Abstract
Saccades and hand-tapping are both potential biomarkers in patients with Huntington’s disease (HD). While it is well known that patients with manifest Huntington’s disease display abnormalities in both of these tasks, less is known about how these abnormalities progress over time, or to what extent premanifest patients are affected. This study was designed to address these issues. We examined premanifest and manifest Huntington’s cohorts, together with a group of controls, over a 3-year period. Data were collected using a portable head-mounted saccadometer and a computerised hand-tapping device. Both premanifest and manifest Huntington’s disease patients display significant and systematic changes from year to year in the parameters describing saccadic latency, while controls remain unchanged. By contrast, although hand-tapping was abnormal in HD patients, annual changes were much smaller. Measuring the rate of progression of saccadic abnormalities in manifest HD patients may provide a way to track disease progression, and thus help to evaluate novel therapies to modify the disease. The clear-cut progression in saccadic abnormalities in the premanifest group may prove useful in the future as a predictor of time to disease onset.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although abnormal CAG expansion in exon1 of the Huntingtin (htt) gene predicts the eventual manifestation of Huntington’s disease (HD), it does not provide a reliable guide to the age at which overt disease will develop or how quickly it will progress. Gross motor abnormalities, such as chorea, are currently used to diagnose manifest disease; however, they may be preceded by more subtle motor changes, so that sufficiently sensitive tests may bring forward the time of detection of the earliest motor manifestations. Previous studies, examining longitudinal changes in the motor function of individuals progressing from premanifest to manifest, have demonstrated a significant decline in rapid alternating movements of the extremities, in stretch reflexes and ocular movements, particularly optokinetic nystagmus [17] and saccadic velocity. Small differences have also been described in response times, whether for spontaneous movements such as alternate button tapping, or in simple or choice reaction times to external stimuli [15, 16]. Both simple as well as complex (simultaneous and sequential) movements of the arm and hand reveal explicit deficits of timing at different stages of the disease. Simple timed motor tests such as finger dexterity, movement between two points, and walking tests, all demonstrate deterioration over time in manifest HD [9, 30, 35]. Hand-tapping parameters differ between HD and control populations and show high reproducibly and correlate with motor Unified Huntington's disease rating scale (UHDRS) changes over time in manifest cases of the disease [28]. However, how hand-tapping rate changes over time in premanifest patients [3, 34] is currently unknown, as is whether it can be used to define the transition to manifest disease, as Saft, et al. [30] have suggested.
Huntington’s disease patients demonstrate a range of oculomotor abnormalities, including impairment of saccades and pursuit [26, 37]. Saccades are typically slow and hypometric, and the more ‘voluntary’ types of saccade, such as anti-saccades and memory guided saccades, are particularly affected [5, 6, 24, 25]. Saccadic reaction times or latency may be affected, though previously we have shown that it is more useful to look not just at mean latencies, but at their distributions, abnormalities of which can provide important quantitative neurological information that can be related to our knowledge of the underlying neural mechanisms. This approach can distinguish premanifest individuals from controls by virtue of the former having an increased number of early saccades (responses with unusually short latencies) [2]. Such findings are consistent with other oculomotor studies that have demonstrated the utility of saccadic latency measurement in detecting early changes in HD [1, 3, 10, 11, 33].
In the present study, we have used two simple motor tasks—saccadometry and repetitive hand-tapping—to examine a large cross-sectional cohort of patients, and to study the longitudinal change in two groups, one of premanifest (PMG) individuals and one of manifest (MG), over a 3-year period. Both tasks are quick and easy to perform using a non-invasive portable device, and yield data that can be fully characterised with a small (two or three) number of parameters, based on the linear approach to threshold with ergodic rate (LATER) model of decision making (for more detail on the mathematical background and experimental justification see [7], and for further references see http://www.cudos.ac.uk/later.html). Our aim was to see whether this approach could yield quantitative measures of the decline of performance over time in MG as well as PMG patients. If successful, such techniques could be routinely employed to provide not only a better prediction of disease onset, but also to serve as a more objective and quantitative measure by which to assess the effects of new therapies.
Materials and methods
Participants
The present study was approved by the local Regional Ethics Committee and was conducted at the Cambridge Centre for Brain Repair, UK. Participants were recruited from the regional HD clinic at the Centre. All patients had a positive genetic test for HD and were evaluated by an experienced neurologist (RAB) using a standard neurological examination and the UHDRS to ascertain, with at least 99% certainty, whether individuals had motor manifestations of Huntington’s disease. On this basis, participants were divided into three groups: manifest (MG), with overt motor signs, premanifest (PMG), with no diagnostic motor signs, and controls (C), who were usually the partners/spouses of the patients and had no known neurological disorder. All participants gave their informed consent after the procedures had been explained to them.
Two populations of patients were examined. The first set (Table 1), studied longitudinally over 3 years, consisted of 36 HD gene carriers, divided into a group of 18 PMG patients and another of 18 MG patients, along with 12 controls. Because PMG individuals progress to MG with time, it follows that the average age of PMG patients is expected to be less than that of MG patients, and this is indeed found in our groups. The mean age of the controls lies midway between that of the PMG and MG patients. The PMG patients were mostly not on any medication, with only a few individuals (three out of 18) taking antidepressants (fluoxetine or citalopram). In contrast, most of the MG patients were on various treatments including olanzapine, carbamazepine and citalopram (Table 2). No controls were taking any medication at the time of testing.
The second set of patients, studied cross-sectionally, consisted of a group of 29 individuals who were premanifest at the time of the study, along with 62 manifest patients (Table 3).
Recording eye movements
Participants sat 1.5 m from a matt screen, with dim ambient lighting. Visually guided horizontal eye movements were recorded using a miniaturised infra-red 1 kHz saccadometer, low-pass filtered at 250 Hz with 12 bit resolution (Ober Consulting, Poznan, Poland, [29]). It is mounted on the patient's head by an elastic strap and rests comfortably on the nose; three built-in low-power lasers project red 13 cd m−2 spots subtending some 0.1° in a horizontal line in the midline at ±10° [1, 2]. Because the stimuli move exactly with the head, no head-restraint is necessary; sessions are, therefore, comfortable for the participants, including for the HD patients presenting with chorea, and a great deal of data can be gathered without fatigue.
Each trial began with the central fixation target displayed for a random fore-period of 0.5–1.5 s. On its extinction, one of the two peripheral targets appeared, chosen at random, remaining illuminated until 25 ms after the end of the resultant saccade, or for 1 s, whichever was shorter; participants were instructed to follow the target with their eyes as it moved. Twenty calibration trials were followed by 300 experimental trials, taking some 10–15 min; aberrant records contaminated by blinks, excessive head movement or other abnormalities were automatically removed by the software, which was also used to determine saccadic latency using an algorithm based on velocity and acceleration. The resultant latency distributions were then analysed using specialized software SPIC [8], calculating best-fit LATER (http://www.cudos.ac.uk/later.html) parameters (μ, σ and σ E) for each distribution (Fig. 2) by minimisation of the Kolmogorov–Smirnov one-sample statistic [19].
Recording hand-tapping
Participants sat in front of the hand-tapping device, which is a box with two push-buttons projecting from the top 30 cm apart, one red and one green [28]. They were instructed to tap the buttons alternately as fast as possible over a 45 s period, as timed by software on a laptop connected to the device. Both hands were tested separately, the dominant hand first. The successive intervals between taps were recorded for each hand separately in order to generate histograms of the distribution of intervals between consecutive taps. The statistics of these inter-tap intervals for hand-tapping were then analysed in the same way as for saccades, using SPIC, calculating best-fit LATER parameters (μ, σ). Data were analysed using appropriate statistical techniques, specified in the relevant parts of the results section; where required, it was first determined that distributions did not depart from normality (Shapiro–Wilk, p > 0.05).
Saccadic and hand-tapping assessments were undertaken at the same time as the clinical assessments, so that we collected all the data in a single test session for each participant.
Results
Typical distribution plots
Figure 1 shows the distributions of manual and saccadic latencies for a typical gene-positive manifest HD patient. Distributions of reaction times, whether manual or saccadic, are usually skewed, with a long tail to longer latencies. However, in general, the reciprocal of reaction time, or promptness, follows a Gaussian distribution (and is, therefore, more amenable to statistical analysis). Consequently, if latency distributions are plotted cumulatively on a probit scale, using a reciprocal abscissa (a reciprobit plot), they will be expected to generate a straight line, as seen in Fig. 1a for the manual responses. Such a distribution can be fully described by just two parameters; these are μ, the reciprocal of the median latency, and σ, its standard deviation. A large value of μ corresponds to increased promptness or speed of response, and thus a shorter latency; because of the reciprocal relationship, the units for these two parameters are s−1, or Hz. A further advantage is that μ is proportional to a commonly used clinical measure of performance in repetitive self-paced tasks such as hand-tapping; namely, the number of movements made in a given period of time.
Reciprobit plots of cumulative distributions of reaction time in a single manifest HD patient. a Manual responses for the left and right hands (red and blue data points, respectively, and both combined (green). The cumulative distribution is a straight line, indicating that the reciprocal of reaction time follows a Gaussian distribution. b Saccades responses. The reaction times are faster, with a larger standard deviation, and there is an additional sub-population of early saccades, lying on a line with shallower slope. In both figures the lines represent asymptotes of best fit (minimisation of Kolmogorov–Smirnov statistic) for the two parameters of the main distribution, μ and σ, and for σ E, which describes the population of early saccades
For saccades (Fig. 1b), there is often additionally a small sub-population of early saccades, that typically lie on a different straight line with a shallower slope, intersecting the infinite time axis on the right at p = 0.5. In this case, a third parameter σ E, the standard deviation of this early population, is also estimated. These are the parameters analysed in this study, except in the case of hand-tapping, for which no early responses are found in practice, so that σ E does not exist.
Longitudinal population
As expected, the mean age of MG patients (55.2 years) was significantly higher than that of PMG patients (45.5 years, p < 0.05). The groups were otherwise well matched with no significant difference in their sex balance or mean CAG repeat length. The control group had a mean age which fell halfway between the PMG and MG groups (50.1 years) with a similar sex balance. These data are summarized in Table 1.
Saccadic reaction times
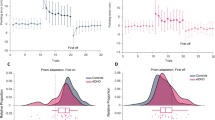
Figure 2 shows the measured values of the saccadic distribution parameters for horizontal visually evoked saccades in each of the 3 years for the two patient groups (PMG and MG) and the controls. For both PMG and MG groups, the values of μ and σ E can be seen to decrease with time, while σ appears not to vary, and this is confirmed by paired t tests comparing year 3 and year 1 (17 d.f.: μ, p = 0.033; σ, p = 0.337; σ E, p = 0.0005). The controls showed no significant change in any of the parameters over the 3 years of the study (p > 0.05 in all cases). Comparing the PMG to MG groups for all 3 years together, it is apparent that μ is greater for the PMG group than for the MG group, and this is confirmed by an unpaired t test (53 d.f., p = 0.046); no significant difference (p > 0.05) was found for either σ or σ E.
Summary of results, combining left and right responses, for horizontal saccades in premanifest and manifest patient groups as well as on a matched control population. For each of the distributional parameters, μ, σ and σ E, the progressive values are shown for years 1, 2 and 3. Error bars represent one SE. μ, σ = mean and standard deviation of reciprocal latency (or promptness) for the main population; σ E = standard deviation of the early population. For both the PMG and MG patients, promptness is reduced (and therefore latency increased) over years 1–3. Early saccades (σ E) follow a similar pattern: both premanifest and manifest individuals steadily decline from year 1 to year 3, but in this case there is an increase between PMG and MG patients, which may relate in part to medication. The controls show no significant change in any of these parameters over the 3 years of the study
Hand-tapping
Corresponding results for hand-tapping are shown in Fig. 3a, b. In contrast to the saccadic parameters, there are no significant changes in μ or σ within either group over time (p > 0.05). When comparing the groups for all 3 years together, μ is again significantly greater for the PMG group than the MG group for all 3 years (Fig. 3a; unpaired t test, p < 0.001), but there is no significant difference in σ (p > 0.05). The controls showed no significant change over time in either μ or σ (p > 0.05).
a Summary of results for intervals between responses in hand-tapping. For both the distributional parameters, μ and σ, the progressive values for the two groups (premanifest and manifest) are shown for years 1, 2 and 3 (the units are s−1 or Hz). Error bars represent one SE. The only significant difference observed with the repetitive hand-tapping task between MG and PMG groups is in μ, with the MG group being significantly slower. No significant change in any of these measures in the control population was seen during the same 3-year period. b Rate of right hand taps (measured over 45 s) for both premanifest and manifest groups compared to the total UHDRS motor score. For the PMG (red) group, the correlation of the absolute number of taps with UHDRS is not significant as one would anticipate, (R2 = 0.014 and p = 0.66). For the MG (blue) group, the correlation of the absolute number of taps with this clinical assessment is statistically significant (R2 = 0.42 and p = 0.0069)
We also correlated the hand-tapping rate with UHDRS motor scores, as was done previously in a manifest group of patients [28]. Again, we showed that the right hand-tapping rate correlated significantly and negatively with total UHDRS motor score, but only for MG patients (R 2 = 0.42 and p = 0.0069). For the PMG group there was, as one might expect, no significant correlation (R 2 = 0.014 and p = 0.66).
Cross-sectional population
Comparison of saccades and hand-tapping
Figure 4 shows the correlation of the measured values of μ for hand-tapping and for saccades for the cross-sectional set of patients. Premanifest (n = 29) form a group visually distinct from manifest (n = 62), the former lying above and to the right, reflecting the increased values of μ for both hand-tapping and saccades that were noted in Figs. 2 and 3. Linear regression for the two groups individually shows a rather weak correlation between manual and saccadic values (PMG: R 2 = 0.163, p = 0.41; MG: R 2 = 0.32, p = 0.013), but considering both groups together, the correlation is much stronger and statistically significant (R 2 = 0.44, p < 0.0001).
Cross-sectional correlation between measured values of μ (mean promptness, or reciprocal median latency) for hand-tapping and for saccades; each point represents an individual patient (blue, premanifest; red, manifest). The premanifest individuals (blue) form a cluster that is distinct from that for the manifest (red). Considering both groups together, there is a strong statistically significant correlation (R 2 = 0.44, p < 0.0001)
Correlation with expected number of years to disease onset in PMG
We have used the IOWA HD calculator as described by Langbehn et al. [20] to see whether the saccadic median latency correlates with the expected number of years to disease onset. We found no correlation in any of our motor measures in any study year to estimate time to disease onset in our PMG patients.
Discussion
In this study, we have measured the longitudinal change in premanifest and manifest HD individuals over a 3-year period using two different techniques: saccadometry and hand-tapping. One primary aim was to detect changes over time and investigate whether the two techniques—one measuring responses evoked by an external stimulus, the other measuring internally evoked responses—were affected in similar ways by disease. We have shown that there are significant differences in the distributional parameters between the two groups: in the manifest group, median latency is increased for both kinds of response, and the incidence of early saccades is increased, but the slope (σ) varies very little. With the passage of time, there are marked changes in the saccadic parameters, such that clear progression can be seen over 12-month periods in both PMG and MG patients. In particular, saccadic median latency is higher (and promptness, therefore, lower) in the MG patients than the PMG patients, and in both groups increases steadily over time; however, the slope (σ) is constant over this same period. In addition, the incidence of early saccades, like saccadic promptness, declines over time within both groups, but with a marked increase between the PMG and MG groups.
Stage of disease
It is clear that distributions of saccadic latency can distinguish PMG from MG patients [2], as well as show steady monotonic changes over time. The current results are consistent with previously published data [1, 4, 6, 10, 32, 38] showing the utility of saccadic measurements in detecting the earliest changes in Huntington’s disease, including—as we have shown previously—in premanifest patients [2]. In addition, we have confirmed our earlier findings of the utility of studying hand-tapping in HD, which used a non-computerised version of the hand-tapping device [28]. These measurements also very clearly distinguish PMG from MG patients, even if they do not seem to show significant changes over the 3 years.
Tracking disease progression
One striking aspect of the changes in the distribution parameters in this study is the steady increase in saccadic median latency over time for both MG and PMG groups, equivalent to about 24 ms from year 1 to 3. Reaction times tend to increase with age in the normal population, but only by around 1 ms per annum [18]; in the control group for this cohort there was no significant change. The incidence of early saccades (σ E) shows a steady decline over time in both groups, but with a marked increase between the PMG and MG groups. The increase in the number of early, unregulated, spontaneous saccades (σ E) in the transition from PMG to MG could be regarded as being analogous to the increase in spontaneous, unwanted movements of chorea that currently define the onset of manifest disease in HD. But the gradual decrease in σ E in both PMG and MG groups is not what one would expect if indeed it is related to chorea, and this trend is difficult to account for.
Caution is needed in comparing premanifest and manifest patients, and interpreting changes over time in the manifest group, because of the confounding effect of medication. Currently, we do not have sufficient data to be able to say how much of the changes described above—including, for instance, the correlation seen in Fig. 4—are due to the disease progression and how much to pharmacology. The only relevant data in this study are from the 18 MG patients, of whom four have had no medication over the 3-year period. Their mean saccadic latency appeared not to change significantly over this period (paired t tests, 3 d.f.: μ, p = 0.069; σ, p = 0.481; σ E, p = 0.086). The apparent sudden change in the value of hand-tapping, μ, in the absence of any discernible change over time in the premanifest group, also suggests that some of the observed changes could be influenced by medication. As this longitudinal study continues, premanifest patients will become manifest, and we will then be able to resolve this fundamental question.
Predicting disease onset
The best-known algorithm that has been proposed as a predictor of disease onset is the HD calculator, as described by Langbehn et al. [20], which takes into account the age of a premanifest individual together with their CAG repeat length. If the mean saccadic latency were a predictor of disease onset, one might expect it to correlate with the output of the HD calculator. In fact, in our group there was no significant correlation. This may be due to the fact that our premanifest group was too far from disease onset (using μ for year 1, the expected number of years to disease onset was 13.07 ± 5.5; mean ± SD), and this formula is generally applied to those individuals likely to develop disease in the next 10 years. The incremental increase in mean saccadic latency in the premanifest group as a whole suggests strongly that regular measurements on an annual basis may be a reliable method for estimating the onset of manifest HD, and perhaps more useful than some of the range of different approaches that have been adopted to define the earliest abnormalities of HD, in particular, measures of cognitive ability. Cognitive dysfunction in attention, concentration, visuospatial abilities and memory are present in the early stages of the disease and progress over time. Previous studies [13, 15, 16, 31, 36] that have examined the cognitive changes in premanifest and early stage HD individuals suggest that there may be early changes, but have failed to identify criteria that could provide a clear cut point of transition, in part because such tests are intrinsically subjective and qualitative in nature. Quantitative tools, such as the ones we present here, appear to offer a relatively sensitive and precise means of detecting abnormalities that progress over time in premanifest patients, which can be deployed robustly in small cohorts of patients.
Comparison of saccadometry and hand-tapping
Within both the premanifest and manifest groups, median latency and the standard deviation for hand-tapping remained stable over the 3 years. However, there was a clear difference in median latency between the two groups; the manifest group having a much longer latency (and therefore lower promptness) than the premanifest group.
The two kinds of test, looking at different aspects of motor control, are likely to be affected in different ways, at different times by the disease process. As shown in Fig. 4, when a linear regression for the two groups was applied to each individual data set, there was only a rather weak correlation, but when we considered the two groups together, the correlation was much stronger and statistically significant.
A further examination of the data from the PMG and MG patients reveals other interesting similarities and differences. Baseline values of median latency for saccades and hand-tapping are correlated in both PMG and MG patients, yet changes in latency over time do not correlate in this way. This suggests that the two types of response are differentially affected by progression of the disease process.
Comparison of externally and internally triggered movement
The saccadic system is widely distributed in the brain, and is therefore affected by a broad range of neurological conditions [25, 27]. That oculomotor impairments are one of the first characteristics of HD to emerge [15–17, 21–23, 26, 37] is most probably due to the close involvement of the cortex and basal ganglia with the saccadic control circuit [12, 14], and, as such, provides an excellent research tool [25]. In addition, the basal ganglia and their cortical projections control internally generated movements such as hand-tapping. In this study we, therefore, used two tasks which differ not simply in what is being moved (hand or eye), but also, and perhaps more profoundly, in how the movement is evoked; purely internally in the case of hand-tapping, in the sense that each movement is triggered by the previous one, and purely externally in the case of saccades.
The two kinds of test, looking at different aspects of motor control, are likely to be affected in different ways at different times by disease process. Comparing PMG and MG patients, both similarities and differences emerge in the results of the two tests. Baseline values of median latency for saccades and hand-tapping are correlated in both PMG and MG patients, yet changes in latency over time do not correlate in this way. This suggests that the two types of response are differentially affected by progression of the disease process.
Overall, this study has shown, for the first time, that significant changes over time can be found in both premanifest and manifest individuals, but not controls, over a 3-year period. The simplicity and robust nature of the assessments, coupled to their ability to detect significant changes annually, make them attractive markers of disease progression and potential predictors of disease onset.
References
Ali FR, Michell AW, Barker RA, Carpenter RH (2006) The use of quantitative oculometry in the assessment of Huntington’s disease. Exp Brain Res Exp Hirnforsch 169:237–245
Antoniades CA, Altham PM, Mason SL, Barker RA, Carpenter R (2007) Saccadometry: a new tool for evaluating presymptomatic Huntington patients. Neuroreport 18:1133–1136
Biglan KM, Ross CA, Langbehn DR, Aylward EH, Stout JC, Queller S, Carlozzi NE, Duff K, Beglinger LJ, Paulsen JS (2009) Motor abnormalities in premanifest persons with Huntington’s disease: the PREDICT-HD study. Mov Disord 24:1763–1772
Blekher TJS, Marshall J, White K, Hui S, Weaver M, Gray J, Yee R, Stout JC, Beristain X, Wojcieszek J, Foroud T (2006) Saccades in presymptomatic and early stages of Huntington disease. Neurology 67:394–399
Blekher T, Weaver MR, Cai X, Hui S, Marshall J, Jackson JG, Wojcieszek J, Yee RD, Foroud TM (2009) Test-retest reliability of saccadic measures in subjects at risk for Huntington disease. Invest Ophthalmol Vis Sci 50:5707–5711
Blekher TMYR, Kirkwood SC, Hake AM, Stout JC, Weaver MR, Foroud TM (2004) oculomotor control in asymptomatic and recently diagnosed individuals with the genetic marker for Huntington’s disease. In: Vision research, pp 2729–2736
Carpenter RH, Williams ML (1995) Neural computation of log likelihood in control of saccadic eye movements. Nature 377:59–62
Carpenter RHS (1994) SPIC: a PC-based system for rapid measurement of saccadic responses. J Physiol 4P:480
Garcia Ruiz PJ, Hernandez J, Cantarero S, Bartolome M, Sanchez Bernardos V, Garcia de Yebenez J (2002) Bradykinesia in Huntington’s disease. A prospective, follow-up study. J Neurol 249:437–440
Golding CVP, Danchaivijitr C, Hodgson TL, Tabrizi SJ, Kennard C (2006) Identification of an oculomotor biomarker of preclinical Huntington disease. Neurology 67:485–487
Hicks SL, Robert MP, Golding CV, Tabrizi SJ, Kennard C (2008) Oculomotor deficits indicate the progression of Huntington’s disease. Prog Brain Res 171:555–558
Hikosaka O, Takikawa Y, Kawagoe R (2000) Role of the basal ganglia in the control of purposive saccadic eye movements. Physiol Rev 80:953–978
Ho AK, Sahakian BJ, Brown RG, Barker RA, Hodges JR, Ane MN, Snowden J, Thompson J, Esmonde T, Gentry R, Moore JW, Bodner T (2003) Profile of cognitive progression in early Huntington’s disease. Neurology 61:1702–1706
Isoda M, Hikosaka O (2008) Role for subthalamic nucleus neurons in switching from automatic to controlled eye movement. J Neurosci 28:7209–7218
Kirkwood SC, Siemers E, Bond C, Conneally PM, Christian JC, Foroud T (2000) Confirmation of subtle motor changes among presymptomatic carriers of the Huntington disease gene. Arch Neurol 57:1040–1044
Kirkwood SC, Siemers E, Hodes ME, Conneally PM, Christian JC, Foroud T (2000) Subtle changes among presymptomatic carriers of the Huntington’s disease gene. J Neurol Neurosurg Psychiatry 69:773–779
Kirkwood SC, Siemers E, Stout JC, Hodes ME, Conneally PM, Christian JC, Foroud T (1999) Longitudinal cognitive and motor changes among presymptomatic Huntington disease gene carriers. Arch Neurol 56:563–568
Klein C, Foerster F, Hartnegg K, Fischer B (2005) Lifespan development of pro- and anti-saccades: multiple regression models for point estimates. Brain Res Dev Brain Res 160:113–123
Kolmogorov A (1941) Confidence limits for an unknown distribution function. Ann Math Stat 23:525–540
Langbehn DR, Brinkman RR, Falush D, Paulsen JS, Hayden MR (2004) A new model for prediction of the age of onset and penetrance for Huntington’s disease based on CAG length. Clin Genet 65:267–277
Lasker AG, Zee DS (1997) Ocular motor abnormalities in Huntington’s disease. Vis Res 37:3639–3645
Lasker AG, Zee DS, Hain TC, Folstein SE, Singer HS (1987) Saccades in Huntington’s disease: initiation defects and distractibility. Neurology 37:364–370
Lasker AG, Zee DS, Hain TC, Folstein SE, Singer HS (1988) Saccades in Huntington’s disease: slowing and dysmetria. Neurology 38:427–431
Lasker G, Adrian ZD (1997) Ocular motor abnormalities in Huntington’s disease. Vis Res 37:3639–3645
Leigh RJKC (2004) Using saccades as a research tool in the clinical neurosciences. Brain 127:460–477
Leigh RJ, Newman SA, Folstein SE, Lasker AG, Jensen BA (1983) Abnormal ocular motor control in Huntington’s disease. Neurology 33:1268–1275
Leigh RJZD (2006) The neurology of eye movements
Michell AW, Goodman AO, Silva AH, Lazic SE, Morton AJ, Barker RA (2008) Hand tapping: a simple, reproducible, objective marker of motor dysfunction in Huntington’s disease. J Neurol
Ober JK, Przedpelska-Ober E, Gryncewicz W, Dylak J, Carpenter RS, Ober JJ (2003) Hand-held system for ambulatory measurement of saccadic durations of neurological patients. In: Modelling and measurement in medicine
Paulsen JS, Langbehn DR, Stout JC, Aylward E, Ross CA, Nance M, Guttman M, Johnson S, McDonald M, Beglinger LJ, Duff K, Kayson E, Biglan K, Shoulson I, Oakes D, Hayden M (2007) Detection of Huntington’s disease decades before diagnosis: the predict HD study. J Neurol Neurosurg Psychiatry
Peinemann A, Schuller S, Pohl C, Jahn T, Weindl A, Kassubek J (2005) Executive dysfunction in early stages of Huntington’s disease is associated with striatal and insular atrophy: a neuropsychological and voxel-based morphometric study. J Neurol Sci 239:11–19
Peltsch A, Hoffman A, Armstrong I, Pari G, Munoz DP (2008) Saccadic impairments in Huntington’s disease. Exp Brain Res Exp Hirnforsch 186:457–469
Rupp J, Blekher T, Jackson J, Beristain X, Marshall J, Hui S, Wojcieszek J, Foroud T (2010) Progression in prediagnostic Huntington disease. J Neurol Neurosurg Psychiatry 81:379–384
Rupp J, Blekher T, Jackson J, Beristain X, Marshall J, Hui S, Wojcieszek J, Foroud T (2009) Progression in prediagnostic huntington disease. J Neurol Neurosurg Psychiatry
Saft C, Andrich J, Meisel NM, Przuntek H, Muller T (2006) Assessment of simple movements reflects impairment in Huntington’s disease. Mov Disord 21:1208–1212
Snowden JS, Craufurd D, Thompson J, Neary D (2002) Psychomotor, executive, and memory function in preclinical Huntington’s disease. J Clin Exp Neuropsychol 24:133–145
Starr A (1967) A disorder of rapid eye movements in Huntington’s chorea. Brain 90:545–564
Tsai Tzu-Tung LA, David Zee (1995) Visual attention in Huntington’s disease: the effect of cueing on saccade latencies and manual reaction times. Neuropsychologia 33:1617–1626
Acknowledgments
The authors thank all the patients who have participated in this study at the Cambridge Centre for Brain Repair. Many thanks to James FitzGerald for comments on the manuscript. This work has been supported by an award to C.A.A by the Medical Research Council of the United Kingdom and through the NIHR Biomedical Research Centre award to the Department of Clinical Neurosciences, Addenbrooke’s Hospital, Cambridge, United Kingdom.
Author information
Authors and Affiliations
Corresponding author
Additional information
R.H.S. Carpenter and Roger A. Barker are joint senior authors.
Rights and permissions
About this article
Cite this article
Antoniades, C.A., Xu, Z., Mason, S.L. et al. Huntington’s disease: changes in saccades and hand-tapping over 3 years. J Neurol 257, 1890–1898 (2010). https://doi.org/10.1007/s00415-010-5632-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-010-5632-2