Abstract
Cortical tubers are very common in tuberous sclerosis complex (TSC) and widely vary in size, appearance and location. The relationship between tuber features and clinical phenotype is unclear. The aim of the study is to propose a classification of tuber types along a spectrum of severity, using magnetic resonance imaging (MRI) characteristics in 35 patients with TSC and history of epilepsy, and to investigate the relationship between tuber types and genetics, as well as clinical manifestations. Three types of tubers were identified based on the MRI signal intensity of their subcortical white matter component. (1) Tubers Type A are isointense on volumetric T1 images and subtly hyperintense on T2 weighted and fluid-attenuated inversion recovery (FLAIR); (2) Type B are hypointense on volumetric T1 images and homogeneously hyperintense on T2 weighted and FLAIR; (3) Type C are hypointense on volumetric T1 images, hyperintense on T2 weighted, and heterogeneous on FLAIR characterized by a hypointense central region surrounded by a hyperintense rim. Based on the dominant tuber type present, three distinct patient groups were also identified: Patients with Type A tuber dominance have a milder phenotype. Patients with Type C tuber dominance have more MRI abnormalities such as subependymal giant cell tumors, and were more likely to have an autism spectrum disorder, a history of infantile spasms, and a higher frequency of epileptic seizures, compared to patients who have a dominance in Type B tubers, and especially to those with a Type A dominance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tuberous sclerosis complex (TSC) is a multisystem disorder with autosomal dominant inheritance which can affect the brain, heart, skin, kidneys, lungs, and retina [1]. Several cerebral abnormalities are associated with TSC including cortical tubers, subependymal nodules (SEN), subependymal giant cell tumors (SGCT) as well as white matter abnormalities such as radial bands and wedge-shaped lesions [2–4]. Cortical tubers have been reported in 82–100% of patients with TSC and vary widely in size and location [5]. Histological studies have shown that tubers are hypomyelinated hamartomas which are characterized by abnormal cortical lamination [6, 7] and the presence of giant or balloon cells, dysplastic neurons and astrogliosis [8–10]. Neurons in tubers are thought to be immature or developmentally arrested cell types [11]. On magnetic resonance imaging (MRI), tubers have traditionally been described as having increased signal of the cerebral cortex and decreased signal of the subcortical white matter on T1 weighted sequences, along with increased signal of cortex and subcortical white matter on T2 weighted sequences and fluid-attenuated inversion recovery (FLAIR) images [2, 12, 13].
Tubers are thought to be related to the neurological manifestations in TSC including seizures, cognitive deficits, and behavioral impairment [14–18]. α-[11C] methyl-l-tryptophan positron emission tomography (PET) studies suggested the presence of epileptogenic and nonepileptogenic tubers in TSC patients, with physiologic differences between these two types of lesions demonstrated by increased serotonin synthesis in epileptogenic tubers [19–21]. Diffusion weighted imaging (DWI) revealed a higher apparent diffusion coefficient (ADC) in cortical tubers compared to normal-appearing brain, as well as higher ADC values in epileptogenic tubers in comparison to nonepileptogenic tubers [22]. Recently, Major and colleagues [23] used intracranial electrocorticography to show that certain cortical tubers may be epileptically inactive, and that seizures may arise instead from the normal-appearing cortex surrounding the tuber.
Previous attempts have been made to identify different types of cortical tubers. In 1901, Pellizzi [24] proposed a dual classification based on pathological inspection of resected tubers: Type 1 having smooth surfaces, and Type 2 with a central depression of tissue associated with a cystic component. Nine decades later, Braffman et al. [8] were the first to describe these two types of cortical tubers on MR images. Recently, Chu-Shore and colleagues [25] showed a strong association between Type 2 cortical tubers, also called cyst-like tubers, and a TSC2 gene mutation, as well as a more aggressive seizure phenotype. The relationship between anatomical and physiological characteristics of tubers and their surrounding tissues and clinical phenotype remains unclear. Identification of different tuber types and a better understanding of their relationship with genotype and clinical manifestations, such as epileptic activity, and their severity may improve our comprehension of the pathophysiology of TSC. Our own experience with MRI has demonstrated three, rather than two, distinct types of tubers. The present study aims to better characterize this classification of three types of tubers seen in TSC, using the MRI signal characteristics of the subcortical white matter component in 35 patients with TSC and epilepsy. We also investigated the relationship between the dominant tuber type found in each patient, and other neuroanatomical characteristics, genetic and clinical manifestations, in order to assess an association between tuber type and disease severity. MRI and clinical records from a small group of patients without history of epilepsy were also reviewed and similar findings were obtained in regards to genetic mutation, dominant tuber type and MRI characteristics. Moreover, all these patients presented the three types of tubers. Since one of our main interests was to investigate epileptogenic features among the different tuber type dominance, only patients with a history of seizures were included in the present study.
Methods
Participants
MRI and clinical records of 35 patients were selected blindly among the population of patients seen at our TSC center and retrospectively reviewed for this study. The only selection criteria for inclusion were history of epilepsy and the availability of a volumetric T1 sequence, axial T2 weighted, axial FLAIR and axial diffusion tensor imaging (DTI). This study was approved by the MGH institutional review board and informed consent was waived since only retrospective data was analyzed. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
Magnetic resonance imaging
MR imaging was performed on a 1.5 T GE Signa system (GE Signa, Madison, WI) or on a 1.5 T Avanto or a 3 T TrioTim Siemens system (Siemens Medical Solutions, Erlangen, Germany) as part of the annual routine care of patients with TSC. Sequences obtained with 1.5 T systems included 3D SPGR (GE Signa) or MPRAGE (Avanto Siemens) (TR 32, TE 10, NEX 1, flip angle 25, matrix 256 × 192, 1.2 mm slice thickness, 0 mm gap) acquired in an axial plane, FSE (GE Signa) or TSE (Avanto Siemens) axial T2 (TR 6000, TE 102, NEX 2, ETL 12, Matrix 320 × 256, 3 mm slice thickness, 0 mm gap), axial FLAIR (TR 10000, TE 120, TI 2200, NEX 1, matrix 256 × 192, 3 mm slice thickness, 0 mm gap) and DTI (single shot, b value = 1,000 mm2/s, TR 10000, TE 91.6, NEX 1, Bandwidth 1953.12, FOV 220 × 220, matrix 100 × 100, slice thickness 2.2 mm with 0 mm gap). Sequences obtained with 3 T TrioTim Siemens system included MPRAGE (TR 2000, TE 3.7, NEX 1, flip angle 10, matrix 256 × 256, 1 mm slice thickness, 0 mm gap) acquired in an axial plane, TSE axial T2 (TR 5280, TE 87, NEX 1, ETL 9, matrix 256 × 256, 4 mm slice thickness, 0 mm gap), axial FLAIR (TR 9660, TE 73, TI 2700, NEX 1, matrix 256 × 179, 4 mm slice thickness, 0 mm gap) and DTI (single shot, b value = 1,000 mm2/s, TR 8000, TE 84, NEX 1, Bandwidth 1,445, FOV 2,048 × 2,048, matrix 128 × 128, slice thickness 2 mm with 0 mm gap). Diffusion tensor images were eddy current corrected and processed to create DWI and ADC maps.
The most recent MRI was retrospectively reviewed for each patient by a study investigator with experience in neuroimaging blinded to the clinical data after consultation with a pediatric neuroradiologist. For patients who underwent surgical resection because of intractable seizures, the most recent MRI prior to surgery was also reviewed. The brain was assessed for the presence of cortical and cerebellar tubers, associated white matter abnormalities, SEN and SGCT.
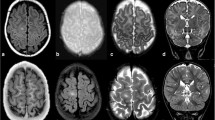
The signal intensity of cortical tubers and adjacent white matter abnormalities, as well as cerebellar tubers was assessed on each of the four MR sequences in comparison to adjacent normal parenchyma. Diagnostic criteria for cerebral and cerebellar lesion identification were in accordance with prior reports [12, 13, 26]. Tubers were defined as areas of cortical gray matter distortion with decreased or isointense subcortical signal intensity on T1 images, increased signal intensity on T2 FSE and increased or decreased signal on FLAIR sequences. Cortical and cerebellar tubers were identified and compiled. We identified three types of tubers: Type A with subcortical isointense signal on volumetric T1 images and subtly hyperintense signal on T2 weighted and FLAIR images, which exerted no mass effect on the surrounding brain and did not distort the gyral folding pattern (see Fig. 1); Type B tubers with subcortical hypointense signal on volumetric T1 images and homogeneously hyperintense signal on T2 weighted and FLAIR images, which had borders that were not well circumscribed, and that exerted little mass effect and minimally disrupted the gyral pattern (see Fig. 2); and Type C tubers with subcortical hypointense signal on volumetric T1, hyperintense signal on T2 weighted images and heterogeneous signal on FLAIR images, characterized by a hypointense central region surrounded by a hyperintense rim. Tuber Type C corresponds to cyst-like tubers previously described in the literature [8, 27]. This last type of tuber did exert a mass effect on the surrounding brain and distorted the gyral pattern (see Fig. 3). Each tuber was labeled as Type A, B or C. SEN were defined as nodular lesions attached to the ventricular margin extending into the ventricle. SGCT were defined as masses arising in the vicinity of the Foramen of Monro which demonstrate an increase in size over time with a measurement >1 cm. The presence of SEN and SGCT was determined using volumetric T1 and T2 weighted sequences.
ADC values of cerebral lesions were measured using circular regions of interest (ROI) with a minimum radius of 5 mm. Magnified conventional images were used to avoid regions of cerebrospinal fluid in the ADC measurements. ADC measurements were performed in Type B and Type C tubers determined on T2 weighted and FLAIR images. Because Type A tubers were not distinguishable on visual inspection of ADC maps, no ADC measures were made of these lesions. Up to 20 ADC values were measured in each tuber type (B and C, if present) distributed over the cerebrum in each patient. For each patient, the number of measurements depended on the number of tubers of each type which measured at least 5 mm to allow the minimum ROI size. Some patients had more than 20 tubers of Type B and/or Type C with adequate size. For these cases, the 20 tubers with the highest ADC values were selected for measurement. A mean ADC value was calculated for each tuber type (B and C), with no regard to the location, in all patients.
The number of cortical tuber types and the dominant cortical tuber type, which was determined on visual inspection as the type of tuber that was proportionally predominant to other tuber types in the brain, were determined for each individual. A qualitative assessment of the cerebral space occupied by tubers was made (1 = only a few tubers; 2 = multiple tubers that occupied a significant portion of the brain; 3 = at least half of the cerebral tissue was occupied by tubers).
Demographic and clinical information
Clinical charts of all 35 patients were reviewed for demographic information, TSC genotype (TSC1 or TSC2), intellectual quotient (IQ) or developmental quotient (DQ) obtained from the neuropsychological assessment performed closest in time to the reviewed MRI, clinical diagnosis of autism spectrum disorder (ASD), history of infantile spasms (IS), age at onset of epilepsy, frequency of seizures reported closest in time to the MRI (0 = seizure free, 1 = occasional, 2 = monthly, 3 = weekly, 4 = daily), control of seizures with two or fewer antiepileptic drugs (AED) for at least 12 months, number of all AEDs that had been used, as well as history and total number of treatments for epilepsy [AED, vagus nerve stimulator (VNS), ketogenic diet or low glycemic index diet, surgery].
Statistical analysis
All patients were divided into three groups corresponding to the dominant tuber type observed on MRI: group A, B or C corresponding to whether the dominant cortical tuber observed was Type A, B or C. Categorical variables were assessed by the Pearson chi-square test. For significant chi-square tests, one-to-one comparisons were made (group A vs. group B, group A vs. group C, group B vs. group C), using a Bonferroni correction for multiplicity of tests. Ordinal and continuous dependant variables were analyzed by Kruskal–Wallis one-way analysis of variance (ANOVA), with dominant tuber type groups as the inter-group factor. Post-hoc analysis was performed utilizing a Mann–Whitney test, using a Bonferroni correction. An ANOVA, with dominant cortical tuber type groups (group A, group B, and group C), and cortical tuber types visible on ADC maps (Type B and Type C) as factors, has been applied to ADC values. All reported P values used two-tailed tests of significance with α set at 0.05. Data points unknown due to unavailable test or histories were excluded from all statistical tests.
Results
MRI characteristics
MRI features are summarized in Table 1. No differences between cerebral and cerebellar tubers were found on visual MRI inspection. Thirty-one patients in our cohort (89%) demonstrated at least one Type A tuber (Fig. 1). Type B tubers were visible on MRI of all 35 patients included in this study (Fig. 2), and Type C tubers were seen in 29 patients (83%) (Fig. 3). Between six and 20 ADC values of Type B tubers have been measured in all patients. Mean ADC value of Type B was 1,168.97 ± 132.94 × 10−6 mm2/s. Between one and 20 ADC values of Type C tubers were measured in the 29 patients with type C tubers, with mean ADC value of 1,507.51 ± 170.65 × 10−6 mm2/s. In the literature, normal appearing parenchyma is reported to be between 700 and 900 × 10−6 mm2/s [22, 28]. There was a significant difference (F (1,28) = 223.04, P < 0.0001, ε = 0.998) between ADC values of cortical tubers Type B and Type C (see Fig. 4).
All patients enrolled in this study were found to have at least two tuber types; 10 of the 35 patients (29%) exhibited two types, and 25 individuals (71%) presented all three types. However, in each individual, one distinct tuber type appeared to be dominant. Figure 4 shows ADC data of tubers Type B and Type C for the three groups separately and for all 35 patients. This figure shows that group C had higher ADC values in Type B (P = 0.004) and Type C (P = 0.002) compared to the group A. Likewise, when we compared ADC values in cortical tubers between groups C and B, a trend was noted between both groups regarding tubers of Type B (P = 0.069) and a significant difference was obtained for Type C (P = 0.004).
Demographic data and clinical history
The patient demographic and clinical characteristics are given in Table 2. All 35 patients were between 1 and 21 years of age (mean 10 years 8 months, SD 4 years 9 months) at the time of the MRI. No age differences were found between groups. Significant differences between groups were noted with respect to TSC2 mutation, history of IS, and seizure frequency. Intragroup differences in ASD approached significance.
Discussion
Cortical tubers are very common in TSC and widely vary in size, appearance and location. The present study proposes identification of three types of tubers based on visual inspection of subcortical white matter tuber component MRI signal intensity. We found a relationship between the dominant tuber type and the severity of phenotype and cerebral abnormalities. Patients with a Type A tuber dominance had milder phenotype and brain abnormalities, whereas patients with Type C tuber dominance had more severe characteristics. Thus, the different tuber neuroimaging endophenotypes could be associated with genetic and clinical abnormalities that follow a spectrum of severity.
MRI features
Patients with Type C dominance were more likely to have more severe MRI abnormalities. First, 67% of patients with dominance in Type C had a SGCT, which can cause obstruction of cerebrospinal fluid flow, hydrocephalus, increased intracranial pressure, and even death [29]. This proportion of patients presenting SGCT was much higher than the proportion measured in both groups A (11%) and B (15%), and to the 6.1–18.5% previously reported in the general TSC population [8, 30]. Second, the proportion of the brain occupied by tubers also followed this spectrum of severity, increasing gradually from group A to group C. Here, we decided to use a qualitative measure of the tuber/brain proportion in contrast to the tuber count method. Although tuber count has been used as a marker of neurological severity in TSC [12, 31], more recent studies reported that tuber/brain proportion is a better predictor for cognitive impairment [16]. Furthermore, tuber count has been reported to undercount tubers as well as underestimate the impact of large cerebral lesions and overestimate the effect of small tubers. The qualitative aspect of the measure used in this study could be viewed as a methodological weakness, and a quantitative technique, such as tuber segmentation on brain MRI recently described by Jansen et al. [16], could be used in further studies.
ADC values measured in cerebral lesions seemed to also reflect the continuum of severity related to the three tuber types. Tubers Type A are not visually detectable on ADC maps. Type B tubers exhibited higher values than normal appearing parenchyma, and Type C tubers were associated with significantly higher ADC values than Type B tubers. An increase in diffusivity in association with higher T2 and decreased T1 signals indicates higher free water content that is likely due to an increase in extracellular space and a decrease in density of cellular elements. The T1 signal decrease may also be partly due to decreased myelination [28, 32, 33]. This is in close agreement with the histopathological findings in TSC, which has shown a disruption in normal cortical lamination, abnormal cell differentiation and reduction in density of myelinated fibers and number of normal neurons [22].
Interestingly, high ADC values in tubers have been associated with epileptogenicity of the lesion [22, 34]. Moreover, cyst-like tubers, which correspond to Type C in this study, have recently been associated with a more severe seizure phenotype than noncystic tubers [25]. This increase in epileptogenicity may be due to functional isolation of the tuber regions by the cystic white matter. In future studies, it would be interesting to directly investigate the association between tuber type and epileptogenicity using intracranial electrocorticography (see [23], for methodology) to see if Type C tubers are associated with heightened epileptogenicity than Type B and Type A. A better description and understanding of the association between tuber types and epileptogenicity could help develop an additional noninvasive tool for presurgical evaluation of patients who present with TSC with intractable epilepsy, by including measurement of ADC values of tubers in their work-up.
Sophisticated MRI techniques are now available and should help to discriminate tuber types in TSC patients. Compared to Braffman et al. [8] who identified only two types of tubers on 0.3–1.5 T MRI scans, we identified three tuber types using 1.5–3 T MRI scans. Among the three tuber types reported, Type A is associated with more subtle MRI signal abnormalities and can be easily missed, as we noticed in several clinical reports, by readers who do not have extensive experience with the neuroimaging characteristics of TSC. Clinically, it can lead to a misleading conclusion of a “negative” MRI.
Genetic and clinical characteristics
Genetic results showed that a gradual increase in the proportion of patients presenting TSC2 mutation in comparison to TSC1 was found between group A and group C. Although the literature reports an important overlap between neurologic and cognitive phenotype of mutations in both genes, TSC2 mutations have been associated with a more severe seizure phenotype, a lower cognitive function, the presence of more cerebral lesions and more severe dermatologic, kidney and pulmonary involvement in comparison to TSC1 mutation [35–38]. We also found a similar increase in severity among the three tuber groups in regards to some neurological characteristics. Indeed, the diagnosis of ASD was more frequent in group C than in the two other groups, and also more frequent in group B than in group A. A similar pattern was found for history of IS and seizure frequency.
Limitations
There are several methodological limitations with the current study. First and as reported above, a relatively small group of patients were investigated. This may be the reason for lack of statistical significance between the three groups regarding several variables, such as age at onset of epilepsy, or seizure control (see Table 2). Secondly, intellectual functioning of the patients included in this study may not represent the intellectual status generally reported in the general TSC population. In fact, 82% of our sample had an IQ/DQ below the low average, whereas most studies report that 50% of individuals with TSC have a normal intelligence quotient [39–41]. This may have been influenced by the fact that all patients included in this study have a history of epilepsy, which has been correlated with cognitive impairment [42]. Moreover, almost half of our sample has a history of IS, which is highly associated with poor intellectual functioning [17, 43, 44]. The occurrence of IS in TSC is reported to be 20–30% [45], which is lower than the 49% occurrence we measured in our group. This may also explain the high proportion of our patients with an IQ/DQ below the low average range. Inclusion of patients with TSC without a history of seizure would be interesting in further studies. Finally, it would be very interesting to investigate correlations between tuber types, based on MRI features, and pathological findings obtained from tubers resected from patients with TSC who underwent tubectomy as a surgical epilepsy treatment. This interesting question will be investigated in a future research study.
Conclusion
This is the first study to suggest a classification of three tuber types, distinguishable with conventional MRI, and to investigate the relationship between the different tuber types and severity of clinical symptoms. The presence of different tuber types may suggest multiple distinct molecular processes of tuber formation, or one molecular process under the influence of different modifiers. More studies are needed to better characterize and understand these significant differences of tuber types as well as to investigate the mechanisms underlying the gradient pathophysiology of tubers. In the future, a more precise characterization of each tuber along a spectrum of severity instead of a division of that spectrum into different tuber types may provide more specific information. Nevertheless, the identification of different tuber types represents advancement in understanding the relationship between genotype and clinical manifestations, such as epilepsy or ASD, and will possibly help stratify patients for treatment trials.
References
Roach ES, Sparagana SP (2004) Diagnosis of tuberous sclerosis complex. J Child Neurol 19:643–649
Bozzao A, Manenti G, Curatolo P (2003) Neuroimaging. In: Curatolo P (ed) Tuberous sclerosis complex: from basic science to clinical phenotypes. Mac Keith Press for the International Child Neurology Association, London, pp 109–123
DiMario FJ (2004) Brain abnormalities in tuberous sclerosis complex. J Child Neurol 19:650–657
Griffiths PD, Bolton P, Verity C (1998) White matter abnormalities in tuberous sclerosis complex. Acta Radiol 39:482–486
Ridler K, Suckling J, Higgins N, Bolton P, Bullmore E (2004) Standardized whole brain mapping of tubers and subependymal nodules in tuberous sclerosis complex. J Child Neurol 19:658–665
Crino PB, Trojanowski JQ, Dichter MA, Eberwine J (1996) Embryonic neuronal markers in TS single-cell molecular pathology. Proc Natl Acad Sci USA 93:14152–14157
Hirose T, Schelthauer BW, Lopes MBS, Gerber HA, Altermatt HJ, Hukee MJ et al (1995) Tuber and subependymal giant cell astrocytoma associated with tuberous sclerosis: an immunohistochemical, ultrastructural, and immunoelectron microscopic study. Acta Neuropathol 90:387–399
Braffman BH, Bilaniuk LT, Naidich TP, Altman NR, Post MJ, Quencer RM et al (1992) MR imaging of tuberous sclerosis: pathogenesis of the phakomatosis, use of gadopentetate dimeglumine, and literature review. Radiology 183:227–238
Suronov AA, Wu X, Weiner HL, Mikell CB, Goodman RR, Crino PD et al (2008) Tuberous sclerosis: a primary pathology of astrocytes? Epilepsia 49:53–62
Trombley IK, Mirra SS (1981) Ultrastructure of tuberous sclerosis: cortical tuber and subpendymal tumor. Ann Neurol 9:174–181
Stefansson K, Wollman RL, Huttenlocher PR (1999) Lineage of cells in the central nervous system. In: Gomez MR, Sampson JR, Whittemore VH (eds) Tuberous sclerosis complex, 3rd edn. Oxford University Press, New York, pp 251–262
Doherty C, Goh S, Young Poussaint T, Erdag N, Thiele EA (2005) Prognostic significance of tuber count and location in tuberous sclerosis complex. J Child Neurol 20:837–841
Pinto Gama HP, da Rocha AJ, Braga FT, da Silva CJ, Martins Maia AC Jr, de Campos Meirelles RG et al (2006) Comparative analysis of MR sequences to detect structural brain lesions in tuberous sclerosis. Pediatr Radiol 36:119–125
Crino PB, Nathanson KL, Henske EP (2006) The tuberous sclerosis complex. N Engl J Med 355:1345–1356
Doherty C, Goh S, Poussaint TY, Erdag N, Thiele EA (2006) Prognostic significance of tuber count and location in tuberous sclerosis complex. J Child Neurol 20:837–841
Jansen FE, Vincken KL, Algra A, Anbeek P, Braams O, Nellist M et al (2008) Cognitive impairment in tuberous sclerosis complex is a multifactorial condition. Neurology 70:916–923
O’Callaghan FJ, Harris T, Joinson C, Botton P, Noakes M, Presdee D et al (2004) The relation of infantile spasms, tubers, and intelligence in tuberous sclerosis complex. Arch Dis Child 89:530–533
Schwartz RA, Fernandez G, Kotulska K, Jozwiak S (2007) Tuberous sclerosis complex: advances in diagnosis, genetics, and management. J Am Acad Dermatol 57:189–202
Asano E, Chugani DC, Muzik O, Shen C, Juhász C, Janisse J et al (2000) Multimodality imaging for improved detection of epileptogenic foci in tuberous sclerosis complex. Neurology 54:1976–1984
Chugani DC, Chugani HT, Muzik O, Shah JR, Shah AK, Canady A et al (1998) Imaging epileptogenic tuber in children with tuberous sclerosis complex using α-[11C]methyl-l-tryptophan positron emission tomography. Ann Neurol 44:858–866
Fedi M, Reutens DC, Andermann F, Okazawa H, Boling W, White C et al (2003) alpha-[11C]-Methyl-l-tryptophan PET identifies the epileptogenic tuber and correlates with interictal spike frequency. Epilepsy Res 52:203–213
Jansen FE, Braun KPJ, van Nieuwenhuizen O, Huiskamp G, Vincken KL, van Huffelen AC et al (2003) Diffusion-weighted magnetic resonance imaging and identification of the epileptogenic tuber in patient with tuberous sclerosis. Arch Neurol 60:1580–1584
Major P, Rakowski S, Simon MV, Cheng ML, Eskandar E, Baron J et al (2009) Are cortical tubers epileptogenic? Evidence from electrocorticography. Epilepsia 50:147–154
Pellizzi GB (1901) Contnibuto allo studio dell’idiozia: rivisita sperimentale di freniatnia e medicine legate delle alienazioni mental. Riv Sper Freniatr 27:265–269
Chu-shore CJ, Major P, Montenegro M, Thiele EA (2009) Cyst-like tubers are associated with TSC2 and epilepsy in tuberous sclerosis complex. Neurology 72:1165–1169
Marti-Bonmati L, Menor F, Dosda R (2000) Tuberous sclerosis: differences between cerebral and cerebellar cortical tubers in a pediatric population. AJNR Am J Neuroradiol 21:557–560
Jurkiewicz E, Jozwiak S, Bekiesinska-Figatowska M, Papula-Kosciesza I, Walecki J (2006) Cyst-like cortical tubers in patients with tuberous sclerosis complex: MR imaging with the FLAIR sequence. Pediatr Radiol 36:498–501
Firat AK, Karakas HM, Erdem G, Yakinci C, Bicak U (2006) Diffusion weighted MR findings of brain involvement in tuberous sclerosis. Diagn Interv Radiol 12:57–60
Goh S, Butler W, Thiele EA (2004) Subpendymal giant cell tumors in tuberous sclerosis complex. Neurology 63:1457–1461
Shepherd CW, Gomez MR, Lie JT, Crowson CS (1991) Causes of death in patients with tuberous sclerosis. Mayo Clin Proc 66:792–796
Goodman M, Lamm SH, Engel A, Sheperd CW, Houser OW, Gomez MR (1997) Cortical tuber counts: a biomarker indicating neurologic severity of tuberous sclerosis complex. J Child Neurol 21:85–90
Makki MI, Chugani DC, Janisse J, Chugani HT (2007) Characteristics of abnormal diffusivity in normal-appearing white matter investigated with diffusion tensor MR imaging in tuberous sclerosis complex. AJNR Am J Neuroradiol 28:1662–1667
Sener RN (2002) Tuberous sclerosis: diffusion MRI findings in the brain. Eur Radiol 12:138–143
Chandra PS, Salamon N, Huang J, Wu JY, Koh S, Vinters HV et al (2006) FDG-PET/MRI coregistration and diffusion-tensor imaging distinguish epileptogenic tubers and cortex in patients with tuberous sclerosis complex: a preliminary report. Epilepsia 47:1543–1549
Au KS, Williams AT, Roach ES, Batchelor L, Sparagana SP, Delgado MR et al (2007) Genotype/phenotype correlation in 325 individuals referred for a diagnosis of tuberous sclerosis complex in the United States. Genet Med 9:88–100
Dabora SL, Jozwiak S, Franz DN, Roberts PS, Nieto A, Chung J, Choy YS et al (2001) Mutational analysis in a cohort of 224 tuberous sclerosis patients indicates increased severity of TSC2, compared to TSC1, disease in multiple organs. Am J Hum Genet 68:64–80
Jansen FE, Braams O, Vincken KL, Algra A, Anbeek P, Jennekens-Schinkel A et al (2008) Overlapping neurologic and cognitive phenotypes in patients with TSC1 or TSC2 mutations. Neurology 70:908–915
Strizhera GD, Carsillo T, Kruger WD, Sullivan EJ, Ryu JH, Henske EP (2001) The spectrum of mutations in TSC1 and TSC2 in women with tuberous sclerosis and lymphangiomyomatosis. Am J Resp Crit Care Med 163:253–258
de Vries PJ, Howe CJ (2007) The tuberous sclerosis complex proteins—a GRIPP on cognition and neurodevelopment. Trends Mol Med 13:319–326
Joinson C, O’Callaghan FJK, Osborne JP, Martyn C, Harris T, Bolton PF (2003) Learning disability and epilepsy in an epidemiological sample of individuals with tuberous sclerosis. Psychol Med 33:335–344
Winterkorne EB, Pulsifer MB, Thiele EA (2007) Cognitive prognosis of patients with tuberous sclerosis complex. Neurology 68:62–64
Gomez MR, Sampson JR, Whittemore VH (1999) Tuberous sclerosis complex, 3rd edn. Oxford University Press, New York
Goh S, Kwiatkowski DJ, Dorer DJ, Thiele EA (2005) Infantile spasms and intellectual outcomes in children with tuberous sclerosis complex. Neurology 65:235–238
Jozwiak S, Goodman M, Lamm SH (1998) Poor mental development in patients with tuberous sclerosis complex. Arch Neurol 55:379–384
Curatolo P, Seri S, Verdecchia M, Bomnardieri R (2001) Infantile spasms in tuberous sclerosis complex. Brain Dev 23:502–507
Acknowledgments
We are grateful to Miguel Chagnon, Adam Numis and Larry MacDonald for providing advice and information regarding statistical analysis. This work was supported by a scholarship by the Canadian Institutes of Health Research (CIHR), awarded to Anne Gallagher, Ph.D. as well as by the Carol and James Herscot Center for Tuberous Sclerosis Complex.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gallagher, A., Grant, E.P., Madan, N. et al. MRI findings reveal three different types of tubers in patients with tuberous sclerosis complex. J Neurol 257, 1373–1381 (2010). https://doi.org/10.1007/s00415-010-5535-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-010-5535-2