Abstract
Idiopathic intracranial hypertension (IIH) is a disorder of raised intracranial pressure (ICP) in the absence of identifiable pathology. The purpose of this study was to evaluate the clinical presentation and monitor a 3-month course using frequent optical coherence tomography (OCT) evaluations, visual field testings and lumbar opening pressure measurements. A longitudinal study of 17 patients with newly diagnosed IIH and 20 healthy overweight controls were included in the study. Peripapillary retinal nerve fiber layer thickness (RNFLT) and retinal thickness (RT) measurements (Stratus OCT-3, fast RNFL 3.4 protocol), and Humphrey visual field testing were evaluated at regular intervals. Repeat lumbar puncture was performed at final visit (n = 13). The diagnostic delay was 3 months and initial symptoms were headache (94%), visual blurring (82%) and pulsatile tinnitus (65%). Complete clinical remission was achieved in 65%, partial in 29% and unchanged symptoms in 6%. Total average RNFLT and RT decreased significantly during the follow-up period (p < 0.0001 and p < 0.0001, respectively). Changes in RNFLT and RT correlated with improvements in visual field mean deviation (MD) (RNFLT: p = 0.006; RT: p = 0.03) and pattern standard deviation (PSD) (RNFLT: p = 0.002; RT: p = 0.003). In patients with weight-loss >3.5% of BMI, ICP decreased significantly (p = 0.0003). In patients with weight-loss <3.5% of BMI, changes in ICP were insignificant (p = 0.6). OCT combined with visual field testing may be a valuable objective tool to monitor IIH patients and the short term IIH outcome is positive. Weight-loss is the main predictor of a favorable outcome with respect to CSF pressure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Idiopathic intracranial hypertension (IIH) is a disorder characterized by a raised intracranial pressure (ICP) in the absence of an identifiable neurological pathology [1, 2]. Symptoms and signs include headache, tinnitus, transient visual obscurations, blurred vision, diplopia and papilledema. Obesity, recent weight gain and female sex are risk factors for IIH, but the cause and pathophysiological mechanisms are still undetermined [3].
The natural history of IIH is variable. In some cases it is a self-limiting condition while in others, the ICP remains elevated for several years [3]. The potential chronic nature of the disease is associated with progressive optic nerve damage and irreversible visual defects.
Pharmacotherapy using acetazolamide is recommended to lower the intracranial pressure and thereby relieve symptoms and papilledema. Studies suggest that papilledema can be more readily controlled if weight-loss is achieved, but the association between weight loss and ICP reduction has not been established [4–10].
Most patients with IIH require careful follow-up to ensure appropriate treatment. Combined assessment of visual field function and disc morphology has long been appreciated for IIH. Optical coherence tomography (OCT) is a relatively new imaging technique allowing in vivo measurements of retinal layer thicknesses. It can quantify peripapillary retinal layers objectively which has improved the clinical evaluation of optic disc pathology although discrimination between axonal damage or resolution in papilledema is impossible. One previous study has demonstrated the use of OCT to follow-up chronic courses of papilledema (≥3 months) in adult IIH [11]. However, the value of OCT has not been shown during the initial 3-month period after diagnosis of IIH where close follow-up is mandatory.
This study had two aims: (1) To evaluate the initial 3-month course of a consecutive newly diagnosed IIH population using OCT and visual field testing and (2) to investigate the relationship between changes in CSF pressure and weight loss. These areas have not previously been studied.
Subjects and methods
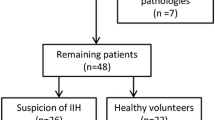
The study enrolled patients with confirmed IIH according to ICHD-II criteria for increased intracranial pressure (criteria B) [1]. Subjects were recruited from all patients with suspected IIH referred to the Danish Headache Centre in 2006–2008.
Inclusion criteria: age ≥18 years, high CSF-pressure (ICP >25 cmH2O if BMI >30 kg/m2; ICP >20 cmH2O if BMI ≤30 kg/m2), normal CSF composition, MRI and MR venography, and neurological examination except for papilledema and sixth nerve palsy [1]. Exclusion criteria: concurrent significant medical diseases, psychiatric diseases or ocular conditions.
After neurological screening, including direct ophthalmoscopy by the same physician, subjects underwent ophthalmologic examination comprising best-corrected visual acuity (Snellen), color vision testing (Ishihara), standard automated perimetry, applanation tonometry, optic disc photography and peripapillary mydriatic OCT. All subjects except one underwent ophthalmologic examinations in the morning (8–10 am) <2 h prior to lumbar puncture. This patient presented with rapid progressive symptoms and lumbar puncture prior to OCT examination was considered essential.
Treatment regimens including acetazolamide and dietary recommendations for weight-reduction were initiated after examinations. Medical dosage was individualized and limited to 2,250 mg/day. Medical therapy was regularly adjusted to relieve symptoms and papilledema and minimize side-effects. Furosemide (40–120 mg/day) combined with potassium was prescribed if acetazolamide was insufficient. When acetazolamide was not tolerated, topiramate was used as second-line treatment.
Subjects were offered a regular follow-up evaluation program comprising visits 1 week, 1, 2 and 3 months after diagnosis. During follow-up evaluations, OCT and automated perimetry were performed, body weight was recorded and medical dosage was adjusted if necessary. The 3-month follow-up evaluation also included detailed ophthalmological status and a subsequent lumbar puncture. Medical treatment was withheld for 72 h prior to this evaluation (1 week for subjects taking topiramate).
A control group of 20 healthy individuals was recruited through internet advertising for overweight research volunteers (age 18–65 years, BMI >25 kg/m2). Exclusion criteria: concurrent medical diseases or ocular conditions. Detailed information about lumbar puncture was given.
Data from patients and controls have been evaluated in a previous methodological study describing the reliability of OCT to identify IIH (Skau M, unpublished). The Ethics Committee of the Capital Region of Denmark approved this study. Written informed consent was obtained.
Standard automated perimetry
Standard automated perimetry (SAP) was performed (Humphrey Field Analyzer II, 30-2, SITA Fast). Subjects without prior experience did a one-minute test trial before the test. Criteria for reliable SAP results: <33% fixation losses, false negatives and false positives. Mean deviation (MD) and pattern standard deviation (PSD) were recorded.
Optical coherence tomography
OCT (Stratus OCT 3000, software 4.01; Carl Zeiss Meditec, Dublin, USA) was performed using the Fast 3.4 RNFL algorithm. Fast RNFL scans consisted of three peripapillary scans (256 A-scans each) with a diameter of 3.4 mm. A minimum of two well-centered Fast RNFL scans were obtained from each eye. Retinal nerve fiber layer thickness (RNFLT) and total retinal thickness (RT) were automatically derived by the OCT software (Fig. 1) [12, 13].
OCT images of papilledema in IIH. a Peripapillary RNFL thickness analysis. White lines outline RNFL: vitreoretinal interface (one arrow) and posterior border of the RNFL to the ganglion cell layer (two arrows). b Peripapillary RT thickness analysis. White lines outline RT: vitreoretinal interface (one arrow) and junction of the inner and outer segment of the photoreceptors (three arrows)
All peripapillary scans were subjectively assessed by the same person. The best peripapillary scan based on signal quality for each eye was selected for further data analyses. Where boundary detection of the algorithm failed in a localized area of the scan circle, thickness was determined manually for the concerning A-scans using the software precursor tools and the corrected mean thickness calculated. Averaged A-scan measurements of the total peripapillary scan circle were used for data analyses (total RNFLT, total RT).
Fundus photos
Fundus photos were evaluated qualitatively post hoc by two experienced neuro-ophthalmologists. Papilledema was classified according to Frisén [14].
Intracranial pressure
Lumbar puncture was performed using standard 20-gauge spinal needles (18-gauge needles if extensive lumbar adipose tissue was present). Opening pressure was measured while the subject was placed in a lateral decubital position with legs and spine extended, head and spine strictly horizontal and as relaxed as possible. Sufficient time was allowed for the pressure to stabilize. Subsequently, 10–15 mL CSF was removed for analysis. All but one lumbar puncture were performed by the same experienced physician. Subjects were all awake and not sedated.
Data analysis
Demographic data were summarized. Differences between patients and controls were investigated by t-test for age and BMI, chi-squared test for gender, and non-parametric 2-sided Mann–Whitney test for ICP. Wilcoxon sign test for matched pairs and paired t-test were used to compare ICP and BMI, respectively, at baseline and final follow-up. Association between ICP and BMI changes were analyzed by linear regression.
Interocular mean values were used for analyses. At presentation, retinal layers could not be quantified in some patients because of very severe papilledema. Evaluation of these scans indicated that RNFLT and RT were markedly increased. Given cases with immeasurable retinal layers at presentation, nonparametric tests were used for analysis of OCT data. Wilcoxon sign test for matched pairs was used to compare OCT measures at baseline and final follow-up and Mann–Whitney test to compare groups. Paired t-test was used to compare values of Snellen (logMAR), MD, PSD and Ishihara between baseline and follow-up, and t-test was used to compare groups. Correlations between OCT and visual field data were evaluated by nonparametric Spearman’s correlation analysis. Level of significance was considered for p < 0.05.
Results
Twenty patients and 20 controls were recruited; 3 patients (1 man, 2 women) were noncompliant with their follow-ups and were excluded. In all, data from 17 patients were analyzed. Characteristics of subjects and controls are presented in Table 1.
On presentation, headache was present in 16 patients (94%). Additional symptoms included visual blurring (82%), pulsatile tinnitus (65%), photophobia (53%), retrobulbar pain (47%), nausea (47%), dizziness (47%), subjective memory disturbances (47%), diplopia (41%), phonophobia (35%), transient visual obscurations (24%) and vomiting (24%). Median duration between initial symptoms and diagnosis was 3 months (range 1 week to >5 years).
No control subjects had pulsatile tinnitus, visual disturbances and chronic headache. Episodic migraine (≤2 episodes/year) and frequent, episodic tension-type headache (1–14 episodes/month) were reported by 3 and 4 controls, respectively [1].
Clinical data at baseline are presented in Table 2. Direct ophthalmoscopy revealed bilateral and unilateral papilledema in 13 and 1 patients, respectively; median edema grade 2 (range 0–4, interocular mean). Clinically, 3 patients revealed no papilledema but presented with characteristic symptoms and CSF-pressure of 26.0, 28.0 and 39.5 cmH2O. Due to severe papilledema, RNFLT and RT could not be measured in 4 and 3 patients, respectively. In measurable eyes, mean total RNFLT was 169.2 ± 80 μm and mean total RT was 438.2 ± 203 μm.
Median follow-up period was 93 days (range 81–140) over a total number of 2, 4 and 5 visits for 3, 3 and 11 subjects, respectively. Acetazolamide was initiated at median 1.5 g/day (range 0.5–2.25) and the median number of dosage changes during the follow-up period was 2 (range 0–3). Remission of symptoms was recorded in 11 patients, while 5 reported reduction in frequency or severity of symptoms. One patient reported unchanged symptoms and discontinued therapy. After 3-month follow-up, the median acetazolamide dosage was 1.5 g/day (0–2.25). Two subjects had stopped their medication, 1 took additional 80 mg/day furosemide, and 1 was switched to topiramate 50 mg/day. During the medical withdrawal before the final follow-up visit, 10 patients remained asymptomatic, 6 experienced recurrent or increased symptoms and 1 patient did not experience any change of existing symptoms.
During follow-up, patients improved significantly in OCT parameters and visual field sensitivity (Fig. 2; Table 2). At the final visit, total RNFLT and RT were above the 95% CI of controls in 16/34 eyes (47.1%, RNFLT) and 15/34 eyes (44.1%, RT) compared with 26/34 (76.5%, RNFLT) and 29/34 (85.3%, RT) at presentation.
Changes in MD and PSD from baseline to the final visit correlated significantly with OCT changes (RNFLT vs. MD: r = −0.77, p = 0.006; RT vs. MD: r = −0.63, p = 0.03; RNFLT vs. PSD: r = 0.83, p = 0.002; RT vs. PSD: r = 0.77, p = 0.003).
A second lumbar puncture was performed after 3 months in 13/17 patients. Median CSF-pressure drop from 31.0 cmH2O (range 23.4 to >50) to 24.0 cmH2O (20.2–42.5) (p = 0.02). Mean BMI decreased from 33.4 kg/m2 (range 26.1–44.1) to 31.1 kg/m2 (23.5–44.1) (p = 0.005). RNFLT changed from median 133 μm (range 98 μm to immeasurable) to 104 μm (87–179) (p = 0.0002). RT decreased from median 328.5 μm (274 μm to immeasurable) to 277 μm (254–409) (p = 0.0002).
There was a positive linear association between the proportional change in BMI and ICP (b = 5.2 (cmH2O m2)/kg, p = 0.0002) (Fig. 3). As illustrated in Fig. 3, patient data tend to segregate into two subgroups with a proportional change in BMI either below or above 3.5%.
Post-hoc analysis revealed that patients with a weight-reduction lower than 3.5% BMI (n = 6) had continuously elevated CSF-pressure at follow-up evaluation from median 29.0 cmH2O (range 23.4 to >50) to median 32.0 cmH2O (23.2–42.5) (p = 0.6). In contrast, CSF-pressure changed from median 34.5 cmH2O (29.0–46.0) to 21.0 cmH2O (20.2–24.5) in patients with a BMI change >3.5% (p = 0.0003). In the latter group, ICP was normalized in 3/7 according to ICHD-II criteria [1]. No significant differences in RNFLT, RT and MD could be identified between the two subgroups during baseline, final visit or across time.
Discussion
The present study confirmed a positive, short term outcome of IIH, the reliability of OCT to monitor optic disc changes and for the first time also in the initial phases of IIH. This imaging technology allowed quantification of optic disc changes related to resolution of papilledema during regulated medical therapy. Reduction in papilledema was shown to coincide with improvement in visual field sensitivity. Weight-loss greater than 3.5% of BMI was related to a significant reduction in CSF opening pressure after 3 months.
At baseline, average RNFLT and RT in our patient sample were significantly higher compared with controls. Our baseline RNFLT data are comparable with the data of 22 recently diagnosed IIH patients presented by Rebolleda et al. [11]. In our study, mean RNFLT was above normal in 76% eyes compared to 73% eyes in the study of Rebolleda et al. [11].
Application of total RT to follow-up papilledema has not been presented previously. We hypothesize that RT is an additional and more reliable estimator of severe papilledemas than RNFLT. When RNLF thickens in papilledema, absorption and scatter increase relative to the directly backwards reflected light resulting in reduced signal to noise ratio [15, 16]. This may impair the ability to define the posterior border of the RNFL towards the hyporeflective ganglion cell layer correctly, thus leading to an underestimation of RNFLT for increasingly severe cases of papilledemas. Future OCT studies are needed to evaluate this hypothesis.
Peripapillary OCT measurements declined rapidly in the first 2 months, indicating regression of papilledema. Although RNFLT and RT were above 95% CI of controls in 47 and 44% eyes, respectively, differences between subject and control groups were insignificant during follow-up. In the study of Rebolleda et al. [11], mean average RNFLT was classified as normal in 90.9% of eyes after one year. Unlike Rebolleda’s investigation, in the present research medical therapy was withheld 72 h prior to examination. This was done to assess the present disease activity (CSF-pressure) and, therefore, the therapeutic improvement of OCT parameters may have been underestimated.
The response time for the optic disc to normalize after treatment may depend on the severity of baseline disc edema and the type and dosage of medical therapy itself. The most commonly recommended medical therapy is acetazolamide but current dosage practices are based on clinical experience. Randomized prospective trials assessing the dose–response relation are lacking. In this study, a median and fairly high dose of 1.5 g/day acetazolamide tended to normalize OCT within 2–3 months and lead to symptomatic relief in 94% (16/17) patients. Although rare, rapid, progressive IIH exists and requires aggressive intervention to prevent loss of vision [17].
During follow-up, improvement in OCT was accompanied by corresponding visual field mean deviation improvements. A similar finding was noted by Rebolleda et al. [11] in their 1-year follow-up study. Salgarello et al. [18] also demonstrated a close association between confocal scanning laser ophthalmoscopy of optic disc tomography and visual field sensitivity in IIH at baseline and at 17.1 ± 9 months of follow-up. Our results further indicate that resolution occurs early, within the first months after initiation of treatment.
Although a relation between the severity of papilledema and visual field loss was demonstrated in the present study, OCT and automated perimetry represent different, but complimentary physiologic and anatomic information and should be used in combination.
The main problem in using OCT to follow-up IIH is that OCT cannot distinguish emerging axonal atrophy from resolving edema. OCT relates to the thickness of retinal layers and not to the quantitative amount of nerve fibers or water related to edema. Moreover, severe papilledema with markedly increased RNFLT presents a technical challenge for the OCT technique. In severely thickened retinal tissue, absorption and scatter of the emitted light beam increase relative to the back-reflected light. This may lead to a decreased signal-to-noise ratio and thus impair the ability to obtain OCT images. In our study, we were unable to measure RNFLT and RT in 4 and 3 patients, respectively, during presentation. Such difficulties were not described in previous OCT studies focusing on mild edemas [11, 19, 20].
By contrast, visual field testing is an instrument to monitor visual losses in IIH which may be sensitive to previous perimetric experience [21–23]. The initial functional improvement found in our study during follow-up evaluation may, in part, reflect a learning effect.
In this study, we re-evaluated disease activity by means of CSF-pressure 3 months after diagnosis. A marked reduction in CSF-pressure was noted in more than 50% of patients, although they did not differ from the others with respect to OCT and visual field parameters. An intriguing new hypothesis is that severity of papilledema at presentation is not predictive for a chronic course of IIH. This area should be addressed in future studies.
Surprisingly, we found a clear difference in the extent of weight-loss between the group with markedly decreased pressure and the group with a persistent high pressure. The former group was characterized by a >3.5% reduction in BMI during follow-up. This led to a second hypothesis that weight reduction is the most important predictor of a short term outcome of IIH.
The strong association between IIH and obesity is well known [24]. Evidence from clinical studies indicates that papilledema is more rapidly reversed or more easily controlled if weight-loss is achieved [4–10]. However, previous studies evaluated weight-loss in relation to resolution of papilledema, not in relation to CSF-pressure.
There is, to our knowledge, only one previous study describing the change in CSF-pressure after weight reduction. A decrease in CSF-pressure from 35.3 ± 35 to 16.8 ± 12 cmH2O was reported in 8 patients following a weight-loss of 57 ± 5 kg, but their follow-up period ranged from 4–72 months and their clinical and therapeutic status were not reported [4]. Future controlled weight-reduction studies in IIH using pre-defined weight-loss cut-off limits are needed to corroborate our hypothesis.
Compared to prior studies, our patient sample is noteworthy for the lower level of obesity than in other investigations [5, 10]. This suggests that less obese IIH patients also benefit from weight-loss, and our finding that a better outcome is associated with BMI-reduction >3.5% from baseline may be helpful for clinicians.
A limitation of the present study is the small sample size. Although the incidence is increasing, IIH is a relatively rare clinical entity. In order to prevent loss of vision it is essential to recognize the symptoms and identify these patients in the early stages. Our follow-up time was relatively short but it was demonstrated that the disease activity within the very first weeks is essential. Longer follow-up periods to assess visual outcome, dynamic CSF-pressure and long-term benefits of weight-loss can, nevertheless, be recommended.
In conclusion, OCT in combination with visual field testing is a valuable objective tool to monitor IIH patients during the initial disease course. Disease activity described by CSF opening pressure at 3-month follow-up was evaluated for the first time, raising new hypotheses about outcome. Although medical therapy is important to improve visual morbidity, weight-loss may be the main factor related to a shortened disease course and is strongly recommended for all over-weight IIH-patients.
References
Headache Classification Subcommittee of the International Headache Society (2004) The international classification of headache disorders, 2nd edn. Cephalalgia 24(Suppl 1): 9–160
Friedman DI, Jacobson DM (2002) Diagnostic criteria for idiopathic intracranial hypertension. Neurology 59:1492–1495
Skau M, Brennum J, Gjerris F, Jensen R (2006) What is new about idiopathic intracranial hypertension? An updated review of mechanism and treatment. Cephalalgia 26:384–399
Sugerman HJ, Felton WL, Salvant JB, Sismanis A, Kellum JM (1995) Effects of surgically induced weight loss on idiopathic intracranial hypertension in morbid obesity. Neurology 45:1655–1659
Sugerman HJ, Felton WL, Sismanis A, Kellum JM, DeMaria EJ, Sugerman EL (1999) Gastric surgery for pseudotumor cerebri associated with severe obesity. Ann Surg 229:634–640
Kupersmith MJ, Gamell L, Turbin R, Peck V, Spiegel P, Wall M (1998) Effects of weight loss on the course of idiopathic intracranial hypertension in women. Neurology 50:1094–1098
Wong R, Madill SA, Pandey P, Riordan-Eva P (2007) Idiopathic intracranial hypertension: the association between weight-loss and the requirement for systemic treatment. BMC Ophthalmol 7:15–20
Johnson LN, Krohel GB, Madsen RW, March GA (1998) The role of weight loss and acetazolamide in the treatment of idiopathic intracranial hypertension. Ophthalmology 105:2313–2317
Rowe FJ, Sarkies NJ (1999) The relationship between obesity and idiopathic intracranial hypertension. Int J Obes Relat Metab Disord 23:54–59
Michaelides EM, Sismanis A, Sugerman HJ, Felton WL (2000) Pulsatile tinnitus in patients with morbid obesity: the effectiveness of weight reduction surgery. Am J Otol 21:682–685
Rebolleda G, Munoz-Negrete FJ (2009) Follow-up of mild papilledema in idiopathic intracranial hypertension with optical coherence tomography. Invest Ophthalmol Vis Sci 50:5197–5200
Schuman JS, Hee MR, Puliafiro CA et al (1995) Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol 113:586–596
Pons ME, Garcia-Valenzuela E (2005) Redefining the limit of the outer retina in optical coherence tomography scans. Ophthalmology 112:1079–1085
Frisén L (1982) Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry 45:13–18
Parikh RS, Parikh SR, Sekhar GC, Prabakaran S, Babu JG, Thomas R et al (2007) Normal age-related decay of retinal nerve fiber layer thickness. Ophthalmology 114:921–926
Budenz DL, Anderson DR, Varma R et al (2007) Determinants of normal retinal nerve fiber layer thickness measured by stratus OCT. Ophthalmology 114:1046–1052
Thambisetty M, Lavin PJ, Newman NJ, Biousse V (2007) Fulminant idiopathic intracranial hypertension. Neurology 68:229–232
Salgarello T, Falsini B, Tedesco S, Galan ME, Colotto A, Scullica L (2001) Correlation of optic nerve head tomography with visual field sensitivity in papilledema. Invest Ophthalmol Vis Sci 42:1487–1494
Karam EZ, Hedges TR (2005) Optical coherence tomography of the retinal nerve fiber layer in mild papilloedema and pseudopapilloedema. Br J Ophthalmol 89:294–298
El-Dairi MA, Holgado S, O’Donnell T, Buckley EG, Asrani S, Freedman SF (2007) Optical coherence tomography as a tool for monitoring pediatric pseudotumor cerebri. J AAPOS 11:564–570
Wall M, George D (1991) Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain 114:155–180
Rowe FJ, Sarkies NJ (1998) Assessment of visual function in idiopathic intracranial hypertension: a prospective study. Eye 12:111–118
Capris P, Autuori S, Capris E, Papadia M (2008) Evaluation of threshold estimation and learning effect of two perimetric strategies, SITA Fast and CLIP, in damaged visual fields. Eur J Ophthalmol 18:182–190
Durcan FJ, Corbett JJ, Wall M (1988) The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol 45:875–877
Acknowledgments
This study was sponsored by Research Foundation of Capital Region, VELUX foundation and the John and Birthe Meyer Foundation. The authors report no disclosures or conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skau, M., Sander, B., Milea, D. et al. Disease activity in idiopathic intracranial hypertension: a 3-month follow-up study. J Neurol 258, 277–283 (2011). https://doi.org/10.1007/s00415-010-5750-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-010-5750-x