Abstract
This article describes the clinical features of anterior semicircular canal benign paroxysmal positional vertigo (AC-BPPV) and a new therapeutic maneuver for its management. Our study was a retrospective review of cases from an ambulatory tertiary referral center. Thirteen patients afflicted with positional paroxysmal vertigo exhibiting brief positional down-beating nystagmus in positional tests (Dix–Hallpike and head-hanging position) were treated with a maneuver comprised of the following movements: Sequential head positioning beginning supine with head hanging 30° dependent with respect to the body, then supine with head inclined 30° forward, and ending sitting with head 30° forward. All cases showed excellent therapeutic response to our repositioning procedure, i.e. relief of vertigo and elimination of nystagmus. The maneuver described is an option for AC-BPPV treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo presenting to primary care and neuro-otology clinics [1–4]. The most accepted theory to explain the subjective (brief episodes of vertigo) and objective (positional nystagmus) clinical features is thought to be loose debris (otolith fragments) within the posterior semicircular canal [3, 4]. This debris moves freely inside the endolymphatic system and can thus migrate to any semicircular canal. Epley [5] used the term “vestibular lithiasis” to include the six semicircular canals, all potentially vulnerable to BPPV.
The most common variant, posterior BPPV (PC-BPPV) has an upbeating-torsional nystagmus on positional testing (Dix–Hallpike). Anterior semicircular canal BPPV (AC-BPPV), diagnosed by observation of a similar nystagmus but in a downbeating direction, is not frequent and therapeutic information on this condition is extremely scarce [3, 6, 7]. Recent controlled studies have clearly established that physical maneuvers based on inner ear biomechanics are highly effective for PC-BPPV. In these maneuvers, the head is positioned such that loose otoconia are allowed to sediment within the labyrinth. It seems highly likely that similar maneuvers should be equally effective for anterior canal BPPV. However, as the anterior canal follows a different trajectory from the posterior canal, maneuvers to treat AC-BPPV must necessarily differ geometrically from those described by Epley [8] and Semont [9] for PC-BPPV.
Most anterior canal (AC) treatment studies have used maneuvers which are variants of posterior canal (PC) procedures, beginning with nose-up to the healthy side and eliminating the nose-down portion of Epley or Semont maneuvers. These approaches are reasonable from a biomechanical perspective. On the other hand, use of unmodified PC procedures to treat contralateral AC-BPPV are not biomechanically reasonable, because the final nose-down position of both the Epley and Semont maneuvers should cause debris to move into the anterior canal rather than out of it as desired.
In this regard, there have been several non-controlled studies concerning the treatment of anterior canal BPPV. Honrubia et al. [2] mention a “Reverse Epley” postural repositioning procedure. This maneuver is biomechanically reasonable, but no published data regarding its efficacy is available. The “Reverse Semont” maneuver has also been recommended—as head positions with respect to gravity are identical to those of the Epley maneuver, this procedure is likely to be equally effective. Again, there are no published data concerning efficacy.
Kim and associates [10] studied 30 patients using a procedure based on biomechanical principles. In the Kim maneuver, the patient’s head is rotated 45° away from the affected ear and then lowered to 30° below the horizontal (as in a Dix–Hallpike test, or the first position of the “Epley” maneuver for PC-BPPV). After about 30 s, the patient’s head is elevated while lying in a supine position and the head is kept turned at 45° for 1 min; finally the patient is returned to a sitting position and the chin is tilted downwards (30°). The authors found 96.7% efficacy in over 30 patients (12 AC-BPPV, and 18 multicanal BPPV).
Another maneuver for AC-BPPV was described by Rahko [11]. In this maneuver, the patient lies on the healthy side. The head is first tilted downwards 45° (position 1), then horizontally (position 2), then upwards 45° (position 3) for 30 s in each position; finally the patient sits up (position 4) remaining well supported in this position for at least 3 min. Fifty-three of 57 patients were symptom free after the maneuver. Neither diagnosis nor results were based on nystagmus pattern, nor did the study include a control group or double blind design.
Crevits [12] described a “Prolonged Forced Position procedure” in two patients with refractory AC positional vertigo. Biomechanically, this maneuver differs significantly from the others described, in that there is an explicit effort to position the anterior canal so that it is nearly upside down, rather than attempting to position it 45° to one side as in the variants of the Epley maneuver described above. Crevits rapidly moves the patient from sitting to lying supine with the head bent backwards as far as possible, such that the vertex is about 60° below the horizontal. The head is supported in this hanging position for 30 min and then moved quickly forward as far as possible, with the vertex near the vertical axis. For this position, the head is stabilized with a pulley system. Initial positioning of the head far backward makes this maneuver biomechanically reasonable, but it is very cumbersome due to its prolonged duration and use of hardware; it also requires patient admission to a hospital. Helminski and Hain [13] proposed using a “deep Dix–Hallpike” maneuver for AC-BPPV. Biomechanically, this maneuver resembles the Crevits maneuver but is less cumbersome. These authors presented no data regarding efficacy.
Others treatment alternatives, so far without scientific studies proving efficacy, include the Brandt Daroff exercise and the reverse Semont maneuver. Finally, among surgical alternatives, plugging of the anterior canal has been applied [14].
In summary, several non-controlled studies on treatment of anterior canal BPPV, using reversed CRP methods as their basic methodology, as well as a second type of maneuver (Crevits) applying a prolonged extreme backward head positioning, have been conducted to date. We present our experience with a new and rapid maneuver for anterior canal BPPV treatment, similar to that of Crevits, which appears highly effective.
Materials and methods
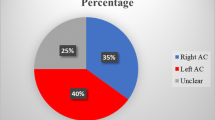
We examined 577 patients diagnosed with BPPV during the past two years at the neurotology unit of our clinic, in order to identify AC-BPPV cases. Among the 577 BPPV patients, 504 (87.3%) were identified with the PC variant, 60 (10.3%) with HC and 13 (2.2%) met criteria for AC-BPPV.
Patients with clinical examination and laboratory findings suggesting pathologic conditions of the central nervous system were excluded from this study. To avoid interference from other canals we also excluded multicanal BPPV cases.
Both Dix–Hallpike and straight-back head-hanging maneuvers were performed on all patients to establish the diagnosis of posterior or anterior canal involvement. Intense vertigo accompanied by a burst of nystagmus with typical characteristics of latency, crescendo, and transience were necessary to confirm the diagnosis. Differential diagnosis between posterior and anterior canal BPPV variants was based on the direction of the vertical component of the fast phase of nystagmus response, being upward and torsional in cases of posterior canal involvement, and downward with or without a torsional component in cases of anterior canal involvement [15]. Horizontal canal BPPV was diagnosed by the presence of horizontal geotropic or apogeotropic paroxysmal nystagmus, provoked by turning the head from the supine to either lateral position.
All AC-BPPV patients underwent complete audiologic and neurotologic evaluation, including pure tone audiometry, videonystagmography (VNG) and brain MRI or CT scan, prior to use of our repositioning maneuver for treatment.
Methods
All patients had clear anterior semicircular canal canalithiasis. In patients 1, 2, 9, 12 and 13, diagnosis was based on the fact that “canal conversion” from the posterior to anterior was observed. Having applied Epley’s Maneuver for PC-BPPV treatment in all these cases, patients returned a few days later complaining of positional vertigo. During the Dix–Hallpike and head-hanging tests, after a short latency period, patients developed brief downbeating positional nystagmus associated with vertigo (Fig. 1). Patients 3–8 presented with positional vertigo 6 months–2 years after being treated for PC-BPPV with the Epley maneuver. Patients 10 and 11 did not present with prior BPPV.
Particle repositioning procedure
Our repositioning maneuver is illustrated in Fig. 2. It consists of four steps, with position changes occurring at 30-s intervals. From the head-straight sitting position (position 1), a head-hanging maneuver is performed so that the head is brought to at least 30° below the horizontal, as shown in Fig. 2 (position 2). During the maneuver, loose otoconia within the anterior canal should move away from the anterior canal cupula, triggering a down beating nystagmus. For patients who are unable to attain a 30° dependent head position, a tilting examination table or “tilt table” can be used to attain the same head position with respect to gravity.
After 30 s, once vertigo and nystagmus provoked by the maneuver cease and while still supine, the patient’s head is moved quickly forward “chin to chest” (position 3), with the vertex near the vertical axis. After another 30 s have elapsed, head and body are brought into the sitting position (position 4), remaining there for another 30 s. In cases of failure or incomplete remission of symptoms, the same maneuver is repeated.
Results
Out of 13 patients with AC-BPPV, using one or more repetitions of the straight-back maneuver described in this paper, all patients became symptom free. After a single maneuver 84.6% of patients were controlled. Over all, it was necessary to perform the maneuver 1.23 times for complete AC-BPPV control. Table 1 shows the most relevant clinical features of AC-BPPV patients.
As an example of a typical pattern we describe case 5: a 91 year-old man with several prior bouts of right PC-BPPV and right HC-BPPV in the last 6 months. Brain CT scan showed mild cortical atrophy. Particle repositioning maneuvers had been successful in the past and the patient had remained free of symptoms until the week prior to clinic visit. Positional tests showed DBN on both right and left Dix–Hallpike maneuvers, and during the head-hanging position. The repositioning maneuver for the AC was implemented successfully.
Discussion
We describe 13 patients with positional DBN and vertigo, 11 of whom responded to a single maneuver, and two who required an additional maneuver. Although this is an uncontrolled case series, and definitive proof requires a randomized controlled trial, these results document a promising new approach to treatment of AC-BPPV.
One might question whether our patients had anterior canal BPPV, since in some of them, during the straight head-hanging maneuver the nystagmus elicited was entirely downbeating, instead of having both downbeating and torsional components as expected according to Ewald’s law [16]. From mathematical modeling of BPPV one may infer that the nystagmus will present with a latency and that its orientation will always be along the plane of the anterior canal [17]. Nevertheless, purely downbeating nystagmus with lack of a torsional component has been previously reported in cases of anterior canal BPPV by Bertholon and associates who suggested that the torsional component is not always present, possibly because of the anterior canal’s anatomical orientation which is closer to the sagittal plane (about 41°) compared to that of the posterior canal (56°). Additionally, because torsional gain of the human vestibular ocular reflex is about 0.75 in response to high-frequency (~2 Hz) roll head impulses [18], the torsional component would be smaller than the horizontal and vertical components, partially explaining observation of a purely down beating nystagmus. Presumably, again due to the nearly sagittal orientation, as our case illustrated, downbeating nystagmus consistent with AC-BPPV can be provoked by the Dix–Hallpike to either side. Also supporting the conclusion that these patients had AC-BPPV, is the observation that other potential mechanisms for downbeating nystagmus (e.g. central causes, cervical vertigo, otolithic disturbances), would not respond to a physical maneuver.
The probable mechanism behind the effectiveness of this maneuver is shown in Fig. 2. In position 1, otoconia lie near the AC ampulla. In position 2 (head-hanging position), both anterior canals are inverted with the ampulla superior, and the non-ampullary ending medial and inferior. Otoconia migrate due to their weight towards the apex of the anterior canal. In position 3 (chin to chest), gravity facilitates further migration towards the common crus. Finally, in position 4, the patient sits up with head tucked in. This last step allows otoconia to move through the common duct (crus) and into the vestibule. At least 30 s in each position is advisable to give otoconia time to migrate, as even under a full ‘g’ of force, otoconia move down only about 1% of canal diameter per second [19].
With this maneuver we do not need to know which anterior canal is affected. Lopez-Escamez et al. [20] found bilateral positional downbeating nystagmus was triggered by the DH maneuver in 5 of 14 AC-BPPV patients, with difficulty localizing the affected ear. For triggering anterior canal BPPV, strict rotation in the canal plane is of relatively less importance than a final low head-down position. During head-hanging, the head reaches a more dependent position by about 20°, than during the Dix–Hallpike position. This may be crucial for provoking anterior canal BPPV [6]. It is likely, as suggested by Bertholon [6], that the straight head-hanging maneuver is the best way to trigger AC-BPPV, and in our current diagnostic protocol, we use this maneuver when the Dix–Hallpike and HC-BPPV maneuvers are negative. According to our observations, this repositioning maneuver works symmetrically for unilateral AC-BPPV (regardless of which side is affected). Therefore identifying the affected ear should not be critical under these conditions.
What if the maneuver does not work? In this case, we would advise repeating it several times and waiting a longer period in the initial head-hanging position, as well as between positions. If it still does not work, we suggest completing the work up to rule out other reasonable causes, such as central positional vertigo (e.g. nodulus lesion) [21]. Using high-resolution 3D MRI, Schratzenstaller et al. [22] found morphological abnormality at the top of the superior semicircular canal (generating a stop to free floating otoconia) in patients with AC-BPPV resistant to therapy, particularly in patients with previous ear surgery or ear disease.
Conclusions
AC-BPPV is a rare condition presenting with positional downbeating nystagmus. Absence of the torsional component does not rule out AC involvement. We suggest, for patients with positional vertigo in whom the Dix–Hallpike maneuver is negative or shows downbeating nystagmus, completing the exam with the HH maneuver and following the procedure described here to treat AC-BPPV.
References
Bronstein AM (2003) Vestibular reflexes and positional manoeuvres. J Neurol Neurosurg Psychiatry 74:289–293. doi:10.1136/jnnp.74.3.289
Honrubia V, Baloh RW, Harris MR, Jacobson KM (1999) Paroxysmal positional vertigo syndrome. Am J Otol 20:465–470
Furman JM, Cass SP (1999) Benign paroxysmal positional vertigo. N Engl J Med 341:1590–1596. doi:10.1056/NEJM199911183412107
Parnes LS, Agrawal SK, Atlas J (2003) Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ 169:681–693
Epley JM (2001) Human experience with canalith repositioning maneuvers. Ann N Y Acad Sci 942:179–191
Bertholon P, Bronstein AM, Davies RA, Rudge P, Thilo KV (2002) Positional down beating nystagmus in 50 patients: cerebellar disorders and possible anterior semicircular canalithiasis. J Neurol Neurosurg Psychiatry 72:366–372. doi:10.1136/jnnp.72.3.366
Herdman SJ, Tusa RJ (1996) Complications of the canalith repositioning procedure. Arch Otolaryngol Head Neck Surg 122:281–286
Epley JM (1992) The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 107:399–404
Semont A, Freyss G, Vitte E (1988) Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol 42:290–293
Kim YK, Shin JE, Chung JW (2005) The effect of canalith repositioning for anterior semicircular canal canalithiasis. ORL J Otorhinolaryngol Relat Spec 67:56–60. doi:10.1159/000084336
Rahko T (2002) The test and treatment methods of benign paroxysmal positional vertigo and an addition to the management of vertigo due to the superior vestibular canal (BPPV-SC). Clin Otolaryngol Allied Sci 27:392–395. doi:10.1046/j.1365-2273.2002.00602.x
Crevits L (2004) Treatment of anterior canal benign paroxysmal positional vertigo by a prolonged forced position procedure. J Neurol Neurosurg Psychiatry 75:779–781. doi:10.1136/jnnp.2003.025478
Helminski JO, Hain TC (2007) Evaluation and treatment of benign paroxysmal positional vertigo. Ann Long Term Care 15(6):33–39
Brantberg K, Bergenius J (2002) Treatment of anterior benign paroxysmal positional vertigo by canal plugging: a case report. Acta Otolaryngol 122:28–30. doi:10.1080/00016480252775698
Herdman SJ (1997) Advances in the treatment of vestibular disorders. Phys Ther 77:602–618
Ewald JR (1892) Physiologische Untersuchungen über das Endorgan des Nervus octavus. Bergmann, Wiesbaden
Squires TM, Weidman MS, Hain TC, Stone HA (2004) A mathematical model for top-shelf vertigo: the role of sedimenting otoconia in BPPV. J Biomech 37:1137–1146. doi:10.1016/j.jbiomech.2003.12.014
Aw ST, Todd MJ, Aw GE, McGarvie LA, Halmagyi GM (2005) Benign positional nystagmus: a study of its three-dimensional spatio-temporal characteristics. Neurology 64:1897–1905. doi:10.1212/01.WNL.0000163545.57134.3D
Hain TC, Squires TM, Stone HA (2005) Clinical implications of a mathematical model of benign paroxysmal positional vertigo. Ann N Y Acad Sci 1039:384–394. doi:10.1196/annals.1325.036
Lopez-Escamez JA, Molina MI, Gamiz MJ (2006) Anterior semicircular canal benign paroxysmal positional vertigo and positional downbeating nystagmus. Am J Otolaryngol 27:173–178. doi:10.1016/j.amjoto.2005.09.010
Fernandez C, Alzate R, Lindsay JR (1960) Experimental observations on postural nystagmus. II. Lesions of the nodulus. Ann Otol Rhinol Laryngol 69:94–114
Schratzenstaller B, Wagner-Manslau C, Strasser G, Arnold W (2005) Canalolithiasis of the superior semicircular canal: an anomaly in benign paroxysmal vertigo. Acta Otolaryngol 125:1055–1062. doi:10.1080/00016480510037023
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yacovino, D.A., Hain, T.C. & Gualtieri, F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol 256, 1851–1855 (2009). https://doi.org/10.1007/s00415-009-5208-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5208-1