Abstract
Despite the high relevance of emotion processing for social functioning, the study of the impairment of facial affect in multiple sclerosis (MS) has received little attention. Previous research reported evidence for emotion processing deficits but the nature and extent are not fully explained. Thirty-five MS patients underwent dedicated neuropsychological assessment of emotion processing using two facial affect recognition tasks and self-report measures of alexithymia. For comparison, healthy participants served as controls. Relative to healthy controls, MS patients were impaired in facial affect recognition on four of the six Ekman basic emotions, except happiness and disgust. The MS patients were more alexithymic than the healthy controls. These data provide evidence for deficits in the recognition of emotional face expressions and emotional introspection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ability to recognize emotions from facial expressions is crucial for social functioning in everyday life. More recently, it was shown that empathy is an important social skill involving the left inferior frontal and medial frontal cortex [1, 2]. Although mood impairments are common in MS [3], the study of emotion processing and its abnormalities in MS has received little attention.
MS is a progressive disease of the central nervous system primarily leading to white matter changes but involving the cerebral cortex as well [4]. In fact, the grey matter involvement and the loss of nerve fibers are considered to cause sensorimotor, visual, and cognitive deficits in chronic MS patients [5]. The first report on impairments in facial affect recognition in MS patients attributed them to a general impairment in facial perception [6]. More recently, it was argued that patients with MS have disturbances in emotion processing [7, 8]. Also, evidence was found for deficits in the identification of emotional states from prosodic cues [9]. Beyond results of impaired facial affect recognition, the presence of alexithymia was also advocated in MS patients [10]. Alexithymia is a dimensional normal distributed personality trait characterized by difficulties identifying, understanding, and describing emotions [11]. Previous research found the prevalence of alexithymia in French MS patients to be two times elevated as compared to the general population [12]. Furthermore, alexithymia has been found to be particularly present in patients with psychosomatic disorders [13]. Therefore, alexithymia may have a large impact on patients’ self-perception, regulation of emotion, control of behavior, and the interaction with other people.
Since MS patients are known to be impaired in regulation of emotion and, thus, in the control affective behavior we designed this study to examine the level of emotion processing in MS patients. Specifically we were interested in the performance test of facial affect recognition and self-report measures of emotion. We hypothesized that MS patients are impaired in recognizing emotions from human facial expressions. Also, we wished to explore if this socially relevant deficit is related to alexithymia in MS patients. To substantiate our hypotheses, MS patients’ data were compared to those of healthy controls.
Methods
Patients
In this prospective study, 42 patients with chronic MS were consecutively entered into the study between February 2008 and December 2009. Seven patients were excluded from data analysis due to pathological results on the Benton Facial Recognition Test (BFRT, see below). The large majority of the remaining MS patients (83%) suffered from secondary progressive MS, while five had relapsing remitting MS and one primary progressive MS. All patients received immunomodulatory treatment, predominantly mitoxantrone (80%) [14] but as well cyclophosphamide (9%), cortisone (9%) and natalizumab (3%). Mean years of disease duration was 9.2 years (SD 8.4). Patients’ age of symptom onset was 35.2 years (SD 11.1), and the mean age of diagnosis was 39.5 years (SD 12.2). The median score of the Expanded Disability Status Scale (EDSS) was 6.0 (range 0–7.5), indicating a “disability severe enough to preclude full daily activities” [15]. MS patients scored within the normal range on the Mini Mental Status Examination Test (MMSE) [16], M = 29.1, SD 1.2. Exclusion criteria were a deficit in the recognition of neutral facial expressions, indicated by a pathological score on the BFRT, an inability of writing and drawing with the dominant hand, as well as a history of major mental illness and a history of neurological disease other than MS. Healthy controls served as a control group. Descriptive statistics of the MS patients and the control group are presented in Table 1.
All of the participants gave informed written consent to participate in the study and none of the participants had visual disturbances that would interfere with testing. Experiments were approved by the local ethics committee and conducted according to the Declaration of Helsinki.
Procedure and measures
After providing demographic information, all participants completed self-report measures of depressiveness (BDI, Beck’s Depression Inventory) [17] and alexithymia (TAS-20, Toronto Alexithymia Scale) [11, 18]. MS patients completed the Benton Facial Recognition Test (BFRT) [19] measuring recognition of neutral faces from various perspectives and the Faces Symbol Test (FST) [20], a screening instrument for cognitive impairment in MS that requires drawing of easy-to-draw, simple geometric symbols beneath corresponding male and female heads.
To measure facial affect recognition, the Test of Perceptual Competence of Facial Affect Recognition (PCFAE, developed by Ingenhag, Schäfer and Franz in 2007, unpublished) and the Ekman-60-Faces test [21] were used. For PCFAE, participants were presented with a series of morphed faces showing emotional facial expressions of sadness, anger, fear, disgust, happiness or surprise on a computer screen in random order. Each morph sequence consisted of 30 images, each of which was presented for 750 ms. In each sequence, the facial expression slightly changed starting from a neutral expression to the fully developed expression of emotion. The faces were taken from the averaged Karolinska Directed Emotional Faces, http://www.facialstimuli.com/index_files/Page502.htm and every emotion was presented four times, twice with a female face and twice with a male face. Participants were required to press the space bar with their right index finger as soon as they had detected one of the six emotional expressions mentioned. Then they were asked to select the emotion by clicking at the corresponding label in a new window. If the space bar was not pressed until the end of the morph sequence, the selection window opened automatically. Thus, the PCFAE comprised two distinct measures: the number of correctly identified emotional expressions (accuracy) and the number of the image (1–30) shown when the emotion was detected (index image). As for the validity, significant correlations were found between the PCFAE and the Ekman-60-Faces-Test [21], r = 0.35. The reliability is specified with an internal consistency of 0.75 and a split-half reliability of 0.82 [22]. The Ekman-60-Faces test consisted of 60 faces of the Ekman and Friesen [21] series presenting the same six basic emotions. On a computer screen, each picture was presented for 5 s followed by a forced-choice menu to indicate the emotion detected.
Altogether, testing took between 1.5 and 2 h. Therefore, the order of tests was varied in a pseudorandom fashion across subjects.
Previously, the sample data were tested for normal distribution using the Kolmogorov–Smirnov test and homogeneity of variance using the Levene test. For comparison of the patient groups, a t test for independent samples with TAS-20 as the dependent variable and group as the independent variable and a Mann–Whitney U nonparametric test with BDI as the dependent and group as the independent variable were conducted. Additionally, a MANCOVA with group as the between-subjects variable, PCFAE accuracy (except sadness and surprise accuracy) and index scores, as well as the Ekman-60-Faces test score as within-subjects variables and age, education, BDI, and TAS-20 as covariates was conducted. Due to inhomogenity of variances, group differences for PCFAE accuracy sadness and surprise were tested with Kruskal–Wallis nonparametric test.
Results
In Table 2, the mean scores and the results of inferential statistical tests comparing MS patients and healthy controls are presented for the self-report measures BDI, TAS-20, FST, and BFRT.
The results of the t test and Mann–Whitney U test indicated significant group differences for BDI (p ≤ 0.001) and TAS-20 (p = 0.013), see Table 2 . MS patients were significantly more depressed compared to healthy controls. According to the cut-off scores, 17.1% of the MS patients were classified as depressed, 28.6% as moderately depressed, and 45.7% showed no signs of depression (8.6% missing). As expected, in the healthy control group, the majority (75.4%) had no mood disturbances. 21.3% were classified as moderately depressed and a minority of 3.3% showed signs of depression. Moreover, MS patients were significantly more alexithymic than healthy controls. In the MS group, 37.1% had low alexithymia, 37.1% had moderate alexithymia, and 25.7% had high alexithymia. Of the healthy controls, 23.0% had low alexithymia, 21.3% had moderate alexithymia, and 16.4% had high alexithymia (cut-off scores were calculated according to Franz et al. [11]). MS patients recognition of neutral faces was unimpaired as measured by the BFRT (80% normal range, 20% borderline). On the FST (information processing speed, working memory, sustained attention), patients scored below average.
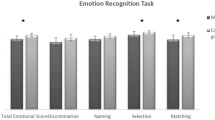
As Fig. 1 shows, the results of the MANCOVA and Kruskal–Wallis nonparametric test indicated significant main effects for the following PCFAE measures: total accuracy, fear accuracy, surprise accuracy, anger accuracy, sadness accuracy, total index, fear index, surprise index, anger index, sadness index, as well as the Ekman-60-Faces test (MANCOVA total accuracy F(5/93) = 4.23, p = 0.002; fear accuracy F(5/93) = 4.23, p = 0.002; anger accuracy F(5/93) = 5.16, p ≤ 0.001; total index F(5/93) = 2.99, p = 0.015; fear index F(5/93) = 3.14, p = 0.012; surprise index F(5/93) = 3.44, p = 0.007; anger index F(5/93) = 2.75, p = 0.024; sadness index F(5/93) = 3.01, p = 0.015; Ekman-60-Faces test F(5/93) = 5.68, p ≤ 0.001; Kruskal–Wallis test PCFAE sadness accuracy p = 0.003; surprise accuracy p = 0.017). The groups did not differ significantly in accuracy and indices of disgust and happiness. MS patients were less accurate on all PCFAE-measures mentioned above compared to healthy controls (Fig. 1). That was valid for the total scores as well as for fear, surprise, anger, and sadness separately. As for the response duration (index measures), MS patients detected emotional face expressions of fear and of surprise faster than healthy controls. Compared to healthy controls, MS patients’ response duration was slowed for sadness and anger. MS patients recognized significantly less facial expressions of emotion on the Ekman-60-Faces test compared to healthy controls.
Spearman correlation analysis between the PCFAE total scores and socio-demographic variables (age, education, symptom onset, diagnosis onset, and disease duration) and the other cognitive or emotional measures (BDI, TAS-20, MMSE, BFRT, FST) within the MS group yielded no significant correlations except for diagnosis onset (r = −0.335, p = 0.049) and the FST (r = −0.481, p = 0.015). The Ekman-60-Faces test was significantly correlated with education (r = 0.411, p = 0.008), age (r = −0.355, p = 0.037), diagnosis onset (r = −0.405, p = 0.016), symptom onset (r = −0.406, p = 0.017) and the PCFAE (r = 0.638, p ≤ 0.001).
To explore the relation of the impairment of facial affect recognition to the neurological impairment further, MS patients were divided into two subgroups according to their EDSS score (n = 9, EDSS ≤4 and n = 26, EDSS >4). Descriptively, MS patients with an EDSS >4 were slower on the FST, overall facial affect recognition (PCFAE total index) and recognition of disgust (PCFAE disgust index). Calculation of effect sizes yielded strong effects for FST (d = 0.95) and PCFAE disgust index (d = 0.84) and a moderate effect for PCFAE total index (d = 0.51), while no differences between groups were found by the Kruskal–Wallis test.
Discussion
The present study shows that patients with chronic MS and a moderate neurological deficit as assessed with the EDSS but normal neutral face recognition (BRFT) suffered from marked abnormalities of affect recognition in faces. As a group, the MS patients were more alexithymic than the healthy controls as measured by a self-report standardized questionnaire. Also, the MS patients made significantly more mistakes in both facial affect recognition tasks (PCFAE and Ekman-60-Faces test). In detail, MS patients performed less accurately than healthy controls on the PCFAE emotions fear, surprise, anger, and sadness, while they did not differ from healthy controls on disgust and happiness. The total percentage of errors was higher in MS patients compared to healthy controls. Compared to healthy controls, MS patients needed less time until they detected an emotion during the morphing sequence. In detail, response duration was speeded up when detection of fear and surprise was required and slowed when anger and sadness were presented. In general, our results are in line with recent findings of other authors [7, 23, 24], but they also extend those of others. To our knowledge, there is only one recently published study that examined facial affect recognition separately for six basic emotions and found a selective impairment in the detection of angry and fearful faces [8]. Our results show an impairment in detecting emotions from facial expressions, which might reflect the widespread lesions caused by MS. Similar lesion patterns might appear in other neurological or psychiatric conditions leading to similar impairment patterns. For example, there is evidence for deficits in emotion recognition in temporal lobe epilepsy with medial temporal sclerosis [25], Huntington’s disease [26], and dysfunctional theory of mind processing in Parkinson’s disease [27]. It should be noted, however, that our neurologically more severely affected MS patients fared less well in recognizing emotions in human face expressions than the neurologically less severely affected MS patients. This impairment, however, was not a general deficit of emotion processing or face recognition. Notably, this socially relevant impairment in recognizing emotions in human facial expressions was associated to alexithymia in the majority of our patients.
Moreover, the impairment in facial affect recognition can result from a general deficit in facial perception, as suggested by Beatty et al. [6], or reflect an impairment of emotion processing. None of the explanations can be ruled out completely by this study since we did not concentrate on the processing of neutral faces here. However, contrary to Beatty et al., our study only included MS patients who scored within the normal range of the Benton Facial Recognition Test. The deficit in our patients, therefore, argues for an emotional rather than a perceptual deficit. This is in line with results of neuroimaging studies examining the processing of emotional facial expressions. In a PET study, Kano et al. [28] found differential activation patterns in alexithymic versus normally empathic subjects while viewing emotional faces. In alexithymics, regional cerebral blood flow was decreased in the interior and middle frontal cortex, the orbitofrontal cortex, the inferior parietal cortex and the occipital cortex in the right hemisphere and increased in the superior frontal cortex, the inferior parietal cortex, and the cerebellum in the left hemisphere compared to normally empathic subjects. For angry and sad faces, a negative correlation was found between regional cerebral blood flow in the inferior and superior frontal cortices, the orbitofrontal cortex and parietal cortex in the right hemisphere, and TAS-20-scores. Other authors found alexithymia to be associated with less accurate performance in a facial recognition task [29]. Of the MS patients examined in our study, 26% were classified as highly alexithymic (37% as moderately alexithymic) but no significant correlations were found between alexithymia as measured by TAS-20 and facial affect recognition as assessed with the PCFAE and Ekman-60-Faces test. It appears likely that alexithymia and emotional face recognition result from only partly overlapping lesion patterns which have not been completely decoded yet. Clearly, there is a periventricular predominance of white matter lesions in MS affecting also the projections from the superior frontal gyrus. Nevertheless, the lesion patterns are known to be highly variable across MS patients affecting different projections in the differential neuronal networks underlying processing of empathy and recognition of emotional face expressions. This might explain why no correlations were found between emotion recognition and alexithymia in our MS sample.
It was suggested that a large-scale distributed network provides the basis for intact facial affect recognition [30]. Recent research provides evidence that white matter damage is able to impair recognition of emotions and that damage of association fiber tracts, such as the inferior fronto-occipital fasciculus and the inferior-longitudinal fasciculus leads to impairments in facial affect recognition by disrupting signal transduction between visual and emotion-related cortical areas [31]. Foci of inflammation are widespread throughout grey and white matter in MS [32], making it likely that these lesions also affect association fiber tracts and neuronal networks involved in the ability to recognize an emotion from a facial expression. Notably, patients with polyneuropathy differed neither from healthy controls nor from MS patients in the degree of alexithymia and facial affect recognition accuracy in general and for fear, anger, surprise, disgust and happiness as well as overall response duration while their response durations revealed differential changes in both directions (slower and faster). Unfortunately, they were older than our MS patients and healthy controls precluding definite conclusions.
There are limitations to the study. First, the sample size was relatively small. Second, as cognitive measures we used the MMSE, the BFRT, and the FST in our MS patients. The presence of memory impairment in MS has often been described [33, 34] and previous research found evidence for a correlation between facial affect recognition and information processing speed but not with measures of memory [8]. However, it appears unlikely that the results obtained here were confounded by such deficits. Our MS patients scored under average in the FST that measures different cognitive domains such as information processing speed, working memory and sustained attention. Although many MS patients suffered from motor impairments, this most likely did not influence the reaction time, since the patients had their fingers on the push button, which made their response easy and mainly driven by the speed of the morphing sequence. Rather, it should be noted that the FST scores significantly correlated with the PCFAE score. The PCFAE on the other hand did not require working memory capacity since directly after the proband detected an emotion he had to press the push button leading to a multiple choice menu to select the emotion opens automatically. Therefore, even if we had no further cognitive data except the FST, accuracy of the PCFAE appeared to be relatively independent from working memory function, information processing speed, and motor speed. The FST provided an insight into general cognitive performance including sustained attention. Although we cannot exclude that the sum of all these differences including depressiveness, age, and education was relevant for the impairment of our MS patients as evident in the FST, the patients were unimpaired in the recognition of neutral faces (BFRT). Moreover, the deficits in facial affect recognition were present in the PCFAE as well as in the Ekman-60-Faces test. Therefore, we would like to suggest that the impairment in the PCFAE and Ekman-60-Faces test in our MS patients was likely due to an impairment of emotion recognition.
Finally, with respect to the fact that our MS patients all received immunomodulative treatment and their disease duration was quite long (average 9.9 years), it would also be interesting for further research to assess facial affect recognition and alexithymia in earlier stages of the disease.
References
Seitz RJ, Nickel J, Azari NP (2006) Functional modularity of the medial prefrontal cortex: involvement in human empathy. Neuropsychology 20:743–751
Decety J, Jackson PL (2004) The functional architecture of human empathy. Behav Cogn Neurosci Rev 3:71–100
Nicholl CR, Lincoln NB, Francis VM, Stephan TF (2001) Assessment of emotional problems in people with multiple sclerosis. Clin Rehabil 15:657–668
Geurts JJG, Barkhof F (2008) Grey matter pathology in multiple sclerosis. Lancet Neurol 7:841–851
Grassiot B, Desgranges B, Eustache F et al (2009) Quantification and clinical relevance of brain atrophy in multiple sclerosis: a review. J Neurol 256:1397–1412
Beatty WW, Goodkin DE, Weir WS, Staton RD, Monson N, Beatty PA (1989) Affective judgements by patients with Parkinson’s disease or chronic progressive multiple sclerosis. Bull Psychon Soc 27:361–364
Krause M, Wendt J, Dressel A, Berneiser J, Kessler C, Hamm AO, Lotze M (2009) Prefrontal function associated with impaired emotion recognition in patients with multiple sclerosis. Beh Brain Res 205:280–285
Henry JD, Phillips LH, Beatty WW et al (2009) Evidence for deficits in facial affect recognition and theory of mind in multiple sclerosis. J Int Neuropsychol Soc 15:277–285
Beatty WW, Orbelo DM, Sorocco KH, Ross ED (2003) Comprehension of affective prosody in multiple sclerosis. Mult Scler 9:148–153
Montreuil M, Lyon-Caen O (1993) Troubles thymiques et relations entre alexithymie et dysfonctionnement inter hémisphérique dans la sclérose en plaques. Rev Neuropsychol 3:287–302
Franz M, Popp K, Schäfer R et al (2008) Alexithymia in the German general population. Soc Psychiatry Psychiatr Epidemiol 43:54–62
Chahraoui K, Pinoit JM, Viegas N, Adnet J, Bonin B, Moreau T (2008) Alexithymie et liens avec la depression et l’anxiété dans la sclérose en plaques. Rev Neurol 164:242–245
Pedrosa Gil F, Ridout N, Kessler H, Neuffer M, Schoechlin C, Traue HC, Nickel M (2008) Facial emotion recognition and alexithymia in adults with somatoform disorders. Depress Anxiety 26:E26–E33
Hartung HP, Gonsette R, Konig N et al (2002) Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind, randomised, multicentre trial. Lancet 360:2018–2025
Kurtzke J (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452
Kessler J, Markowitsch HJ, Denzler P (2000) Mini-Mental-Status-Test (MMST). Beltz Test GmbH, Göttingen
Hautzinger M, Bailer M, Worall H, Keller F (1995) Beck depressions-inventar (BDI) testhandbuch. Huber, Bern
Bagby RM, Parker JD, Taylor GJ (1994) The twenty-item Toronto alexithymia scale-I. Item selection and cross-validation of the factor structure. J Psychosom Res 38:23–32
Benton AL, Sivan AB, Hamsher K, Varney NR, Spreen O (1994) Contributions to neuropsychological assessment. Oxford University Press, New York
Scherer P, Penner IK, Rohr A et al (2007) The faces symbol test, a newly developed screening instrument to assess cognitive decline related to multiple sclerosis: first results of the Berlin Multi-Centre FST Validation Study. Mult Scler 13:402–411
Ekman P, Friesen W (1976) Pictures of facial affect. Consulting psychologists press, Palo Alto
Seidler D (2008) Evaluation und Validierung eines computergestützten Diagnostiktools zur Erfassung affektexpressiver Wahrnehmungskompetenzen. Diploma thesis; Bergische Universität Wuppertal, Germany
Banati M, Sandor J, Mike A (2009) Social cognition and theory of mind in patients with relapsing-remitting multiple sclerosis. Eur J Neurol 17:426–433
Jehna M, Neuper C, Petrovic K (2010) An exploratory study on emotion recognition in patients with a clinically isolated syndrome and multiple sclerosis. Clin Neurol Neurosurg 112:482–484
Meletti S, Benuzzi F, Rubboli G et al (2003) Impaired facial emotion recognition in early-onset right mesial temporal lobe epilepsy. Neurology 60:426–431
Johnson SA, Stout JC, Solomon AC et al (2007) Beyond disgust: impaired recognition of negative emotions prior to diagnosis in Huntington’s disease. Brain 130:1732–1744
Bodden ME, Dodel R, Kalbe E (2010) Theory of mind in Parkinson’s disease and related basal ganglia disorders: a systematic review. Mov Disord 25:13–27
Kano M, Fukudo S, Gyoba J (2003) Specific brain processing of facial expressions in people with alexithymia: an H 152 O-PET study. Brain 126:1474–1484
Jessimer M, Markham R (1997) Alexithymia: a right hemisphere dysfunction specific to recognition of certain facial expressions? Brain Cogn 34:246–258
Vuilleumier P (2005) How brains beware: neural mechanisms of emotional attention. Trends Cogn Sci 9:585–594
Philippi CL, Mehta S, Grabowski T et al (2009) Damage to association fiber tracts impairs recognition of the facial expression of emotion. J Neurosci 29:15089–15099
Bo L, Geurts JJ, Mork SJ, van der Valk P (2006) Grey matter pathology in multiple sclerosis. Acta Neurol Scand Suppl 183:48–50
Benedict RHB, Ramasamy D, Munschauer F, Weinstock-Guttmann B, Zivadinov R (2009) Memory impairment in multiple sclerosis: correlation with deep grey matter and mesial temporal atrophy. J Neurol Neurosurg Psychiatry 80:201–206
Amato MP, Ponziani G, Siracusa G, Sorbi S (2001) Cognitive dysfunction in early-onset multiple sclerosis—a reappraisal after 10 years. Arch Neurol 58:1602–1606
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prochnow, D., Donell, J., Schäfer, R. et al. Alexithymia and impaired facial affect recognition in multiple sclerosis. J Neurol 258, 1683–1688 (2011). https://doi.org/10.1007/s00415-011-6002-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6002-4