Abstract
There is insufficient evidence to support the use of exercise in the management of chronic disablement in people with inflammatory peripheral neuropathy. Therefore, our study aimed to determine the feasibility and effectiveness of a physiotherapist prescribed community based exercise programme for reducing chronic disablement in patients with stable motor neuropathy.
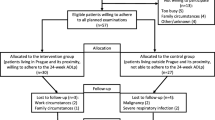
We assessed the effects of a 12 week unsupervised, community based strengthening, aerobic and functional exercise programme on activity limitation and other measures of functioning in 16 people with stable motor neuropathy and 10 healthy control subjects.
Fourteen of 16 patients and 8 out of 10 healthy control subjects completed the study and exercised safely in the community with no adverse events. Significant improvements were seen in all measures of activity limitation and in wider measures of health including anxiety, depression and fatigue in the patient group. Improvements were sustained at six months after completion of the exercise programme, except for depression. Ten patients continued to exercise regularly at six months.
These findings demonstrate that individually prescribed community based exercise is feasible and acceptable for people with stable motor neuropathy and participation in exercise may be successful in reducing chronic disablement. Future randomised controlled trials are needed to examine the efficacy of this complex community based intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lasting symptoms of inflammatory peripheral neuropathy (PN), common after Guillain-Barré syndrome (GBS) and in Chronic inflammatory demyelinating Polyradiculneuropathy (CIDP), [6, 7, 9, 33] may contribute to persistent disablement, [19] reduced health status and difficulty returning to work and hobbies [7]. Such chronic disablement often results in a sedentary lifestyle, leading to increased health risks including obesity, cardiovascular disease and poor mental health [21, 32]. Exercise can reduce or prevent secondary health complications exacerbated by inactivity and also improve well-being [2, 11, 34, 37]. Exercise has also been shown to be beneficial in reducing disablement in patients with other neurological conditions [10, 28, 39]. However, a recent systematic review concluded that there was insufficient evidence with which to evaluate the effect of exercise on functional ability in people with peripheral neuropathy [38]. Clinical studies of targeted exercise in this patient group have shown some improvements in residual impairments such as strength, endurance and cardiovascular fitness [12, 31]. However, few have examined the effect of exercise on overall functioning, such as changes in activities and participation, despite these outcomes being of great importance to patients [12, 30, 31]. Furthermore, no published studies have examined exercise behaviour after the intervention period, although continued exercise is necessary to maintain general health improvements [8]. Individually tailored combinations of strengthening, aerobic and functional exercise carried out at home or in the local community might promote exercise adherence and optimise the functional impact for people with inflammatory PN. Therefore, we aimed to investigate the feasibility, acceptability and efficacy of a prescribed 12 week community based combined exercise programme for people after GBS or with CIDP.
Methods
Sixteen adult volunteers were recruited prospectively from patients attending the Peripheral Nerve Clinic at Guy’s Hospital, London and from the Guillain-Barré Syndrome Support Group - UK, a patient support organisation. Patients were included if they were at least one year after nadir of their GBS or had stable CIDP and fulfilled standard diagnostic criteria [3, 14, 27]. To be included patients must have had no change in self reported disability or medication in the previous 6 months. Volunteers were excluded if they had any medical condition that prevented exercise or where they were unsafe to exercise, if they were pregnant or if they were receiving regular immunoglobulin or plasma exchange treatment. Patients underwent a neurological and medical examination to ensure their fitness for exercise and all participants were assessed by a physiotherapist to determine their level of impairment and function. If necessary, participants were referred for professional orthotic prescription and the exercise programme was delayed until appropriate orthotic support was provided.
Ten healthy, sedentary subjects from staff and students of King’s College London were also recruited, underwent medical screening and followed the same assessment and exercise programme as the PN group in order to ascertain the effectiveness of the exercise programme, All outcomes, except disability and disease specific measures, were also assessed pre and post exercise in this group.
Local ethical approval was granted and the study was in accordance with the 1964 Declaration of Helsinki. All participants gave their informed consent prior to inclusion in the study.
Assessments
Primary outcome measure
Disability or activity limitation, was measured using the disease specific Overall Disability Sum Score (ODSS) [23]. The Short Form 36 questionnaire (SF-36) was also used to measure aspects of disablement including physical and mental function and health related quality of life [36]. Both the ODSS and SF-36 have been shown to demonstrate moderate to good validity and responsiveness in people with immune mediated peripheral neuropathies [23, 24].
Secondary outcome measures
These included the Hospital anxiety and depression scale (HADS) [41] and the fatigue severity scale (FSS) [18] both of which have been used in PN [12]. Isometric muscle strength of shoulder abductors, elbow and wrist extensors, hip flexors and ankle dorsiflexors was measured using a hand-held dynamometer [5] and knee extensors using fixed dynamometry. In addition, participants performed a graded symptom limited exercise test on a stationary bicycle to determine peak heart rate and workload [26]. Following a warm up during which participants cycled for 3 minutes at 60 RPM against no resistance, the workload was increased by 30 Watts every minute until participants were unable to maintain the speed of cycling. All measurements were repeated twice, one month apart, before the start of exercise. The first set familiarised participants with the procedures. One rater took all the measurements. Subsequent measurements were taken half way through (after 18 exercise sessions) and at the end of the exercise programme (after 36 sessions). Subjects with PN were also retested at 6 months after the end of the programme. In addition, a pragmatic sub-group of four healthy and five PN subjects wore activity monitors for five days before and after the exercise programme to assess overall activity levels (MTI ActiGraph, Florida). The monitors were worn at waist height and recorded movement, using accelerometers which sampled every minute. The results were expressed as mean activity counts per minute, and were assessed over five days to give a representation of overall activity levels. An informal semi-structured interview was carried out at the end of exercise and six month follow-up which asked participants about the acceptability of the exercise programme, their general health and well being and whether they continued to exercise.
Exercise Programme
Each exercise session was designed to take approximately one hour. Participants exercised in their local community (either at home or a local leisure facility), three times a week for 12 weeks or until they had competed 36 sessions. All components of the exercise session were prescribed by a physiotherapist who ensured participants could perform each exercise safely and effectively.
Each exercise session consisted of aerobic, strengthening and functional exercises. Subjects began with a 10 minute warm up at below 60% of their peak heart rate (HR max) which was determined from the graded exercise test. This was followed by 20 minutes of the participants chosen aerobic exercise at 65–85% of their HR max. Seven subjects in the PN group exercised by cycling, 6 by walking and one by rowing. Four healthy participants exercised by either walking or running, 3 cycled and one rowed. During aerobic exercise, subjects monitored their own heart rate by using a Polar heart monitor (Polar®, Finland) which was pre-programmed to give audible and/or visual feedback if the heart rate fell below or rose above the prescribed range. Individual strengthening exercises were determined by each participant’s clinical presentation. Strengthening exercises comprised 10 second maximal isometric contractions against resistance. Exercise intensity commenced at the patients tolerance but progressed to a maximum of 3 sets of 10 repetitions over the 12 week exercise programme. Functional exercises, included balance and task specific exercises, such as moving from sit to stand, bilateral squats and were selected to target areas of individuals’ functional difficulty or regional weakness. Each exercise session was completed with stretches for major lower limb muscle groups, after a five minute warm down
Adherence and compliance were monitored by self-completed diaries of the actual exercise undertaken. In addition, all participants were contacted by telephone or email shortly after exercise prescription to check that they were confident to exercise independently and on a weekly basis thereafter if required or requested to assist in progression of exercise and to monitor adverse events.
Analysis
All results are presented as mean ± standard deviation (SD) or median (range) unless otherwise stated.
Independent t and Mann Whitney tests were used to determine significant differences between healthy and PN groups at baseline. Since there were no significant differences between baseline measures, the second baseline measures were used for all analyses.
Results after intervention were analysed using repeated measures ANOVA or Friedman’s tests to determine differences from baseline to completion of the programme and from baseline to six month follow up. Post-hoc analyses using paired t- or Wilcoxon tests were carried out where a significant difference was identified. No adjustments were made for multiple comparisons [29].
Confidence limits (95%) of the mean or median change were calculated for measures showing significant differences between baseline and end of the programme. All data were analysed using SPSS© software (SPSS Inc. version 11.5.1.).
Results
Group characteristics
Two patients were provided with ankle foot orthoses before starting the exercise programme. This was in order to ensure that patients were safe to exercise by providing support for joints at risk of soft tissue damage during sustained activity.
One patient was excluded as medication was changed shortly after starting exercise and a second patient had to leave the study at half way due to personal circumstances unrelated to their health or exercise. Data were analysed for the remaining 14 participants after exercise completion and baseline characteristics for the healthy and PN groups are shown in (Table 1). Full six month follow-up data were available for 13 participants because one participant was unable to attend for testing but completed all subjective data over the telephone.
In the healthy group, two participants left the study after half way, one after an accidental injury unrelated to exercising and the other for unrelated personal reasons.
There were no significant differences between healthy and PN groups in height, weight or age. However, body mass index (BMI) was significantly higher in the PN group. Twelve PN participants reported either lower or upper limb involvement, or both, on the ODSS and only two reported no problems in either upper or lower limbs (Table 1). Ten participants reported altered sensation.
The baseline fatigue severity and SF-36 scores are given in Table 2 and show that the healthy participants (median score:3.3, range 2.7–3.7), were significantly less fatigued than neuropathy participants, (4.6, 1.5–6.1, p < 0.01). Healthy participants also had significantly less physical limitations on the physical component summary (PCS) and physical function subscale (PF) of the SF-36 questionnaire than PN subjects at baseline.
Effectiveness of exercise programme
Healthy group
The response of healthy subjects to strengthening and aerobic exercise suggested that the exercise intensity was sufficient to produce improvements. There was a significant moderate improvement of 15–20% in maximal isometric knee extensor force after exercise (see Fig. 1). Although there was no change in healthy participants’ peak workload as assessed during the graded exercise test, there was a small improvement in total workload (627 ± 302 to 662 ± 263 Watts). However, this was not statistically significant.
PN group
The majority of participants with PN showed moderate increases in isometric muscle strength of trained muscles at the end of the intervention. A significant improvement in muscle strength was seen in the knee extensors, the only muscle group to be exercised by all subjects. This is shown in Fig. 1.
As with healthy subjects, peak workload production during symptom limited exercise testing was not significantly different after training in people with PN. However, total workload after exercise (562 ± 419 Watts) was significantly greater than before (467 ± 306, p < 0.05). This improvement was due to participants being able to exercise for longer at their peak load. Greater improvements in total and peak workload may have been masked by the large increases in workload after each minute during the exercise test. Despite this limitation, the exercise programme appeared to be effective in increasing strength and fitness in both the healthy and PN group.
Adherence to exercise programme
According to records from the self-completed diaries, adherence to the exercise programme was good. Participants with PN reported completing a mean of 37 ± 3 sessions over a mean period of 3 months and 20 days ± 1 month 13 days. Healthy subjects completed a mean of 36 ± 1 sessions over a mean time of three months 15 days ± 16 days.
All patients and healthy subjects exercised without injury; although half of participants in both the healthy (4 out of 8) and the PN group (7 out of 14) reported experiencing minor muscle ache and mild joint stiffness which eased after 48 hours, at the start of the programme, and did not prevent exercise. Four PN patients and 8 healthy participants exercised at their local gym. The remaining participants exercised at home. All exercise equipment and membership fees were provided or paid for by funders of the study.
Patients with PN reported positive changes in energy level, motivation and mood at an informal exit interview after the intervention. All participants felt the programme was realistic, beneficial and practical to complete.
Effect of exercise on primary outcome of change in disability or activity limitation
As shown in Table 2, scores on the SF-36 questionnaire in healthy subjects remained unchanged and within normal limits after completion of exercise. For patients with PN, ODSS scores improved significantly after exercise and there was a significant improvement in functioning as measured by the physical function score of the SF-36 after completion of exercise.
Effect of exercise on secondary outcomes
Anxiety, depression and fatigue were significantly reduced after exercise in patients with PN and fatigue was significantly reduced in healthy participants also (see Table 2).
The mean activity levels of 5 patients, measured as mean counts per minute over 5 days increased significantly from 190 ± 21, to 353 ± 155 countsmin−1 (p = 0.04). The healthy exercise group showed no significant change in average activity levels: 268 ± 107 to 286 ± 82 countsmin−1.
Outcome at follow up: six months after completion of the exercise programme
All 14 PN participants were contacted six months later and 13 patients were available for testing. Improvements in activity limitation, mood and fatigue remained significant compared with baseline, with the exception of the depression subscale of the HADS questionnaire. Isometric muscle strength and workload were no longer significantly different from baseline at 6 months. Subjectively, 11 of 14 contacted participants reported “feeling better” than prior to starting the exercise programme and three felt they were the same. None felt worse than before exercise and 6 reported feeling even better than when they had completed the programme, whilst 4 felt the same. Ten participants were still participating in regular exercise at six months. Of the 4 that did not continue exercising, three felt worse than immediately after completion of the exercise programme. Reasons for not continuing exercise were related to time pressures on individual lifestyles.
Discussion
This study aimed to investigate the effect of physiotherapist prescribed community based exercise on disablement in people with inflammatory peripheral neuropathy. The target client group for this type of intervention was patients complaining of either persistent impairment due to PN or chronic limitation of activity for whom curative medical treatment was not available or inadequate. For such patients, self-management by regular exercising would be attractive if it could be shown beneficial. The study design was influenced by factors which made recruitment into a randomised research study difficult. Both GBS and CIDP are uncommon, [15, 20] and finding patients with stable disease and no disqualifying medical conditions was difficult. In addition, the nature of exercise interventions is such that randomisation to intervention versus control groups is not acceptable to many possible participants and may interfere with aspects of the complex intervention prescribed [13]. Therefore we acknowledge that the prospective intervention design chosen introduces bias and thus the interpretation of the results should be viewed with appropriate caution.
Sample size prior to intervention was based on previous studies [31] and 14 people with PN were recruited and completed the study. Post-hoc calculations using the physical component score (PCS) of the SF-36 reveal that the study had 0.87 power at 12 weeks. The majority of initially recruited healthy subjects and patients with PN successfully completed the exercise programme and were able to exercise safely unsupervised in the community setting. Two patients and two healthy control subjects withdrew from the study after beginning to exercise for reasons unconnected to exercise. Overall, adherence to the programme judged from participant completed diaries and telephone contact was good and similar to previous community based studies in neuromuscular disease [1, 16, 40]. Informal exit interviews revealed that participants found the programme uncomplicated and enjoyed exercising. Several felt that the programme had restored their confidence in their ability to exercise safely and effectively, and 10 continued to exercise at 6 months. Inevitably, life events and lifestyle commitments were reasons stated as being responsible for three patients and 4 healthy control subjects not completing the 36 sessions within the planned 12 weeks. Thus whilst lifestyle factors are an inevitable challenge to continuing regular exercise, a community based unsupervised exercise programme as described here may offer patients the flexibility to manage their time [4, 17] and therefore adhere more effectively to the programme.
The results of the study suggest show that participation in regular exercise reduces activity limitation in patients with PN. The median change of one point on the ODSS represents a significant improvement in activity that was determined as meaningful to patients when reported by others using a near identical scale [13]. This improvement was maintained at 6 month follow up. Similar significant improvements in both physical function and the PCS of the SF-36 were also observed which meant that after exercise, PCS scores for patients with PN were no longer significantly different from the healthy subjects and scores were within normal, population derived values [35]. This is consistent with changes reported in previous studies [12, 31].
Fatigue and anxiety are two factors thought to contribute to reduced activity and persistent disablement in PN [19, 22]. In this study, following exercise and at 6 month follow up, patients with PN showed a significant reduction in fatigue, of similar magnitude to those reported by other authors [12]. Anxiety levels improved and remained significantly lower than baseline when retested at 6 months. Healthy subjects also reported significantly less fatigue after completion of the exercise programme and this suggests that people who exercise regularly feel less tired. More importantly in the subgroup of patients with PN that wore activity monitors to evaluate their overall activity levels, the reduction in fatigue was accompanied by a significant increase in overall activity levels. This was not seen in the healthy group and could indicate that fatigue may have been preventing patients from being more active.
The extent to which underlying impairments in muscle strength and endurance are responsible for disability or activity limitation has been suggested to be quite significant for patients with PN [25]. However, our study shows that only small improvements in isometric muscle strength and total workload on exercise testing were achieved after exercising (in both patients and healthy subjects) and these were not maintained at 6 months. Therefore it is likely that exercise intervention has an effect on activity and participation that is somewhat independent of levels of impairment.
Conclusion
Community based, individually tailored exercise was feasible and well tolerated in participants with peripheral neuropathy. A 12 week exercise intervention produced benefits in activities, with improved physical functioning and decreased limitations still evident 6 months after completion of the exercise programme. Activity levels were also raised after the programme, and many participants reported continuing to exercise, indicating long term changes in health behaviour. The current study design aimed to mimic the complex nature of exercise intervention for this client group to demonstrate the effect of participation in regular exercise on activity limitation. The mechanisms by which the intervention produced improvements in activities and quality of life are not known. However, several factors including reduction in impairment, effects on mental well being, contact with a medical professional and belief in the effectiveness of exercise may account for the benefits reported by the participants. These factors are likely to be replicated in a clinical setting where exercise is prescribed by a physiotherapist and do not detract from or lessen the overall benefit experienced by individual patients. However, a randomised controlled trial would be recommended to eliminate observer bias and examine whether exercise is beneficial for people with PN.
References
Agre JC, Rodriquez A, Franke T (1997) Strength, Endurance and work capacity after muscle strengthening exercise in post polio subjects. Arch Phys Med Rehab 78:681–686
American College of Sports Medicine (1995) ACSM’s guidelines for exercise testing and prescription. Williams & Wilkins, Philadelphia
Asbury AK, Cornblath DR (1990) Assessment of current diagnostic criteria for Guillain-Barré syndrome. Ann Neurol 27:S21–S24
Ashworth N, Chad K, Harrison E, Reeder B, Marshall S (2005) Home versus center based physical activity programs in older adults. Cochrane Database Syst RevCD004017
Bohannon RW (1997) Reference values for extremity muscle strength obtained by hand-held dynamometry from adults aged 20 to 79 years. Arch Phys Med Rehabil 78:26–32
Bouchard C, Lacroix C, Plante V, Adams D, Chedru F, Guglielmi JM, Said G (1999) Clinicapathological findings and prognosis of Chronic Inflammatory Demyelinating Polyradiculoneuropathy. Neurology 52:498–503
de Jager AEJ, Minderhoud JM (1991) Residual signs in Guillain-Barré syndrome: analysis of 57 patients. J Neurol Sci 104:151–156
Dishman RK (1990) Determinants of participation in physical activity. In: Bouchard C (ed) Exercise, Fitness and Health. Human Kinetics, Champaign, llinois, pp. 75–100
Dornonville de la CC, Jakobsen J (2005) Residual neuropathy in long-term population-based follow-up of Guillain-Barré syndrome. Neurology 64:246–253
Duncan P, Richards L, Wallace D, Stoker-Yates J, Luchies P, Ogle A, Studenski S (1998) A randomized controlled pilot study of a home based exercise program for individuals with mild and moderate stroke. Stroke 29:2055–2060
Fox K (1999) The influence of physical activity on mental well-being. Public Health Nutr 2:411–418
Garssen MP, Bussmann JB, Schmitz PI, Zandbergen A, Welter TG, Merkies IS, Stam HJ, van Doorn PA (2004) Physical training and fatigue, fitness, and quality of life in Guillain-Barré syndrome and CIDP. Neurology 63:2393–2395
Hawe P, Shiell A, Riley T (2004) Complex interventions: how “out of control” can a randomised controlled trial be? BMJ 328:1561–1563
Hughes RA, Bensa S, Willison HJ, Van der Bergh P, Comi G, Illa I, Nobile-Orazio E, Van Doorn P, Dalakas M, Bojar M, Swan A (2001) Randomized Controlled Trial of Intravenous Immunoglobulin Versus Oral Prednisolone in Chronic Inflammatory Demyelinating Polyradiculoneuropathy. Ann Neurol 50:195–201
Hughes RA, Rees JH (1997) Clinical and epidemiologic features of Guillain-Barré syndrome. J Infect Dis 176:S92–S98
Kilmer DD, McCrory MA, Wright NC, Aitkens SG, Bernauer EM (1994) The effect of a high resistance exercise program in slowly progressive neuromuscular disease. Arch Phys Med Rehabil 75:560–563
King AC, Haskell WL, Taylor CB, Kraemer HC, DeBusk RF (1991) Group- vs home-based exercise training in healthy older men and women. A community-based clinical trial. JAMA 266:1535–1542
Krupp LB, Coyle PK, Doscher NP, Miller A, Cross AH, Jandorf L, Halper J, Johnson B, Morgante L, Grimson R (1995) Fatigue therapy in multiple sclerosis: results of a double blind, randomized, parallel trial of amantadine, pemoline and placebo. Neurology 45:1956–1961
Lennon SM, Koblar S, Hughes RA, Goeller J, Riser AC (1993) Reasons for persistent disability in Guillain Barré Syndrome. Clin Rehabil 7:1–8
Lunn MP, Manji H, Choudhary PP, Hughes RA, Thomas PK (1999) Chronic inflammatory demyelinating polyradiculoneuropathy: a prevalence study in south east England. J Neurol Neurosurg Psychiatry 66:677–680
McDonald CM (2002) Physical activity, health impairments, and disability in neuromuscular disease. Am J Phys Med Rehabil 81:S108–S120
Merkies IS, Schmitz PI, Samijn JP, van der Meché FG, van Doorn PA (1999) Fatigue in immune-mediated polyneuropathies. European Inflammatory Neuropathy Cause and Treatment (INCAT) Group. Neurology 53:1648–1654
Merkies IS, Schmitz PI, van der Meché FG, Samijn JP, van Doorn PA, Inflammatory Neuropathy Cause, Treatment (INCAT) group (2002) Clinimetric evaluation of a new overall disability scale in immune mediated polyneuropathies. J Neurol Neurosurg Psychiatry 72:596–601
Merkies IS, Schmitz PI, van der Meché FG, Samijn JP, van Doorn PA, Inflammatory Neuropathy Cause, Treatment (INCAT) group (2002) Quality of life complements traditional outcome measures in immune-mediated polyneuropathies. Neurology 59:84–91
Merkies ISJ, Schmitz PIM, van der Meché FGA, Samijn JPA, van Doorn PA (2003) Connecting impairment, disability, and handicap in immune mediated polyneuropathies. J Neurol Neurosurg Psychiatry 74:99–104
Mullis R, Campbell IT, Wearden AJ, Morriss RK, Pearson DJ (1999) Prediction of peak oxygen uptake in chronic fatigue syndrome. Br J Sports Med 33:352–356
Nicolas G, Maisonobe T, Le Forestier N, Leger J, Bouche P (2002) Proposed revised electrophysiological criteria for chronic inflammatory demyelinating polyradiculoneuropathy. Muscle Nerve 25:26–30
Oken BS, Kishiyama S, Zajdel D, Bourdette D, Carlsen J, Haas M, Hugos C, Kraemer DF, Lawrence J, Mass M (2004) Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology 62:2058–2064
Perenger TV (1998) What’s wrong with Bonferroni Adjustments? BMJ 316:1236–1238
Rothwell PM, McDowell Z, Wong CK, Dorman PJ (1997) Doctors and patients don’t agree: Cross sectional study of patient’s and doctors’ perceptions and assessments of disability in multiple sclerosis. BMJ 314:1580–1583
Ruhland JLS (1997) The effects of a home exercise program on impairment and health-related quality of life in persons with chronic peripheral neuropathies. Phys Ther 77:1026–1039
Santiago M, Coyle C (2004) Leisure-time physical activity and secondary conditions in women with physical disabilities. Disabil Rehabil 26:485–494
Sghirlanzoni A, Solari A, Ciano C, Mariotti C, Fallica E, Pareyson D (2000) Chronic inflammatory demyelinating polyradiculoneuropathy: long-term course and treatment of 60 patients. Neurol Sci 21:31–37
Villeneuve PJ, Morrison HI, Craig CL, Schaubel DE (1998) Physical activity, physical fitness, and risk of dying. Epidemiology 9:626–631
Ware JE, Kosinski M (2003) SF-36 Physical and mental health summary scales: A manual for users of version 1. QualityMetric Incorporated, Lincoln
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). Med Care 30:473–483
Weyerer S, Kupfer B (1994) Physical exercise and psychological health. Sports Med 17:108–116
White CM, Pritchard J, Turner-Stokes L (2004) Exercise for people with peripheral neuropathy. Cochrane Database Syst Rev
White LJ, McCoy SC, Castellano V, Gutierrez G, Stevens JE, Walter GA, Vandenborne K (2004) Resistance training improves strength and functional capacity in persons with multiple sclerosis. Mult Scler 10:668–674
Wright NC, Kilmer DD, McCrory MA, Aitkens SG, Holcomb BJ, Bernauer EM (1996) Aerobic walking in slowly progressive neuromuscular disease: effect of a 12-week program. Arch Phys Med Rehab 77:64–69
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 87:361–370
Acknowledgements
We thank the participants who took part in the study, Dr J Pritchard, Dr D Allen and Professor John Ernsting for assistance with screening participants, David Lloyd gyms and the Thomas Guy Club for providing exercise facilities. We thank the Guy’s and St Thomas’ Charity and the Guillain-Barré Syndrome Support group for financial support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Received in revised form: 3 April 2006
Rights and permissions
About this article
Cite this article
Graham, R., Hughes, R. & White, C. A prospective study of physiotherapist prescribed community based exercise in inflammatory peripheral neuropathy . J Neurol 254, 228–235 (2007). https://doi.org/10.1007/s00415-006-0335-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0335-4