Abstract
The aim of the study was to characterize the demographic, clinical, and prognostic features of Chinese patients with acute transverse myelitis (ATM). The clinical data from ATM patients in a demyelinating disease database were analyzed retrospectively. Sixty-seven ATM patients with a follow-up duration longer than 2 years were identified. The frequency of neuromyelitis optica-related ATM (NMO-ATM) was high in our cohort (40.3%). Recurrent ATM (R-ATM), with a female predominance, was common in total idiopathic ATM (69.0%, 20/29). In R-ATM with longitudinally extensive spinal cord lesions (LESCLs), the high seropositivity of NMO-IgG, spinal cord lesions mostly involved the central gray matter and severer long-term disability were similar to NMO-ATM. In RTM without LESCLs, low seropositivity of NMO-IgG, preferentially involvement of the peripheral white matter and relative better neurological recovery were consistent with multiple sclerosis-related ATM (MS-ATM). The transition rates to MS in patients with acute partial transverse myelitis (APTM) and acute complete transverse myelitis (ACTM) were not significant (16.7 vs. 6.3%, P = 0.753), while LESCLs (OR = 11.4, P = 0.028) were significantly correlated with transition to NMO. The presence of LESCLs was the only variable showing a higher risk for reaching Rankin 3 (hazard ratio: 2.5, 95% CI: 1.0–6.1). Chinese patients with ATM had demographic, clinical, and prognostic features different from those in Western populations. Idiopathic R-ATM, common in Chinese, is a heterogeneous entity that shares partial clinical, spinal MRI and prognostic features with MS-ATM and NMO-ATM. The length of spinal cord lesion, rather than APTM/ACTM, may be a prognostic factor associated with clinical outcome and long-term disability in our population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute transverse myelitis (ATM) is an inflammatory spinal cord disorder that has a variety of clinical manifestations, although the details of its pathogenesis are unknown in many cases [1]. There are several subtypes of ATM, such as those associated with multiple sclerosis (MS) [2], neuromyelitis optica (NMO) [3], systemic autoimmune disease [4], infection [5, 6], as well as cases with no specific origin (idiopathic ATM) [7]. Although ATM has been widely studied in the Caucasian population, the demographic, clinical, and prognostic features of ATM in Asian populations such as the Chinese have been rarely reported, and it is unclear whether they are distinct from those in Western patients. Therefore, a comprehensive evaluation of ATM in the Chinese, and in particular identification of clinical outcomes in the early stages of the disease, is particularly important for early clinical diagnosis, prognosis, and treatment.
Methods
Patients and classification
The MS Center of the Third Affiliated Hospital of Sun Yat-Sen University is one of the largest referral centers for MS and other demyelinating diseases in Southern China [8]. Potential ATM cases were identified by querying the patient database from January 1, 1995 to October 31, 2009 for a final diagnosis of myelopathy, myelitis, MS, or NMO. Patients were enrolled in the study if they fulfilled the inclusion and exclusion criteria for ATM proposed by the Transverse Myelitis Consortium Working Group (2002) [1]. In addition, all subjects must have had at least one follow-up visit at our Center more than 2 years after the onset of symptoms. Fulfillment of the inclusion and exclusion criteria was confirmed retrospectively by a review of medical records by two neurologists specialized in the demyelinating diseases (Xueqiang HU and Wei QIU).
ATM was subclassified as: (1) MS-related ATM (MS-ATM): patients with a diagnosis of definite MS [9]; (2) NMO-related ATM (NMO-ATM): patients with a diagnosis of NMO [10] (the 1999 Wingerchuk diagnostic criteria [3] was used for several cases due to the lack of NMO-IgG data); (3) systemic disease-related ATM (SD-ATM): patients with clinical evidence of systemic diseases; (4) infectious ATM: patients with serologic evidence of infection with, for example, herpes simplex virus (HSV) or varicella zoster virus (VZV); (5) monophasic ATM (M-ATM): patients with idiopathic ATM without relapses; (6) recurrent ATM (R-ATM): patients with idiopathic ATM who had suffered relapses, but without clinical evidence to permit a diagnosis of MS or NMO.
Based on the clinical and magnetic resonance imaging (MRI) findings, ATM patients were classified as having acute complete transverse myelitis (ACTM) or acute partial transverse myelitis (APTM) according to the definition by Scott et al. [11]. Longitudinal extensive spinal cord lesions (LESCLs) was defined as spinal cord lesions extending over three or more vertebral segments on spinal cord MRI [12]. Holocord lesion was defined as a spinal lesion occupying more than two-thirds of the cross-sectional area of the cord.
Clinical data
The patients’ medical records were reviewed retrospectively, and the following data were retrieved: gender, age at onset, disease duration, number of relapses, Modified Rankin Scale [13] at last visit, clinical manifestations, laboratory and MRI findings, and therapy including use of methylprednisolone, interferon-beta (INF-β), and/or immunosuppressants.
Laboratory tests
Systemic disease screening tests were performed as routine in most cases, including for anti-SSA/SSB antibody, antinuclear antibody, anti-dsDNA antibody, anti-sm antibody, anti-RNP antibody, anti-neutrophil cytoplasmic antibody, rheumatoid factor, and serology for infectious ATM such as antibodies to HSV-1, HSV-2, and VZV. Serum NMO-IgG antibodies were tested using aquaporin 4-transfected cells from a commercial sampling kit (EUROIMMUN AG, Lübeck, Germany) according to the manufacturer’s instructions. The sensitivity and specificity of NMO-IgG by this method for NMO patients in our cohort was 84.0 and 85.0%, respectively [8].
MRI scanning
All MRI scans were performed on a GE 1.5 T MR imager scanner (General Electric, Milwaukee, WI) in the Radiology Department of the Third Affiliated Hospital of Sun Yat-Sen University. The slice thickness of the axial scans ranged from 3–5 mm. The imaging parameters for the spinal cord MRI were as follows: T1 with and without gadolinium enhancement (400/15.5 ms, TR/TE), and T2 (2,500–3,500/100 ms, TR/TE). Most brain MRI scans were performed using T1, T2, proton density, and fluid attenuated inversion recovery (8,800–/120 ms, TR/TE) sequences.
Statistical analysis
Differences between the groups were assessed using analysis of variance, the 2-tailed t test, the Mann–Whitney test, or the Kruskal–Wallis test for quantitative variables, and the chi-squared test or Fisher’s exact test for categorical variables. Kaplan–Meier survival analysis was used for time-dependent outcomes, and differences between the survival curves were analyzed using the log-rank test. The correlation between categorical variables and outcomes was analyzed by the Cox regression test. P values <0.05 were considered statistically significant. Statistical analysis was performed using SPSS version 16.0 (Microsoft Corporation, San Francisco CA).
Results
Demographic features
Our database comprised 282 patients with demyelinating diseases who were diagnosed and managed from 1995 to 2009 in our MS center. As shown in Fig. 1, there were 67 ATM patients with a follow-up duration longer than 2 years finally enrolled in this study. Forty-four (65.7%) patients had the onset syndrome of ATM, and the other 23 (34.3%) patients were diagnosed during the disease course. Classification of ATM in our cohort was compared with that in other studies (Table 1). The proportion of NMO-ATM was markedly higher than that reported in western populations (40.3 vs. 0–27.1%). Interestingly, no cases with infectious ATM or SD-ATM were found in our cohort. All patients with ATM received intravenous methylprednisolone pulse therapy (1,000 mg/day for 3–5 days) in the acute phase. Immunosuppressants were used in 16 patients in the acute phase. INF-β was used in six patients in remission.
Clinical and laboratory findings
The clinical characteristics of the ATM subgroups are shown in Table 2. Male and elderly patients were more common than expected in the M-ATM group, but not in the R-ATM, NMO-ATM, or MS-ATM groups. Peak onset age was 40s in M-ATM, and 30s in R-ATM. R-ATM with LESCLs had a high positivity of NMO-IgG (75.0%) and poor long-term disability (54.5% in moderate or severe disability) which was comparable with NMO-ATM (90.0% NMO-IgG positive rate, and 48.1% in moderate or severe disability). Low seropositive rate of NMO-IgG (0) and relative better neurological recovery (11.1% in moderate or severe disability) in RTM without LESCLs were similar to those in MS-ATM (10.0% NMO-IgG positivity, and 18.2% in moderate or severe disability).
MRI features
Spinal cord MRI was undertaken in 45 ATM patients in the acute stage and 22 ATM patients in the remitting stage. One of 9 (11.1%) M-ATM and 15.0% (3/20) R-ATM had holocord lesions. Spinal cord lesions in the R-ATM without LESCLs group (66.7%), and the MS-ATM group (72.7%) mostly involved the peripheral white matter in the cervical cord (Table 2) (Fig. 2a, b). Spinal cord lesions in RTM with LESCLs (54.5%) and NMO-ATM group (63.0%) mostly involved the central gray matter (Fig. 2c).
Sagittal (upper) and axial (lower) distributions of spinal cord lesions in ATM subgroups. a Spinal cord lesion in an R-ATM patient without LESCLs that involved the peripheral cord. b Spinal cord lesion in an MS-ATM patient without LESCLs that involved the peripheral cord. c Spinal cord lesion in an NMO-ATM patient that involved the central cord. The lesions are shown by arrows. ATM Acute transverse myelitis, R-ATM recurrent ATM, LESCLs longitudinal extensive spinal cord lesions, MS-ATM multiple sclerosis related ATM, NMO-ATM neuromyelitis optica related ATM
Prognosis in ATM patients
Forty-four (65.7%) in a total of 67 patients had ATM as initial symptom. All of these 44 patients were followed up at least 2 years after their first episode of ATM: 20.5% (9/44) of patients did not show a second episode of neuroinflammation during the follow-up period; 45.5% (20/44) patients suffered relapses; 22.7% (10/44) developed NMO; 11.4% (5/44) converted to MS. The variables associated with conversion to NMO and MS are shown in Tables 3 and 4, respectively. Seropositivity for NMO-IgG (odds ratio (OR) = 15.4, P = 0.019) and the presence of LESCLs (OR = 11.4, P = 0.028) were significantly correlated with transition to NMO. Brain lesions fulfilling Barkhof criteria for MS increased risk for developing to MS (P = 0.001). There is not significant difference in the transition rates to MS in patients with APTM and ACTM (16.7 vs. 6.3%, P = 0.753).
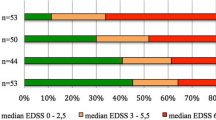
With regard to the disability, 14.9% (10/67) of patients made a full recovery (Rankin 0), 49.3% (33/67) had mild disability (Rankin 1–2), 19.4% (13/67) showed moderate disability (Rankin 3), and 16.4% (11/67) had severe disability (Rankin 4–6). Cox regression analysis was performed to investigate the factors (gender, age of onset, disease duration, ACTM, LESCLs, >1 spinal lesion, number of relapses, INF-β therapy) associated with reaching Rankin 3. The presence of LESCLs was the only variable showing a higher risk for reaching Rankin 3 (hazard ratio: 2.5, 95% CI: 1.0–6.1), and this risk was independent of the other variables (Table 5). Kaplan–Meier survival analysis showed that patients with LESCLs reached Rankin 3 faster than patients without LESCLs (7.5 vs. 10.5 years; log rank 5.1, P = 0.024) (Fig. 3). Moreover, the frequency of moderate or severe disability in patients with LESCLs was significantly higher than in those without LESCLs (17/35 vs. 7/32, OR = 3.4, P = 0.023).
Discussion
ATM is a clinical spectrum with heterogeneous etiologies. Clinical data from Chinese ATM patients is scarce. To our knowledge, this is the first study to investigate the demographic features, characteristics, and prognostic factors of ATM, including idiopathic and disease-related ATM, in the Chinese population.
The relative proportions of the different ATM subgroups in Asians were not well established. In our study, the proportion of NMO-ATM was markedly higher than that reported in the western populations [7, 14–17] and there were no cases of infectious ATM or SD-ATM. This may reflect the high prevalence of NMO in Asians. However, we should consider that selection bias caused by limited laboratory testing for infectious ATM may skew the data.
It has been reported that idiopathic ATM can affect any age, but has bimodal peaks between 10 and 19 years and between 30 and 39 years, with no sex predisposition [1, 18], and that the monophasic form (M-ATM) constitutes the majority of cases [19–22]. Idiopathic ATM on MRI is characterized by a centrally located high T2 signal lesion occupying more than two-thirds of the cross-sectional area of the cord, greater than three vertebral segments in length, with a predilection for the thoracolumbar cord [23, 24]. The present study showed some deviations from these reports in the clinical profiles of Chinese patients with idiopathic ATM: (1) M-ATM was found in only 31.0% (9/29) of idiopathic ATM patients, while R-ATM was common (69.0%, 20/29); (2) there was no peak age of onset between 10 and 19 years; (3) female predominance in R-ATM was different from other reports [25–27]; (4) spinal lesions occupying more than two-thirds of the cross-sectional area of the cord were rare, and only 11.1% (1/9) M-ATM patients and 15.0% (3/20) R-ATM had holocord lesions.
R-ATM has been referred to MS [14, 28], spinal cord-restricted NMO [29], or systemic disease [14], and only a small series of idiopathic R-ATM has been previously reported [25, 30, 31]. Three western studies reported that idiopathic R-ATM was different from classical MS [25, 27, 32], and recurrent longitudinal extensive myelitis (RLEM), with high serum positive rate for NMO-IgG antibodies was included in the NMO spectrum [29]. In contrast, in Asia, idiopathic R-ATM without extra-spinal lesions may be considered as spinal MS [33], and RLEM was different from spinal-restricted NMO [26, 34]. Therefore, the nosology of idiopathic R-ATM remains controversial. We speculate that idiopathic R-ATM, common in Chinese, is a heterogeneous entity that shares partial clinical, spinal MRI and prognostic features with MS-ATM and NMO-ATM. This conclusion was corroborated by : (1) In R-ATM with LESCLs, the high seropositivity rate of NMO-IgG, spinal cord lesions mostly involved the central gray matter and severer long-term disability were similar to NMO [12, 35]. It supported the western report that RLEM should be included in the NMO spectrum [29]; (2) Contrary to some clinical findings in the western reports [25, 27, 32], we did not find factors to differentiate RTM without LESCLs from MS-ATM, except of the onset age and frequency of Barkhof Brain lesions. Female predominance, low seropositivity of NMO-IgG, preferentially involvement of the peripheral white matter in cervical cord and relative better neurological recovery in these patients were consistent with MS-ATM. Some patients had multiple silent brain lesions. Therefore, we suspect that these R-ATM without LESCLs in our study most likely suffered from a unique inflammatory demyelinating disorder within MS but restricted to the spinal cord, though not fulfilling the Barkhof criteria.
The rate of transition to NMO after first-episode ATM has been reported to be low in Western countries (<1%) [36, 37]. However, a study from Hong Kong reported a higher rate of 9.4% [34]. Our findings were even higher than the latter, at 22.7%. In addition, we confirmed that seropositivity for NMO-IgG is predictive of subsequent conversion to NMO, while ATM with Barkhof brain lesions [38, 39] confers a high risk for conversion to MS.
According to some western reports, APTM/ACTM is somewhat related to the clinical outcomes of patients with an initial presentation of ATM [11, 36, 40–42]. Scott et al. [11] suggested that it may be beneficial to develop criteria for both APTM and ACTM. Their report did not focus on the length of the spinal lesion on MRI as a potentially important feature of prognosis in ATM patients, although it did mention that the spinal lesions of APTM on MRI tend to be smaller than those of ACTM; those of the latter generally extend over multiple cord levels. Our study suggests that the length of spinal cord lesion, rather than APTM/ACTM, may be a prognostic factor associated with clinical outcome and long-term disability. We did not confirm that APTM was associated with an increased risk of conversion to MS [11, 36, 40–42]. Interestingly, LESCLs were correlated with a higher risk of conversion to NMO (OR = 11.4, P = 0.028), and more ATM patients without LESCLs developed to MS (P = 0.014). In addition, the presence of LESCLs was the only prognostic factor associated with severer long-term disability in ATM patients. The fact that the length of the spinal cord lesions was more strongly correlated with clinical outcomes and long-term disability than APTM/ACTM implies that the classification of APTM and ACTM by Scott et al. [11] may be inappropriate for the Chinese population. We found a few APTM patients with LESCLs in our study, contrary to Western reports on APTM with smaller spinal cord lesions. It may partially explain the difference. A larger study with a longer follow-up period will be helpful in answering this question.
In conclusion, Chinese patients with ATM had demographic, clinical, and prognostic features different from those in Western populations. Idiopathic R-ATM, common in Chinese, is a heterogeneous entity that shares partial clinical, spinal MRI and prognostic features with MS-ATM and NMO-ATM. The length of spinal cord lesion, rather than APTM/ACTM, may be a prognostic factor associated with clinical outcome and long-term disability in our population.
References
TMCW Group (2002) Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology 59:499–505
Kahl KG, Naumann M, Oertele E, Warmuth-Metz M, Toyka KV (1998) Recurrent transverse myelitis. 2 cases and review of the literature. Nervenarzt 69:1115–1122
Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG (1999) The clinical course of neuromyelitis optica (Devic’s syndrome). Neurology 53:1107–1114
Mok CC, Lee KW, Wong RW, Lau CS (1999) Acute lupus myelitis affecting the clonus medullaris. Clin Exp Rheumatol 17:123–124
Weiss A, Brandl HG (1999) Cervical myelitis in herpes simplex virus (HSV) infections. Dtsch Med Wochenschr 124:781
Dodson D (1990) Transverse myelitis and spastic paraparesis in a patient with HIV infection. N Engl J Med 322:1322
Alvarenga MP, Thuler LC, Neto SP, Vasconcelos CC, Camargo SG, Papais-Alvarenga RM (2010) The clinical course of idiopathic acute transverse myelitis in patients from Rio de Janeiro. J Neurol 257:992–998
Lu Z, Qiu W, Zou Y, Lv K, Long Y, You W, Zheng X, Hu X (2010) Characteristic linear lesions and longitudinally extensive spinal cord lesions in Chinese patients with neuromyelitis optica. J Neurol Sci 293:92–96
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, Lublin FD, Metz LM, McFarland HF, O’Connor PW, Sandberg-Wollheim M, Thompson AJ, Weinshenker BG, Wolinsky JS (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 58:840–846
Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG (2006) Revised diagnostic criteria for neuromyelitis optica. Neurology 66:1485–1489
Scott TF, Kassab SL, Singh S (2005) Acute partial transverse myelitis with normal cerebral magnetic resonance imaging: transition rate to clinically definite multiple sclerosis. Mult Scler 11:373–377
Kira J (2008) Neuromyelitis optica and asian phenotype of multiple sclerosis. Ann N Y Acad Sci 1142:58–71
Roberts L, Counsell C (1998) Assessment of clinical outcomes in acute stroke trials. Stroke 29:986–991
de Seze J, Stojkovic T, Breteau G, Lucas C, Michon-Pasturel U, Gauvrit JY, Hachulla E, Mounier-Vehier F, Pruvo JP, Leys D, Destee A, Hatron PY, Vermersch P (2001) Acute myelopathies: clinical, laboratory and outcome profiles in 79 cases. Brain 124:1509–1521
Harzheim M, Schlegel U, Urbach H, Klockgether T, Schmidt S (2004) Discriminatory features of acute transverse myelitis: a retrospective analysis of 45 patients. J Neurol Sci 217:217–223
Jeffery DR, Mandler RN, Davis LE (1993) Transverse myelitis. Retrospective analysis of 33 cases, with differentiation of cases associated with multiple sclerosis and parainfectious events. Arch Neurol 50:532–535
de Seze J, Lanctin C, Lebrun C, Malikova I, Papeix C, Wiertlewski S, Pelletier J, Gout O, Clerc C, Moreau C, Defer G, Edan G, Dubas F, Vermersch P (2005) Idiopathic acute transverse myelitis: application of the recent diagnostic criteria. Neurology 65:1950–1953
Bhat A, Naguwa S, Cheema G, Gershwin ME (2010) The epidemiology of transverse myelitis. Autoimmun Rev 9:A395–A399
al Deeb SM, Yaqub BA, Bruyn GW, Biary NM (1997) Acute transverse myelitis. A localized form of postinfectious encephalomyelitis. Brain 120:1115–1122
Berman M, Feldman S, Alter M, Zilber N, Kahana E (1981) Acute transverse myelitis: incidence and etiologic considerations. Neurology 31:966–971
Christensen PB, Wermuth L, Hinge HH, Bomers K (1990) Clinical course and long-term prognosis of acute transverse myelopathy. Acta Neurol Scand 81:431–435
Prabhakar S, Syal P, Singh P, Lal V, Khandelwal N, Das CP (1999) Non-compressive myelopathy: clinical and radiological study. Neurol India 47:294–299
Andronikou S, Albuquerque-Jonathan G, Wilmshurst J, Hewlett R (2003) MRI findings in acute idiopathic transverse myelopathy in children. Pediatr Radiol 33:624–629
Choi KH, Lee KS, Chung SO, Park JM, Kim YJ, Kim HS, Shinn KS (1996) Idiopathic transverse myelitis: MR characteristics. AJNR Am J Neuroradiol 17:1151–1160
Kim KK (2003) Idiopathic recurrent transverse myelitis. Arch Neurol 60:1290–1294
Kim SH, Kim SM, Vincent A, Ahn SW, Hong YH, Park KS, Sung JJ, Lee KW (2010) Clinical characteristics, prognosis, and seropositivity to the anti-aquaporin-4 antibody in Korean patients with longitudinally extensive transverse myelitis. J Neurol 257:920–925
Ravaglia S, Bastianello S, Franciotta D, Ceroni M, Pichiecchio A, Tavazzi E, Moglia A, Marchioni E (2009) NMO-IgG-negative relapsing myelitis. Spinal Cord 47:531–537
Qiu W, Wu JS, Zhang MN, Matsushita T, Kira JI, Carroll WM, Mastaglia FL, Kermode AG (2010) Longitudinally extensive myelopathy in Caucasians: a West Australian study of 26 cases from the Perth Demyelinating Diseases Database. J Neurol Neurosurg Psychiatry 81:209–212
Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, Weinshenker BG (2007) The spectrum of neuromyelitis optica. Lancet Neurol 6:805–815
Seifert T, Enzinger C, Ropele S, Storch MK, Strasser-Fuchs S, Fazekas F (2005) Relapsing acute transverse myelitis: a specific entity. Eur J Neurol 12:681–684
Pandit L, Rao S (1996) Recurrent myelitis. J Neurol Neurosurg Psychiatry 60:336–338
Scott TF, Bhagavatula K, Snyder PJ, Chieffe C (1998) Transverse myelitis. Comparison with spinal cord presentations of multiple sclerosis. Neurology 50:429–433
Osoegawa M, Kira J, Fukazawa T, Fujihara K, Kikuchi S, Matsui M, Kohriyama T, Sobue G, Yamamura T, Itoyama Y, Saida T, Sakata K, Ochi H, Matsuoka T (2009) Temporal changes and geographical differences in multiple sclerosis phenotypes in Japanese: nationwide survey results over 30 years. Mult Scler 15:159–173
Chan KH, Tsang KL, Fong GC, Ho SL, Cheung RT, Mak W (2006) Idiopathic inflammatory demyelinating disorders after acute transverse myelitis. Eur J Neurol 13:862–868
Chan KH, Tsang KL, Fong GC, Cheung RT, Ho SL (2005) Idiopathic severe recurrent transverse myelitis: a restricted variant of neuromyelitis optica. Clin Neurol Neurosurg 107:132–135
Gajofatto A, Monaco S, Fiorini M, Zanusso G, Vedovello M, Rossi F, Turatti M, Benedetti MD (2010) Assessment of outcome predictors in first-episode acute myelitis: a retrospective study of 53 cases. Arch Neurol 67:724–730
Rubiera M, Rio J, Tintore M, Nos C, Rovira A, Tellez N, Montalban X (2006) Neuromyelitis optica diagnosis in clinically isolated syndromes suggestive of multiple sclerosis. Neurology 66:1568–1570
Barkhof F, Filippi M, Miller DH, Scheltens P, Campi A, Polman CH, Comi G, Ader HJ, Losseff N, Valk J (1997) Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain 120(Pt 11):2059–2069
Tintore M, Rovira A, Martinez MJ, Rio J, Diaz-Villoslada P, Brieva L, Borras C, Grive E, Capellades J, Montalban X (2000) Isolated demyelinating syndromes: comparison of different MR imaging criteria to predict conversion to clinically definite multiple sclerosis. AJNR Am J Neuroradiol 21:702–706
Cordonnier C, de Seze J, Breteau G, Ferriby D, Michelin E, Stojkovic T, Pruvo JP, Vermersch P (2003) Prospective study of patients presenting with acute partial transverse myelopathy. J Neurol 250:1447–1452
Sellner J, Luthi N, Buhler R, Gebhardt A, Findling O, Greeve I, Mattle HP (2008) Acute partial transverse myelitis: risk factors for conversion to multiple sclerosis. Eur J Neurol 15:398–405
Scott TF, Kassab SL, Pittock SJ (2006) Neuromyelitis optica IgG status in acute partial transverse myelitis. Arch Neurol 63:1398–1400
Acknowledgments
The study was supported by Technology Project of Guangzhou City (No. 2060402).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
R. Li and W. Qiu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, R., Qiu, W., Lu, Z. et al. Acute transverse myelitis in demyelinating diseases among the Chinese. J Neurol 258, 2206–2213 (2011). https://doi.org/10.1007/s00415-011-6093-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6093-y