Abstract
Amyotrophic lateral sclerosis (ALS) is a fatal neurological disease with motor neuron degeneration. Riluzole is the only available treatment. Two-thirds of ALS patients present with growth hormone (GH) deficiency. The aim of this study is to determine if add-on of GH to riluzole, with an individually regulated dose based on Insulin-like growth factor 1 (IGF-I) production, was able to reduce neuronal loss in the motor cortex, reduce mortality, and improve motor function of ALS patients. Patients with definite/probable ALS, in treatment with riluzole, aged 40–85 years, and with disease duration ≤3 years were enrolled. The study was randomized, placebo controlled, and double blind. Before treatment, patients were tested with a GH releasing hormone (GHRH) + arginine test. The initial dose of GH was 2 IU s.c. every other day, and was progressively increased to a maximum of 8 IU. Primary endpoint was N-acetylaspartate/(creatine + choline) (NAA/Cre + Cho) ratio in motor cortex assessed by magnetic resonance spectroscopy performed at months 0, 6, and 12. Secondary endpoints were mortality and ALS functional rating scale revised (ALSFRS-R). The NAA/(Cre + Cho) ratio decreased in all patients who completed the trial. No significant difference was noted between treated and placebo group. At baseline, although IGF-I levels were within the normal range, 73% of patients had GH deficiency, being severe in half of them. Compared with bulbar onset, spinal-onset patients showed more depressed GH response to the GHRH + arginine stimulation test (10.4 ± 7.0 versus 15.5 ± 8.1 ng/mL; p < 0.05). Insulin resistance [homeostasis model assessment of insulin resistance (HOMA-IR)] increased from 2.1 ± 1.0 at baseline to 4.6 ± 1.9 at 12 months (p < 0.001). Insulin-like growth factor (IGF) binding protein 3 (IGFBP-3) decreased from 8,435 ± 4,477 ng/mL at baseline to 3,250 ± 1,780 ng/mL at 12 months (p < 0.001). The results show that GH exerted no effect on cerebral NAA or clinical progression assessed by ALSFRS-R. Two-thirds of ALS patients had GH deficit, with higher levels in the bulbar-onset group. During follow-up, patients showed progressive increase in HOMA-IR and decrease in IGFBP-3 levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease resulting in death in the majority of patients. Treatment is confined to riluzole, which showed a significant but small effect on survival [1]. Two-thirds of ALS patients present with growth hormone (GH) deficiency [2]. Two clinical trials have been performed in ALS patients with s.c. administration of Insulin-like growth factor 1 (IGF-I), with negative results [3, 4]. A third trial was completed in 2008 and gave negative results [5]. Another trial with i.m. administration of methionyl GH (mGH) also gave negative results [6]. Limitations of this trial were the administration of mGH at a fixed dose, regardless of IGF-I status, the extremely variable age of the enrolled patients, and the unavailability of riluzole as a potential add-on drug to GH. Based on these considerations, we decided to test in ALS patients the effect of 1-year treatment with recombinant GH, at a variable dose, as add-on treatment to riluzole in a double-blind, placebo-controlled, randomized, phase II clinical trial.
Patients and methods
Trial design
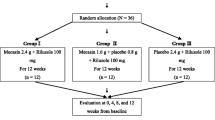
We designed a phase II, randomized, placebo-controlled, double-blind clinical trial to test the efficacy of 12-month treatment with GH (Saizen®; Merck Serono, Rome, Italy). Patients were stratified based on the ALS functional rating scale revised (ALSFRS-R) score (I, ≥36; II, <35) [7]. Each group was randomized with 1:1 ratio to treatment or placebo in blocks of two. GH or placebo was administered starting from 2 IU s.c. every other day (EOD). Doses were progressively increased to reach the target IGF-I levels of 435–580 ng/mL (1.5–2 times the upper limit of normal levels in our reference population) to a maximum allowed dose of 8 IU EOD. The primary objective of the study is to determine if GH slowed the rate of progression of neuronal loss in the primary motor cortex of ALS patients as compared with placebo after 12-month treatment. Secondary objective was the effect of treatment on the ALSFRS-R [7]. The scale ranges from 48 points in a healthy individual, to 0. Safety and tolerability were assessed by monitoring adverse events and laboratory parameters: routine biochemistry, hematocrit, and urine analysis. Patients attended the study center for screening and for eight additional visits.
Patients
The local Ethics Committee approved the clinical trial, which was registered at http://www.clinicaltrials.gov, no. NCT00635960. The trial was performed in accordance with the Declaration of Helsinki, European guidelines CPMP/ICH/135/95, and Italian law D.M. 15/07/1997. All patients gave written informed consent before any activity linked to the clinical trial was started. Inclusion criteria were definite/probable ALS according to El Escorial criteria, age 40–85 years, disease duration ≤3 years, and treatment with riluzole. Exclusion criteria were tracheostomy and/or gastrostomy, hepatic and/or renal failure, pregnancy and/or breastfeeding, signs of active neoplasm, complicated diabetes mellitus, severe hypertension, and inability to undergo magnetic resonance spectroscopy (MRS) examination. Sample size calculation was performed using a two-tailed paired t-test. Based on previous studies [8], the following considerations were made: expected mean value of NAA/(Cre + Cho) ratio to be reduced 30% less in the GH group compared with the placebo group, standard deviation of 0.1, type I error <0.05, and study power 90%. Accounting for up to 35% loss at follow-up, final sample size was set at 40 patients (20 treated and 20 placebos).
GHRH plus arginine test
All patients were tested with regard to their GH secretory status. GH releasing hormone (Geref®; Merck Serono S.p.A., Rome, Italy) was administered as i.v. bolus at the dose of 1 μg/kg of body weight (max. 100 μg), followed by arginine 30% (S.A.L.F., Bergamo, Italy) at fixed dose of 30 g i.v. over 30 min. Blood samples were obtained at 0, 15, 30, 45, 60, and 90 min. Severe GH deficiency was defined by a GH peak <9 ng/mL, and mild deficiency by a GH peak of 9–16 ng/mL.
Magnetic resonance spectroscopy (MRS)
MRS imaging was performed at 3 Tesla (Magnetom Trio; Siemens Medical Systems, Erlangen, Germany) using a two-dimensional spin-echo (2D-SE) technique with chemical shift selective water suppression (TE 270 ms, acquisition matrix 20 × 20, 15-mm-thick single slice positioned at the level of the centra semiovalia). For subsequent analysis, voxels immediately anterior to both central sulci were selected, and corresponding spectra were averaged. The resulting NAA peak integrals, normalized by the sum of choline and creatine, were then used as measures of upper motoneuron loss.
Hormone and metabolite assays
Serum samples were stored at −80°C until analysis. All samples were analyzed using the same assay lot. IGF-I, IGFBP-3, and insulin were measured by radioimmunoassay (Immunotech a.s., Prague, Czech Republic; DSL, Webster, Texas, USA). GH was measured by enzyme-linked immunosorbent assay (ELISA; Diasorin S.p.A., Vercelli, Italy). IGF-I, IGFBP-3, and insulin were also measured in 40 age- and sex-matched healthy controls. The homeostasis model assessment of insulin resistance (HOMA-IR) [9] was calculated with the formula HOMA-IR = fasting immunoreactive insulin in mU/L × fasting plasma glucose in mg/dl/405.
Statistical analysis
Per-protocol analysis was used for all endpoint variables. Continuous variables were analyzed by two-way analysis of variance (ANOVA) for repeated measures. Post hoc analysis was performed with the Bonferroni multiple-comparisons test or the Dunnett’s test to compare basal levels of the variables with those at various time points. Survival analysis was performed by Kaplan–Meier curve and using a Mantel–Cox test. p-Values <0.05 were considered statistically significant. Statistical analysis was performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Patients
A total of 45 patients were screened (Fig. 1) from March 2007 to July 2009. Forty patients were stratified and randomized to treatment: 24 male and 16 female, aged 62.7 ± 8.3 years, 26 of spinal and 14 of bulbar onset, with mean disease duration of 15.6 ± 10.6 months (Table 1). The treatment was well tolerated. One patient was excluded because of pre-existing liver cirrhosis that was not discovered during screening procedures. The most common reported side-effects during the trial were (number of events in parenthesis): increase of liver enzymes (15), joint swelling and stiffening (10), edema of lower limbs (3 events), hypertension (3), limb weakness (2), fasting glucose increase (2), and injection-site reactions (2). No difference in number of adverse events was observed between the treated and placebo group.
GHRH plus arginine test
GH releasing hormone (GHRH) + arginine tests were analyzed for 44 patients (28 male, 16 female; 28 of spinal and 16 of bulbar onset). Basal levels of GH were 0.43 ± 0.6 ng/mL. Twelve patients had normal GH response, whereas 32 (73%) had GH deficiency. Of these, 16 patients (36.4%) showed severe and 16 (36.4%) mild GH deficiency. Bulbar-onset patients showed higher levels of peak GH as compared with spinal onset (15.5 ± 8.1 versus 10.5 ± 7.0 ng/mL; p < 0.05; Fig. 2a). In addition, 13/28 (46%) of spinal-onset patients showed severe GH deficiency, whereas only 2/13 (14%) of bulbar-onset patients had severe GH deficiency (p < 0.05). No significant difference in GH response was observed between male and female patients (12.9 ± 6.4 versus 11.7 ± 9.7 ng/mL; p = 0.64). GH response did not correlate with disease severity or duration.
Hormonal data resulting from the clinical trial. a Plot of peak GH levels after GHRH + arginine stimulation in spinal- and bulbar-onset patients at baseline (box and whiskers with min. and max.). b Serum IGF-I levels in GH- and placebo-treated patients during the study. c Homeostasis model assessment of insulin resistance (HOMA-IR) and d IGFBP-3 levels at baseline, 6 and 12 months for GH- and placebo-treated patients (comparison with baseline: *p < 0.05; **p < 0.01; ***p < 0.001)
Study endpoints
At baseline, the values of the NAA/(Cre + Cho) ratio were 1.14 ± 0.2 for the treated and 1.19 ± 0.14 for the placebo group, showing no statistical difference (Fig. 3a; p = 0.56). At 6 months, NAA/(Cre + Cho) ratio was 1.12 ± 0.17 and 1.19 ± 0.15 in the GH and placebo group, respectively (p = 0.39). At 12 months, NAA/(Cre + Cho) ratio was 1.03 ± 0.15 in the GH and 1.19 ± 0.14 in the placebo group (p = 0.09). Pretreatment ALSFRS-R was 39.8 ± 4.4 for the treated and 37.0 ± 6.0 for the placebo group (Fig. 3b; p = 0.36). At 6 months, ALSFRS-R values were 35.2 ± 6.1 and 33.1 ± 7.8, respectively (p = 0.61), and at 12 months, 32.7 ± 7.3 and 31.1 ± 8.5, respectively (p = 0.63). During the study, five patients died, four in the GH and one in the placebo group (p = 0.20). Three cases of tracheostomy/gastrostomy were reported in each group. Patient stratification based on age, onset type, disease duration, basal ALSFRS-R values, and GH status prior to treatment did not show any difference between GH and placebo group in all endpoint variables (MRS, ALSFRS-R, and survival).
Hormonal data
Basal IGF-I levels were 126 ± 52 ng/mL for all patients, 127 ± 57 ng/mL for the treated, and 124 ± 48 ng/mL for the placebo group (p = 0.80). IGF-I levels were not different from a control group of healthy individuals (130 ± 53 ng/mL, p = 0.74) and were not correlated with GH secretory status. Since IGF-I target levels were not reached in any of the patients, GH or placebo was administered at the highest allowable dose of 8 IU EOD. Three months after treatment, IGF-I levels were statistically different between groups (181 ± 76 ng/mL versus 131 ± 40 ng/mL in the GH and placebo group, respectively; p < 0.05; Fig. 2b) and reached a peak at 9 months in the treated group (244 ± 88 versus 143 ± 58 ng/mL; p < 0.01). At 12 months the difference weakened and was no longer significant (207 ± 166 versus 162 ± 68 ng/mL; p = 0.46). Only one patient in the GH group reached the target IGF-I concentration with a value of 560 ng/mL at month 12. GH-deficient patients reached higher levels of IGF-I as compared with nondeficient patients at 9 months of treatment (317 ± 86 versus 208 ± 68 ng/mL; p < 0.02).
Insulin levels increased from 10.13 ± 4.6 mIU/L at baseline to 16.64 ± 8.2 mIU/L at 6 months (p < 0.001) and 21.28 ± 6.2 mIU/L at 12 months (p < 0.0001) for all patients. HOMA-IR increased from 2.12 ± 0.97 at baseline to 3.44 ± 1.92 at 6 months and to 4.56 ± 1.87 at 12 months (p < 0.001; Fig. 2c) for all patients. Fasting glucose levels were 81 ± 17 mg/dL at baseline, 87 ± 29 mg/dL at 6 months, and 87 ± 36 mg/dL at 12 months (p = 0.80). BMI was 25.7 ± 3.6 kg/m2 at baseline and 26.1 ± 3.8 kg/m2 at 12 months (p = 0.18).
Basal levels of IGFBP-3 were 8,435 ± 4,477 ng/mL in ALS patients and 4,352 ± 4,062 ng/mL in the control group (p < 0.0001). In the patient group, IGFBP-3 decreased to 4,138 ± 2,573 ng/mL at 6 months (p < 0.01) and to 3,250 ± 1,780 ng/mL at 12 months (p < 0.001; Fig. 2d).
No significant differences in the hormonal data were observed between the GH and placebo group, although GH patients showed a trend toward slower decline in IGFBP-3 values and more rapid increase in insulin and HOMA-IR index.
Discussion
We report the results of a 12-month randomized, placebo-controlled, double-blind clinical trial with recombinant GH in ALS patients. Overall, GH was well tolerated and safe, since few side-effects were observed and none of them could be linked to GH treatment. Our study failed to demonstrate an effect of GH on neuronal loss, motor function or disease progression in ALS patients. This was also evident in the subset of patients with impaired GH secretion. Therefore, we would not encourage either pharmacologic or substitutive GH treatment in ALS patients (class II/B evidence).
Our study reflects current interest in therapeutic use of recombinant GH and IGF-I in ALS patients. When the trial was started, data from the third IGF-I study were not available. Both the IGF-I and the GH trials, including the current one, failed to demonstrate any effect on survival or motor symptoms [3–6], indicating that GH and IGF-I are not to be considered for future clinical trials, despite the well-demonstrated neuroprotective effect of these molecules in cellular systems [10, 11] and increased survival in animal models [12].
Main differences between the trial of Smith et al. [6] using GH and the current one are the individually tailored dose of GH, based on peripheral IGF-I production, the enrollment of patients with ≤3 years disease duration, and the add-on of GH to riluzole. As for the individually tailored dose, our approach failed because of strong and unexpected GH resistance in ALS patients. Even though the dose of GH was raised to 8 IU EOD (maximum allowed dose) in all patients, only one patient reached the target IGF-I level at month 12 of treatment.
GH resistance has never been reported in ALS patients, and it was not evident in the previous GH trial [6]. Our data also show a clear dissociation between GH secretory status and IGF-I production in ALS. In support of this, basal IGF-I was perfectly normal in our patients despite impaired GH secretion in most of them. During disease progression, strong GH resistance develops, whereas IGF-I shows a trend towards increase in placebo-treated patients. An IGF-I generation test could help elucidate the time course and mechanisms of GH resistance in ALS [13].
In agreement with previous reports [2, 14], the majority of our ALS patients (73%) showed impaired GH secretion. Of these, half presented with severe GH deficit and half with mild GH deficit. In contrast, basal IGF-I levels were in the normal range and not different from control subjects, and secretory status was similar between males and females. Interestingly, we found that peak GH levels were higher in bulbar-onset patients compared with spinal onset, with higher prevalence of GH deficiency in spinal-onset ALS. It is difficult to explain the more severe deficiency in patients with a milder phenotype. Salvatore et al. [15] recently showed that patients with Huntington’s disease have impaired GH secretion. Similarly to our study, patients with milder phenotype had the lowest GH peak levels. This could be because of increased activation of GH secretion, as a protective mechanism, in severely affected patients.
Progressive insulin resistance (IR) developed in our ALS patients. IR was previously reported using the euglycemic insulin clamp technique and was interpreted as a primary carbohydrate aberration in ALS [16]. Recently, impaired glucose tolerance was found after oral glucose tolerance test [17], and was not associated with disease duration or severity. The causes of IR need to be addressed in future studies, and the role of reduced motor function and motility should be considered. What is clear from our data is that IR develops as an intrinsic feature of ALS, independent of GH treatment.
Previous cross-sectional studies in ALS patients showed normal IGFBP-3 levels as compared with controls [2, 13, 18–20]. In our study, basal levels of IGFBP-3 were increased in ALS patients, and this was an unexpected finding since GH deficit is usually associated with lower IGFBP-3 levels [21]. The effect of high IGFBP-3 levels is difficult to predict, but its apoptotic effect might contribute to the initial phase of ALS pathogenesis [22]. On the other side, IGFBP-3 decrease during disease progression may have multiple causes. Insulin is known to stimulate both IGF-I and IGFBP-3 synthesis [23], and strong insulin resistance develops during disease progression. In addition, circulating proteases, which are increased in serum and cerebrospinal fluid (CSF) from ALS patients [24], are known to reduce IGFBP-3 levels [25], and may play a role during ALS progression.
References
Bensimon G, Lacomblez L, Meininger V (1994) A controlled trial of riluzole in amyotrophic lateral sclerosis ALS/Riluzole Study Group. N Engl J Med 330:585–591
Morselli LL, Bongioanni P, Genovesi M et al (2006) Growth hormone secretion is impaired in amyotrophic lateral sclerosis. Clin Endocrinol (Oxf) 65:385–388
Lai EC, Felice KJ, Festoff BW et al (1997) Effect of recombinant human insulin-like growth factor-I on progression of ALS. A placebo-controlled study. The North America ALS/IGF-I Study Group. Neurology 49:1621–1630
Borasio GD, Robberecht W, Leigh PN et al (1998) A placebo-controlled trial of insulin-like growth factor-I in amyotrophic lateral sclerosis. European ALS/IGF-I Study Group. Neurology 51:583–586
Sorenson EJ, Windbank AJ, Mandrekar JN et al (2008) Subcutaneous IGF-1 is not beneficial in 2-year ALS trial. Neurology 71:1770–1775
Smith RA, Melmed S, Sherman B, Frane J, Munsat TL, Festoff BW (1993) Recombinant growth hormone treatment of amyotrophic lateral sclerosis. Muscle Nerve 16:624–633
Cedarbaum JM, Stambler N, Malta E et al (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169:13–21
Suhy J, Miller RG, Rule R et al (2002) Early detection and longitudinal changes in amyotrophic lateral sclerosis by (1)H MRSI. Neurology 58:773–779
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Aberg ND, Lind J, Isgaard J, Georg Kuhn H (2010) Peripheral growth hormone induces cell proliferation in the intect adult rat brain. Growth Horm IGF Res 20:264–269
Kaspar BK, Frost LM, Christian L, Umapathi P, Gage FH (2005) Synergy of Insulin-like growth factor-1 and exercise in amyotrophic lateral sclerosis. Ann Neurol 57:649–655
Kaspar BK, Lladlò J, Sherkat N, Rothstein JD, Gage FH (2003) Retrograde viral delivery of IGF-I prolongs survival in a mouse ALS model. Science 301:839–842
Buckway CK, Guevara-Aguirre J, Pratt KL, Burren CP, Rosenfeld RG (2001) The IGF-I generation test revised: a marker of GH sensitivity. JCEM 86:5176–5183
Pellecchia MT, Pivonello R, Monsurro MR et al (2010) The GH-IGF system in amyotrophic lateral sclerosis: correlations between pituitary GH secretion capacity, insulin-like growth factors and clinical features. Eur J Neurol 17:666–671
Salvatore E, Rinaldi C, Tucci T et al (2011) Growth hormone response to arginine test differentiates between two subgroups of Huntington’s disease patients. J Neurol Neurosurg Psychiatry 82:543–547
Reyes ET, Perurena OH, Festoff BW, Joegensen R, Moore WV (1984) Insulin resistance in amyotrophic lateral sclerosis. J Neurol Sci 63:317–324
Pradat PF, Bruneteau G, Gordon PH et al (2010) Impaired glucose tolerance in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler 11:166–171
Torres-Aleman I, Barrios V, Berciano J (1998) The peripheral insulin-like growth factor system in amyotrophic lateral sclerosis. Neurology 50:772–776
Corbo M, Lunetta C, Magni P et al (2010) Free insulin-like growth factor (IGF)-1 and IGF-binding proteins-2 and -3 in serum and cerebrospinal fluid of amyotrophic lateral sclerosis patients. Eur J Neurol 17:398–404
Hosback S, Hardiman O, Nolan CM et al (2007) Circulating insulin-like growth factors and related binding proteins are selectively altered in amyotrophic lateral sclerosis and multiple sclerosis. Growth Horm IGF Res 17:472–479
Olivecrona H, Hilding A, Ekstrom C et al (1999) Acute and short-term effects of growth hormone on insulin-like growth factors and their binding proteins: serum levels and hepatic messenger ribonucleic acid responses in humans. J Clin Endocrinol Metab 84:553–560
Butt AJ, Firth SM, King MA, Baxter RC (2000) Insulin-like growth factor binding protein-3 modulates expression of Bax and Bcl-2 and potentiates p53-independent radiation-induced apoptosis in human breast cancer cells. J Biol Chem 275:39174–39181
Liao L, Dearth RK, Zhou S, Britton OL, Lee AV, Xu J (2006) Liver-specific overexpression of the insulin-like growth factor-I enhances somatic growth and partially prevents the effects of growth hormone deficiency. Endocrinology 147:3877–3888
Niebroj-Dobosz I, Janik P, Soko-Çowska B, Kwiecinski H (2010) Matrix metalloproteinases and their tissue inhibitors in serum and cerebrospinal fluid of patients with amyotrophic lateral sclerosis. Eur J Neurol 17:226–231
Mitsui Y, Mochizuki S, Kodama T et al (2006) ADAM28 is overexpressed in human breast carcinomas: implications for carcinoma cell proliferation through cleavage of insulin-like growthfactorbindingprotein-3. Cancer Res 66:9913–9920
Acknowledgments
This study was supported by grants from Agenzia Italiana del Farmaco (no. FARM53XBKT), Ministero della Salute (progetto ordinario RF-SDN-2007-666932). We thank Merck Serono S.p.A. (Roma, Italy) for donating the study drug and blind packaging.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saccà, F., Quarantelli, M., Rinaldi, C. et al. A randomized controlled clinical trial of growth hormone in amyotrophic lateral sclerosis: clinical, neuroimaging, and hormonal results. J Neurol 259, 132–138 (2012). https://doi.org/10.1007/s00415-011-6146-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6146-2