44]. The use of cross-over study design or multiple assessments prior to the introduction of the IMP or after its withdrawal may allow investigators to differentiate the drug effects on neuro-axonal volume or inflammation, which one would expect to occur rapidly, from any effects on neuro-axonal survival, which one would expect to be a much slower process.
References
Wolff SD, Balaban RS (1989) Magnetization transfer contrast (MTC) and tissue water proton relaxation in vivo. Magn Reson Med 10:135–144
van Waesberghe JHTM, Kamphorst W, de Groot CJA, van Walderveen MAA, Castelijns JA, Ravid R, Lycklama a Nijeholt GJ, van der Valk P, Polman CH, Thompson AJ, Barkhof F (1999) Axonal loss in multiple sclerosis lesions: magnetic resonance imaging insights into substrates of disability. Ann Neurol 46:747–754
Schmierer K, Scaravelli F, Altmann DR, Barker GJ, Miller DH (2004) Magnetization transfer ratio and myelin in postmortem multiple sclerosis brain. Ann Neurol 56:407–415
Davie CA, Silver NC, Barker GJ, Tofts PS, Thompson AJ, McDonald WI, Miller DH (1999) Does the extent of axonal loss and demyelination from chronic lesions in multiple sclerosis correlate with the clinical subgroup? J Neuro Neurosurg Psychiatr 67:710–715
Kutzelnigg A, Luchinetti CF, Stadelman C, Bruck W, Rauschka H, Bermann M, Schmidbauer M, Parisi JE, Lassman H (2005) Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain 128:2705–2712
Bechtold DA, Miller SJ, Dawson AC, Sun Y, Kapoor R, Berry D, Smith KJ (2006) Axonal protection achieved in a model of multiple sclerosis using lamotrigine. J Neurol 253:1542–1551
Moll NM, Cossoy MB, Fisher E, Staugaitis SM, Tucky BH, Rietsch AM, Chang A, Fox RJ, Trapp BD, Ransohoff RM (2009) Imaging correlates of leukocyte accumulation and CXCR4/CXCL12 in multiple sclerosis. Arch Neurol 66:44–53
Smith KJ, Kapoor R, Hall SM, Davies M (2001) Electrically active axons degenerate when exposed to nitric oxide. Ann Neurol 49:470–476
Craner MJ, Lo AC, Black JA, Waxman SG (2003) Abnormal sodium channel distribution in optic nerve axons in a model of inflammatory demyelination. Brain 126:1552–1556
Stys PK, Waxman SG, Ransom BR (1992) Ionic mechanisms of anoxic injury in mammalian CNS white matter: role of Na+ channels and Na(+)-Ca2+ exchanger. J Neurosci 12:430–439
Kapoor R, Davies M, Blaker PA, Hall SM, Smith KJ (2003) Blockers of sodium and calcium entry protect axons from nitric oxide-mediated degeneration. Ann Neurol 53:174–180
Bechtold DA, Smith KJ (2005) Sodium mediated axonal degeneration in inflammatory demyelinating disease. J Neurol Sci 233:27–35
Kapoor R, Furby J, Hayton T, Smith KJ, Altmann DA, Brenner R, Chataway J, Hughes RAC, Miller DH (2010) A randomized controlled trial of neuroprotection with lamotrigine in secondary progressive multiple sclerosis. Lancet Neurol 9:681–688
Altmann, Jasperse B, Barkhof F, Beckmann K, Filippi M, Kappos LD, Molyneux P, Polman CH, Pozzilli C, Thompson AJ, Wagner K, Yousry TA, Miller DH (2009) Sample sizes for brain atrophy outcomes in trials for secondary progressive multiple sclerosis. Neurology 72:595–601
Ashburner J, Friston KJ (2005) Unified segmentation. NeuroImage 26:839–851
Evans AC, Collins DL, Mills SR, Brown ED, Kelly RL, Peters TM (1993) 3D statistical neuroanatomical models from 305 MRI volumes. In: Proceedings IEEE-Nuclear Science Symposium and Medical Imaging Conference, pp 1813–1817
Dehmeshki J, Ruto AC, Arridge S, Silver NC, Miller DH, Tofts PS (2001) Analysis of MTR histograms in multiple sclerosis using principle components and multiple discriminant analysis. Magn Reson Med 46:600–609
Robiner WN (2005) Enhancing adherence in clinical trials. Contemp Clin Trials 26:59–77
Bruce JM, Hancock LM, Lynch SG (2010) Objective adherence monitoring in multiple sclerosis: initial validation and association with self-report. Mult Scler 16:112–120
Barkhof F, Bruck W, De Groot CJA, Bergers E, Hulsof S, Geurts J, Polman CH (2003) Remyelinated lesions in multiple sclerosis. Arch Neurol 60:1073–1081
Vrenken H, Guerts JJG, Knol DL, Polman CH, Castelijns JS, Pouwels PJW, Barkhof F (2006) Normal appearing white matter changes vary with distance to lesions in multiple sclerosis. Am J Neuroradiol 27:2005–2011
Fisher E, Chang A, Fox RJ, Tkach JA, Svarovsky T, Nakamura K, Rudick RA, Trapp BD (2007) Imaging correlates of axonal swelling in chronic multiple sclerosis brains. Ann Neurol 62:219–228
Young EA, Fowler CD, Kidd GJ, Chang A, Rudick R, Fisher E, Trapp BD (2008) Imaging correlates of decreased axonal Na+/K+ ATPase in chronic multiple sclerosis lesions. Ann Neurol 63:428–435
Rocca MA, Mastronardo G, Rodegher M, Comi G, Filippi M (1999) Long-term changes of magnetization transfer-derived measures from patients with relapsing-remitting and secondary progressive multiple sclerosis. Am J Neuroradiol 20:821–827
Inglese M, van Easberghe JHTM, Rovaris M, Beckmann K, Barkhof F, Hahn D, Kappos L, Miller DH, Polman C, Pozilli C, Thompson AJ, Yousry TA, Wagner K, Comi C, Filippi M (2003) The effect of interferon β-1b on quantities derived from MT MRI in secondary progressive MS. Neurology 60:853–860
Rovaris M, Agosta F, Sormani MP, Inglese M, Martinelliu V, Comi G, Filippi M (2003) Conventional and magnetization transfer MRI predictors of clinical multiple sclerosis evolution: a medium-term follow-up study. Brain 126:2323–2332
Inglese M, Horsfield A, Filippi M (2001) Scan-rescan variation of measures derived from brain magnetization transfer ratio histograms obtained in healthy volunteers by use of a semi-interleaved magnetization transfer sequence. AJNR Am J Neuroradiol 22:681–684
Chard DT, Parker GJM, Griffin CMB, Thompson AJ, Miller DH (2002) The reproducibility and sensitivity of brain tissue volume measurements derived from an SPM-based segmentation methodology. J Magn Reson Imaging 5:259–267
Hayton T, Furby J, Smith KJ, Altmann, Brenner R, Chataway J, Hughes RAC, Hunter K, Tozer D, Miller DH, Kapoor R (2009) Grey matter magnetization transfer ratio independently correlates with neurological deficit in secondary progressive multiple sclerosis. J Neurol 256:427–435
Rovaris M, Filippi M, Minicucci L, Iannucci G, Santuccio G, Possa F, Comi G (2000) Cortical/subcortical disease burden and cognitive impairment in patients with multiple sclerosis. AJNR Am J Neuroradiol 21:402–408
Ramio-Torrenta L, Sastre Garriga J, Ingle GT, Davies GR, Ameen V, Miller DH, Thompson AJ (2006) Abnormalities in normal appearing tissues in early primary progressive multiple sclerosis and their relation to disability: a tissue specific magnetisation transfer study. J Neurol Neurosurg Psychiatr 77:40–45
Deloire MS, Salort E, Bonnet M, Arimone Y, Boudineau M, Amieva H, Barroso B, Ouallet JC, Pachai C, Galliaud E, Petry KG, Dousset V, Fabrigoule C, Brochet B (2005) Cognitive impairment as marker of diffuse brain abnormalities in early relapsing remitting multiple sclerosis. J Neurol Neurosurg Psychiatr 76:519–526
Davies GR, Ramio-Torrenta L, Hadjiprocopis A, Chard DT, Griffin CMB, Rashid W, Barker GJ, Kapoor R, Thompson AJ, Miller DH (2004) Evidence for grey matter MTR abnormality in minimally disabled patients with early relapsing-remitting multiple sclerosis. J Neurol Neurosurg Psychiatr 75:998–1002
Filippi M, Inglese M, Rovaris M, Sormani MP, Horsfield G, Iannucci G, Colombo B, Comi G (2000) Magnetization transfer imaging to monitor the evolution of MS: a 1-year follow-up. Neurology 55:940–946
Amato MP, Portaccio E, Goretti B, Zipoli V, Battaglini M, Bartolozzi ML, Stromillo ML, Guidi L, Siracusa G, Sorbi S, Federico A, De Stefano N (2007) Association of neocortical volume changes with cognitive deterioration in relapsing-remitting multiple sclerosis. Arch Neurol 64:1157–1161
Sanfilipo MP, Benedict RH, Weinstock-Guttman B, Bakshi R (2006) Gray and white matter brain atrophy and neuropsychological impairment in multiple sclerosis. Neurology 66:685–692
Morgen K, Sammer G, Courtney SM, Wolters T, Melchior H, Blecker CR, Oschmann P, Kaps M, Vaitl D (2006) Evidence for a direct association between cortical atrophy and cognitive impairment in relapsing-remitting MS. Neuroimage 30:891–898
Sastre-Garriga J, Arévalo MJ, Renom M, Alonso J, González I, Galán I, Montalban X, Rovira A (2009) Brain volumetry counterparts of cognitive impairment in patients with multiple sclerosis. J Neurol Sci 282:120–124
Fisniku LK, Cercignani M, Tozer D, Chard D, Jackson J, Miszkiel K, Schmierer K, Thompson A, Miller D (2009) Magnetisation transfer ratio abnormalities reflect clinically relevant grey matter damage in multiple sclerosis. Mult Scler 15:668–677
Agosta F, Rovaris M, Pagani E, Sormani MP, Comi G, Filippi M (2006) Magnetization transfer MRI metrics predict the accumulation of disability 8 years later in patients with multiple sclerosis. Brain 129:2620–2627
Losseff NA, Wang L, Lau HM, Yoo DS, Gawne-Cain ML, McDonald WI, Miller DH, Thompson AJ (1996) Progressive cerebral atrophy in multiple sclerosis. A serial MRI study. Brain 119:2009–2019
Furby J, Hayton T, Altmann D, Brenner R, Chataway J, Hughes RAC, Smith KJ, Miller DH, Kapoor R (2010) A longitudinal study of MRI-detected atrophy in secondary progressive multiple sclerosis. J Neurol 257:1508–1516
van del Elksamp IJ, Knol DL, Vrenken H, Karas G, Meijerman A, Filippi M, Kappos L, Fazekas F, Wagner K, Pohl C, Sandbrink R, Polman CH, Uitdehaag BMJ, Barkhof F (2010) Lesional magnetization transfer ratio a feasible outcome for remyelinating trials in multiple sclerosis. Mult Scler 16:660–669
Zivadinov R, Reder AT, Filippi M, Minagar A, Stüve O, Lassmann H, Racke MK, Dwyer MG, Frohman EM, Khan O (2008) Mechanisms of action of disease-modifying agents and brain volume changes in multiple sclerosis. Neurology 71:136–144
Acknowledgments
The authors would like to thank the radiographers in the NMR Research Unit at the Institute of Neurology, London and all the subjects who participated in the study. The authors would also like to thank Dr. M. Cercignani, Dr. D. Chard, Dr. G. Davies, Dr. K.T.M. Fernando, Dr. L. Fisniku, Prof. R.A.C. Hughes, Dr. Z. Khaleeli, Dr. A. Shenoy, Dr. D. Soon, Dr. J. Swanton and Dr. A. Traboulsee for their advice. This work was funded by the MS Society of Great Britain and Northern Ireland and was undertaken at UCLH/UCL, which received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme. Lamotrigine and placebo were purchased from GlaxoSmithKline UK Ltd. No third party had any involvement in study design, data analysis or interpretation.
Conflicts of interest
R.K. has received honoraria from Biogen Idec, Merck Serono, and MS Therapeutics for participation in scientific advisory boards, and travel or accommodation expenses have been covered by Biogen Idec, Merck Serono, and Teva. K.J.S. has received consultancy fees from Merck Serono, and has received support from the Brain Research Trust for preclinical work on sodium-channel blockade in inflammatory neuropathy. R.B. has received honoraria from Merck Serono for participation in advisory boards, and travel or accommodation expenses have been covered by Biogen Idec and Merck Serono. J.C. has received consultancy fees from Biogen Idec. For D.H.M., University College London Institute of Neurology has received payments for membership of multiple sclerosis trial advisory boards of Biogen Idec, Bayer Schering, GlaxoSmithKline, and Novartis; payments for consultancies with Biogen Idec, GlaxoSmithKline, and Novartis; honoraria from Biogen Idec, GlaxoSmithKline, Novartis, the National Institutes of Health, and the University of Texas Health Science Center; payments for travel or accommodation from Biogen Idec, the Consortium of MS Societies, and GlaxoSmithKline; and research grants from the MS Society (UK), Biogen Idec, Novartis, GlaxoSmithKline, Genzyme, and the National Institute for Health Research. J.F., T.H., K.H., D.J.T. and D.R.A. have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This trial is registered with ClinicalTrials.gov, NCT00257855.
Rights and permissions
About this article
Cite this article
Hayton, T., Furby, J., Smith, K.J. et al. Longitudinal changes in magnetisation transfer ratio in secondary progressive multiple sclerosis: data from a randomised placebo controlled trial of lamotrigine. J Neurol 259, 505–514 (2012). https://doi.org/10.1007/s00415-011-6212-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6212-9