Abstract
Background
The diagnosis of skin wound vitality is currently based on standard histology, but histological findings lack sensitivity in case of a short survival time. New reliable biomarkers of vitality are therefore strongly needed. We assessed the ability of 10 candidate cytokines (IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, TNF-α) to discriminate between vital and early post-mortem wounds.
Methods
Twenty-four cadavers with a recent open skin wound (< 3 h) were included (20 men, 4 women, mean age = 51.0 ± 24.3 years). An early post-mortem wound was performed in an uninjured skin area, and both wounds were sampled at the autopsy (post-mortem interval (PMI) = 66.3 ± 28.3 h). Needle-puncture sites related to resuscitation cares were included as very early post-mortem wounds (n = 6). In addition to standard histology, cytokines levels were simultaneously measured in each sample using a multiplex sandwich immunoassay, then normalized on healthy skin levels. A quantitative evaluation of IL-8-positive cells in ante- and post-mortem wound samples was also performed.
Results
In the training set of samples (n = 72), cytokine levels were significantly higher in vital wounds (mean age = 47 ± 53 min) than in post-mortem wounds (mean PMI = 6.9 ± 9.0 h) (p < 0.2), except for two cytokines (IFN-γ and IL-2). IL-8 was the best discriminatory cytokine (Se = 54%, Sp = 100%, AUC = 0.79), while a multivariate model combining IL-4 and IL12p70 was a bit more discriminant (Se = 55%, Sp = 100%, AUC = 0.84). In the validation set (n = 72), the discriminatory power of the cytokines and the predictive model was slightly lower, with IL-8 remaining the best cytokine (Se = 46%, Sp = 96%, AUC = 0.75). The predictive model remained highly specific (Sp = 100%). Both the cytokines and the predictive model allowed the iatrogenic injuries to be correctly classified as post-mortem wounds. Standard histology and immunohistochemistry showed 21% sensitivity and a specificity of 79% and 100%, respectively. Only two iatrogenic wounds could be properly categorized histologically.
Conclusion
This study suggests that cytokines could be useful biomarkers of skin wound vitality and that the immunoassay method could be more sensitive than immunohistochemistry to identify wounds with a short survival time. Further research is underway to confirm these preliminary data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The determination of wound vitality is a major issue in forensic medicine. Forensic pathologists are often required to determine whether an injury occurred while the person was alive (ante-mortem wound) or after death (post-mortem wound), as it can contribute to the reconstruction of crime scenes [1,2,3,4].
The diagnosis of vitality is currently based on conventional histological findings, in the first line of which are early cellular reactions. The infiltration of polymorphonuclear neutrophils is known to be the only reliable histological criterion to differentiate recent ante-mortem from post-mortem wounds [5]. However, the diagnosis of vitality is challenging when dealing with injuries sustained shortly before death, as neutrophils have been found to flock to the wound site with varying delays (from a few minutes to several hours) [3, 6] due to a number of influencing factors including age, diseases, or medications [7]. The identification of new reliable biomarkers of vitality in the early post-traumatic interval is therefore crucial.
In the last decades, many molecules involved in skin wound repair and expressed at the injury site prior to the standard histological pattern of inflammation have been investigated by various ancillary methods, including histochemistry, biochemistry, and immunohistochemistry [8, 9].
Several immunohistochemical studies have yielded encouraging results in wound vitality. For instance, adhesion molecules such as E-selectin or CD15 have been detected in vital skin wounds with a short survival time, while no expression of these markers has been noticed in post-mortem injuries [10, 11]. Numerous other immunohistochemical markers have been used to assess wound vitality including cytokines [12,13,14], growth factors [15], and enzymes [10], with positive staining sometimes observed within the first minutes after wound infliction. However, most studies on recent wounds have shown a relatively low sensitivity and for several markers a risk of post-mortem false positivity [8]. Therefore, other independent investigations are needed before using immunohistochemistry in daily practice.
Besides immunohistochemistry, biochemical methods such as enzyme-linked immunosorbent assays (ELISA) have also shown promising results in this field. In particular, a few studies suggest that the quantification of cytokines in the cutaneous tissues could be of interest for assessing wound vitality, as high levels of cytokines have been found in early-stage skin wounds, while these markers proved to be only slightly expressed in healthy skin [16,17,18,19]. Different cytokines including interleukins (IL), interferons (IFN), and tumour necrosis factors (TNF) have been investigated, but none of them has been definitely validated as a reliable marker of vitality in the early post-traumatic interval.
In this study, we used an innovative approach based on a multiplex immunoassay to assess the performance of a panel of cytokines for the diagnosis of skin wound vitality. An immunohistochemical analysis was additionally performed as a first step in comparing the ability of biochemistry and immunohistochemistry to discriminate vital from post-mortem wounds, focusing on the marker that showed the highest sensitivity using the immunoassay.
Materials and methods
Study population
From March 1 to October 31, 2018, 24 individuals with at least one recent open skin wound and with a known survival time after wounding were included at the mortuary of the University Hospital of Montpellier. Skin wounds consisted of 16 lacerations, 4 stab wounds, and 4 gunshot wounds, mostly located on the lower limbs. The time interval between trauma and death was determined based on medical records and police reports, including testimony from witnesses. To focus on the early post-traumatic interval, the survival time had to be lower than 3 h. Bodies displaying putrefactive changes (including early signs such as discolouration of the lower abdominal wall) were excluded from the study, as well as the individuals with severe malnutrition, known immunodeficiencies, and immunotherapy.
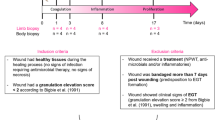
Study design
The study protocol described below was developed and validated in a previous study [20].
Pre-autopsy step
For each subject, a post-mortem incision (2 cm) was performed with a scalpel in an uninjured skin area contralateral to the ante-mortem wound, shortly after arrival at the mortuary and before refrigeration. The time elapsed between death and the infliction of the post-mortem wound was recorded. In patients with multiple ante-mortem wounds, the wound of interest was selected based on its location (no skin samples were collected from the head or hands for ethical reasons) and on its size (large wounds were preferred to small ones). Six needle-puncture sites related to resuscitation care to patients in cardiorespiratory arrest were included and considered as very early post-mortem wounds. The time interval between death and the post-mortem injury was estimated to be lower than 5 min in this subgroup.
Autopsy step
Sample collection
Skin samples from the margins of each wound (ante- and post-mortem) and from an uninjured skin area located on the midline incision line (control samples) were collected on each corpse. For biochemical analyses, 2 samples were taken from each site using a 6 mm diameter-sterile biopsy punch. Specimens were placed in sterile 1.5-mL Eppendorf® tubes after removing the hypodermis (average weight = 42.6 ± 5.3 mg) and were transferred in ice to the biochemistry laboratory, where they were immediately frozen and stored at − 80 °C until analysis. For histological examination, an additional skin sample was taken from each site and immediately placed for fixation in a 10% buffered formalin solution.
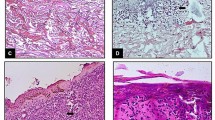
Standard histology
After formalin fixation and paraffin embedding, 5-μm sections were stained with hematoxylin and eosin and a blind histological examination of the vital and post-mortem wounds was performed. Microscopic evidence of vitality was documented, with a particular attention paid to the presence of a significant infiltration of neutrophils. Each wound was classified as “ante-mortem,” “post-mortem,” or “not classified” (NC) when its time of occurrence could not be determined with sufficient certainty (e.g., haemorrhagic infiltration with no significant inflammation).
Biochemical analyses
Protein extraction and quantification
Samples were mechanically homogenized on ice in 1.5-mL Eppendorf® tubes containing 500 μL of phosphate-buffered saline (PBS, pH 7.4), protease inhibitors (Complete Mini Roche®), and detergent (triton 0.05%), using an Ultra-Turrax® T-25 model homogenizer. The samples were centrifuged for 20 min at 15 000 g at + 4 °C, and the supernatant was aliquoted and frozen at − 80 °C until analysis. The protein content (mg/mL) of each sample was measured using the bicinchoninic acid assay (BCA, Sigma-Aldrich®).
Cytokine quantification
In each sample, the concentrations of 10 cytokines (IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, TNF-α) were simultaneously measured with a multiplex sandwich immunoassay (V-PLEX Proinflammatory Panel 1 human kit, Meso Scale Discovery®, USA), according to the manufacturer’s instructions. Briefly, 50 μL of samples was added into the wells of 96-well 10-spot plates pre-coated with specific capture antibodies immobilized on a working electrode. A solution containing detection antibodies conjugated with electrochemoluminescent labels (MSD® SULFO-TAG™) was added, before loading the plate into an instrument where a voltage was applied to the electrodes, causing the captured labels to emit light. The intensity of emitted light measured by the instrument provided a quantitative measure of each cytokine. The lower detection limits were respectively 0.20 pg/mL for IFN-γ, 0.04 pg/mL (IL-1β), 0.09 pg/mL (IL-2), 0.02 pg/mL (IL-4), 0.06 pg/mL (IL-6), 0.04 pg/mL (IL-8), 0.03 pg/mL (IL-10), 0.11 pg/mL (IL-12p70), 0.24 pg/mL (IL-13), and 0.04 pg/mL (TNF-α).
Immunohistochemistry
Paraffin 5-µm sections were immersed in a 10 mM sodium citrate buffer (pH6) for 20 min at 97 °C for dewaxing and antigen retrieval. The following primary antibody was used: IL-8 (1/500; mouse monoclonal, Santa Cruz Biotechnology). Immunohistochemistry was performed with Dako Autostainer Plus (DakoCytomation, Glostrup, Denmark) using the Flex + Envision revelation system (Dako). Appropriate positive and negative controls were used throughout the experiment.
A quantitative evaluation of staining for IL-8 was counted in 10 consecutive high-power fields (hpf) (0.237 mm2) on one representative slide per case, in the immediate vicinity of the wound margin, from the superficial dermis to the deep subcutaneous adipose tissue, taking into account all interstitial leucocytes showing stained cytoplasm, excluding intravascular cells and those within hemorrhagic areas.
Statistical analysis
Duplicate samples were randomly split into a training set and a validation set containing 72 samples each. Cytokine concentrations (pg/mL) were finally normalized on the wet weight of skin samples (g), after the following quotients were calculated and tested: cytokine concentrations/sample weight, cytokine concentrations/protein content, cytokine concentrations/sample weight/protein content. Values were expressed as a median and interquartile range, after being checked for normality using the Shapiro–Wilk test. Cytokine concentrations in vital and post-mortem wounds were expressed as the difference in their levels between wounds and controls, and they were compared in the training set using the Wilcoxon signed-rank test for paired data. At this stage, if the p value of the comparison was higher than 0.2, the cytokine was considered not relevant and was therefore not considered for the rest of the analyses.
Receiver-operating characteristic (ROC) curves were computed to evaluate the capacity of cytokines to discriminate vital wounds from post-mortem wounds.
Multivariate logistic regressions were performed in the training set to determine the combination of cytokines with the best discriminatory power. A predictive model was established and then tested on the validation set, with vital wound as the predicted condition. The variables with a p value < 0.05 after a backward selection of variables were considered statistically significant.
The sensitivity and specificity of standard histology for the diagnosis of wound vitality were calculated based on the wound categorization established after histological examination (ante-mortem, post-mortem, NC). For immunohistochemical analysis, the optimum threshold for vitality assessment was determined based on the number of interstitial IL-8 positive cells contained in ante- and post-mortem wound samples. Spearman’s rank coefficient was computed for the correlation analysis between IL-8 positivity and the biochemical concentration of the cytokine.
Statistical analysis was conducted using SAS® 9.4 software.
Results
A total of 72 duplicate skin samples were removed from the 24 cadavers enrolled in this study (20 men, 4 women, mean age = 51.0 ± 24.3 years), including 24 samples from each of the following sites: ante-mortem wounds, post-mortem wounds, and healthy skin.
The survival time after wounding ranged from a few seconds to 180 min (mean = 47 ± 53 min), while the time interval between death and the infliction of the post-mortem injury was comprised between 0 and 41 h (mean = 6.9 ± 9.0 h). Skin samples were collected after an average post-mortem interval (PMI) of 66.3 ± 28.3 h (24–117 h).
Standard histology
Histological examination allowed vital wounds to be properly diagnosed in 5/24 cases (21% of the vital wounds), and post-mortem wounds to be correctly classified as such in 19/24 cases (79%) (Table 1). The mean age of the misdiagnosed vital wounds was 47 (± 46) min. Three of them (12%) were considered by histology as post-mortem wounds, while 16 (67%) could not be classified with sufficient certainty (NC). Of the 5 misclassified post-mortem wounds, 4 were iatrogenic wounds, with one of them erroneously categorized histologically as an ante-mortem wound (Table 2). The four remaining post-mortem wounds could not be properly classified (NC).
Multiplex immunoassay
Cytokine concentrations in wounds and control samples from the training set are reported in Table 3. Median concentrations showed a high variability in each group, ranging from 3.71 (IL-10) to 1400 pg/mL (IL-8) in the vital wounds, from 1.98 (IL-4) to 223.6 pg/mL (IL-8) in the post-mortem wounds, and from 1.53 (IL-4) to 83.86 pg/mL (IL-8) in the healthy skin. After adjustment on healthy skin levels, cytokine concentrations in vital wounds were found to be significantly higher than those in post-mortem wounds, except for two cytokines (IFN-γ and IL-2) which were not considered for further analysis (Fig. 1, Table 4). IL-8 was the cytokine displaying the highest median values, reaching 1329.2 pg/mL in vital wounds and 78.27 pg/mL in post-mortem wounds (p < 0.0001). The optimum threshold values of each cytokine for the discrimination between vital and post-mortem wounds are reported in Table 5, with the corresponding sensitivities, specificities, and predictive values based on ROC analysis (Online Resource 1).
In the training set, sensitivity ranged from 38 (IL-1β, IL-12p70) to 58% (IL-4, TNF-α), and specificity from 91 (IL-10, IL-12p70) to 100% (IL-1β, IL-6, IL-8). IL-8 was the best discriminatory cytokine with a threshold value of 1203.2 pg/mL (AUC = 0.79), yielding 54% sensitivity and 100% specificity corresponding to negative and positive predictive values of 69% and 100%, respectively.
A multivariate model presented above and combining the values of IL-4 and IL-12p70 was found to be the most efficient predictive model for the diagnosis of wound vitality in the training set, with a discriminatory power higher than that of any single cytokine:
This composite model resulted in a sensitivity of 55% and a specificity of 100% (AUC = 0.84), with a threshold value of 1.17 (Table 5).
In the validation set, the ability of the cytokines and the predictive model to discriminate between vital and post-mortem wounds was slightly lower (Table 5). Among the cytokines, sensitivity ranged from 39 (IL-12p70) to 58% (IL-1β) and specificity from 78 (IL-1β) to 100% (IL-6). IL-8 remained the best discriminatory cytokine with a threshold value of 2372.7 pg/mL (AUC = 0.75), with a sensitivity of 46% and a submaximal specificity of 96%. The predictive power of the mathematical model was broadly similar to that of other cytokines (IL-1β, IL-8) in this set (AUC = 0.73), but remained highly specific (100%). Iatrogenic wounds inflicted very close to death were all correctly diagnosed by either the cytokines or the predictive model in both sets (Table 2).
Immunohistochemistry
Only 5 vital wounds were found to contain interstitial IL-8-positive cells, with a maximum of 5 positive cells per 10 hpf (mean: 0.54). No IL-8-positive cells could be found in any of the post-mortem wounds and control samples. A threshold for vitality assessment of one IL-8-positive cells per 10 hpf could therefore be defined and was reached for very short survival times of a few seconds in 2 out of the 5 positive cases. Of these 5 positive cases, 4 cases had been initially categorized as “unclassified” with standard histology. Overall, immunohistochemical staining for IL-8 sensitivity was 21% and specificity was 100%. The association of standard histology and immunohistochemistry (significant infiltrate of neutrophils and/or IL-8 positivity) allowed reaching 38% sensitivity and 96% specificity. No significant correlation was noted between the number of IL-8-positive cells and the biochemical concentration of IL-8 in the cutaneous tissue (p = 0.42).
Discussion
This study highlights how challenging can be the determination of wound vitality using standard histology in cases of injuries inflicted shortly before or after death. The sensitivity of histology was far from being optimal even when considering survival times up to 3 h, with only 21% of vital wounds correctly classified histologically. In addition, histology misclassified 5 post-mortem wounds, thus yielding a specificity of 79%. In a human model of early vital and post-mortem stab wounds [10], Gauchotte et al. found the sensitivity of inflammation to be 5% and its specificity to be 100%. This discrepancy can be partly explained by the shorter post-traumatic interval (< 45 min, with a mean of 15 min) and by the surgical model used, which may result in a reduction of the stress reaction of the body against the injuries due to anaesthesia [16, 21]. In their ex vivo model of recent post-mortem wounds (wounds inflicted to surgical specimens 5 min after devascularisation), anaesthesia and devascularisation could also have hindered a possible supravital inflammatory reaction which may have lowered the specificity of histology. In our study, one of the very early post-mortem (iatrogenic) wounds was histologically misdiagnosed as an ante-mortem injury, questioning the specificity of inflammation and the possibility of a supravital chemotaxis in such wounds [22].
In contrast to morphological methods, immunoassay methods have the advantage of being standardized and providing objective results based on the absolute quantification of proteins. In this study, we used a highly sensitive multiplex immunoassay that we previously validated in a preliminary study [20] to measure the levels of 10 cytokines in human skin wounds. Multiplex assays provide the opportunity to simultaneously quantify multiple proteins in various biological samples within a short time. They are therefore of particular interest in the field of wound vitality, as it is very likely that only a combination of several markers will eventually provide sufficient sensitivity and specificity to discriminate injuries with a short survival time from early post-mortem wounds [8].
Cytokines are a large family of cellular regulatory glycoproteins which play an active role in intercellular communication pathways, initiating the inflammatory phase by promoting the recruitment and activation of inflammatory cells [23]. As they act before the onset of leucocyte reactions at the injury site, they may represent informative diagnostic tools for the determination of wound vitality. Significantly increased levels of IL-1β, IL-6, and TNF-α were observed as early as 5 min after wounding [12,13,14, 16, 19, 24], whereas wounds with extremely short survival times did not disclose significant changes in cytokine content [16]. IL-12p70 was found to be overexpressed within 30 min after tissue injury [18], and IL-10 and IFN-γ exhibit increased levels after 60 min [17, 25]. Using RT-PCR, Ohshima et al. observed increased levels of IL-10 mRNA 10 min after wounding in mice [26]. Kondo et al. showed IL-8 to be immunohistochemically overexpressed in neutrophils 4 h after wounding [27], while overexpression of IL-13, IL-4, and IL-2 was respectively found after intervals of 1 h, 3 h, and 9 h [17, 18].
Most research work based on cytokine assessment in skin samples has focused on wound age estimation, with very limited consideration being given to the diagnosis of vitality. In addition to the investigation of early-stage vital wounds, the inclusion of those inflicted shortly after death is crucial to rule out possible supravital reactions, as such markers should present optimal specificity to be used in legal proceedings [8, 21]. To our knowledge, TNF-α is the only candidate cytokine that has been studied in post-mortem wounds, where it showed lower immunohistochemical expression levels in mast cells compared to controls and vital wounds [12].
We therefore considered cases with short survival times and with early post-mortem wounds, including a subgroup of possible supravital injuries (iatrogenic punctures from emergency care). Moreover, control skin samples were assessed in each case to take into account the inter-individual variability in the basal expression of cytokines that has been reported by several authors and confirmed in our preliminary study [13, 20, 21].
Of the 10 investigated cytokines, 8 showed significantly higher levels in vital wounds compared to post-mortem wounds, with specificity up to 100% in both the training and the validation sets. In particular, they allowed the 6 iatrogenic injuries to be correctly categorized as post-mortem wounds. These findings suggest that cytokines could represent relevant biomarkers of post-mortem wounds, including the very early of them. However, the cytokines showed low to moderate sensitivity (with a maximum of 58%), reflecting their lower ability to detect early-stage vital wounds. A multivariate model integrating the values of 2 cytokines (IL-4 and IL12p70) was found to be highly specific (Sp = 100%) in both the training and the validation sets. However, its capacity to diagnose ante-mortem injuries in the validation set was limited (Se = 43%) compared with single cytokines such as IL-1β or IL-6.
The immunohistochemical study specifically focused on IL-8 as it was found to be the cytokine with the higher ability to discriminate between vital and post-mortem wounds according to the biochemical analyses (AUC = 0.75). A weak interstitial staining of inflammatory cells for IL-8 was found in a few vital wounds (5/24), resulting in a very low sensitivity (21%). However, an immunohistochemical expression of IL-8 was shown for survival times shorter than those previously reported by Kondo et al. [27]. IL-8 was found to be a specific marker of skin wound vitality with a threshold value superior or equal to one IL-8-positive cells per 10 hpf (Sp = 100%), allowing all post-mortem wounds to be correctly classified, including iatrogenic ones. Overall, IL-8 specificity was similar using either immunohistochemical or biochemical methods, but its sensitivity proved to be significantly higher using biochemistry (46% vs. 21%).
As our protocol was based on human autopsy material, it did not allow fully controlled conditions and inevitably led to a number of limitations. First, only individuals with a precisely known ante-mortem to death interval were included. In many autopsy cases, however, this interval is unknown or insufficiently documented, which leads to the exclusion of the related cases. The strict selection criteria applied to the study population resulted in a small sample size, which prevented us from testing the results on the independence of parameters such as age, gender, anatomical site, or PMI.
Second, post-mortem wounds had to be preferably inflicted shortly after death to allow hypothetical supravital reactions to occur [8, 10, 22]. In some cases, however, the delay reached a few hours post-mortem because of the inherent constraints related to research of this kind, including the transportation time of the body to the mortuary. To address this issue, skin punctures from resuscitation care were considered very early post-mortem wounds, although their small size may have hindered the collection of representative samples for both biochemical and morphological analyses, leading to unlikely but still possible discrepancies in the results. Inconsistent results could also have stemmed from the examination of open skin wounds produced by distinct mechanisms, as the molecular profile of stab wounds may be different from that of blunt force injuries or gunshot wounds. Hence, our results need to be confirmed on better characterized and homogenized skin samples.
Finally, the biomarkers we had to deal with are present in the skin tissue under physiological conditions, with non-negligible inter- and intra-individual variability requiring internal controls from the same individual to be tested in parallel. Positive findings are based on quantitative data which are inevitably subject to margins of error and may thus be disputed in court [21]. In addition, the complexity of the methodology used can make an inter-laboratory comparison of results particularly challenging [2].
Conclusion
In this study, we used a multiplex immunoassay to quantify a panel of cytokines in human skin samples in order to assess the ability of these proteins to discriminate ante- from post-mortem skin wounds. We showed that cytokines could be relevant and helpful key markers of vitality, particularly in the very early post-traumatic interval and in the supravital period. Preliminary results also suggest that the immunoassay method used could be more sensitive than immunohistochemistry. Further research is underway to confirm these findings and to assess the interest of these markers to estimate wound age in forensic practice.
References
Grellner W, Madea B (2007) Demands on scientific studies: vitality of wounds and wound age estimation. Forensic Sci Int 165:150–154. https://doi.org/10.1016/j.forsciint.2006.05.029
Li N, Du Q, Bai R, Sun J (2020) Vitality and wound-age estimation in forensic pathology: review and future prospects. Forensic Sci Res 5:15–24. https://doi.org/10.1080/20961790.2018.1445441
Oehmichen M (2004) Vitality and time course of wounds. Forensic Sci Int 144:221–231. https://doi.org/10.1016/j.forsciint.2004.04.057
Kondo T, Ishida Y (2010) Molecular pathology of wound healing. Forensic Sci Int 203:93–98. https://doi.org/10.1016/j.forsciint.2010.07.004
Dettmeyer RB (2018) Forensic Histopathology: fundamentals and perspectives, 2nd edn. Springer, Cham
Betz P (1994) Histological and enzyme histochemical parameters for the age estimation of human skin wounds. Int J Legal Med 107:60–68. https://doi.org/10.1007/bf01225491
Guo S, DiPietro LA (2010) Factors Affecting Wound Healing. J Dent Res 89:219–229. https://doi.org/10.1177/0022034509359125
Casse J-M, Martrille L, Vignaud J-M, Gauchotte G (2016) Skin wounds vitality markers in forensic pathology: An updated review. Med Sci Law 56:128–137. https://doi.org/10.1177/0025802415590175
Hernández-Cueto C, Girela E, Sweet DJ (2000) Advances in the diagnosis of wound vitality: a review. Am J Forensic Med Pathol 21:21–31
Gauchotte G, Wissler M-P, Casse J-M et al (2013) FVIIIra, CD15, and tryptase performance in the diagnosis of skin stab wound vitality in forensic pathology. Int J Legal Med 127:957–965. https://doi.org/10.1007/s00414-013-0880-1
Dressler J, Bachmann L, Koch R, Müller E (1999) Enhanced expression of selectins in human skin wounds. Int J Legal Med 112:39–44
Bacci S, Romagnoli P, Norelli GA et al (2006) Early increase in TNF-alpha-containing mast cells in skin lesions. Int J Legal Med 120:138–142. https://doi.org/10.1007/s00414-005-0030-5
Grellner W (2002) Time-dependent immunohistochemical detection of proinflammatory cytokines (IL-1beta, IL-6, TNF-alpha) in human skin wounds. Forensic Sci Int 130:90–96
Kondo T, Ohshima T (1996) The dynamics of inflammatory cytokines in the healing process of mouse skin wound: a preliminary study for possible wound age determination. Int J Legal Med 108:231–236
Grellner W, Vieler S, Madea B (2005) Transforming growth factors (TGF-alpha and TGF-beta1) in the determination of vitality and wound age: immunohistochemical study on human skin wounds. Forensic Sci Int 153:174–180. https://doi.org/10.1016/j.forsciint.2004.08.021
Grellner W, Georg T, Wilske J (2000) Quantitative analysis of proinflammatory cytokines (IL-1beta, IL-6, TNF-alpha) in human skin wounds. Forensic Sci Int 113:251–264
Takamiya M, Fujita S, Saigusa K, Aoki Y (2008) Simultaneous detection of eight cytokines in human dermal wounds with a multiplex bead-based immunoassay for wound age estimation. Int J Legal Med 122:143–148. https://doi.org/10.1007/s00414-007-0183-5
Takamiya M, Biwasaka H, Saigusa K et al (2009) Wound age estimation by simultaneous detection of 9 cytokines in human dermal wounds with a multiplex bead-based immunoassay: an estimative method using outsourced examinations. Leg Med (Tokyo) 11:186–190. https://doi.org/10.1016/j.legalmed.2009.03.010
Birincioğlu İ, Akbaba M, Alver A et al (2016) Determination of skin wound age by using cytokines as potential markers. J Forensic Leg Med 44:14–19. https://doi.org/10.1016/j.jflm.2016.08.011
Peyron P-A, Baccino É, Nagot N et al (2017) Looking for new biomarkers of skin wound vitality with a cytokine-based multiplex assay: preliminary study. Ann Biol Clin (Paris) 75:53–60. https://doi.org/10.1684/abc.2016.1214
Cecchi R (2010) Estimating wound age: looking into the future. Int J Legal Med 124:523–536. https://doi.org/10.1007/s00414-010-0505-x
Grellner W, Madea B, Kruppenbacher JP, Dimmeler S (1996) Interleukin-1 alpha (IL-1 alpha) and N-formyl-methionyl-leucyl-phenylalanine (FMLP) as potential inducers of supravital chemotaxis. Int J Legal Med 109:130–133. https://doi.org/10.1007/BF01369672
Gonzalez AC de O, Costa TF, Andrade Z de A, Medrado ARAP (2016) Wound healing - a literature review. An Bras Dermatol 91:614–620. https://doi.org/10.1590/abd1806-4841.20164741
Bai R, Wan L, Shi M (2008) The time-dependent expressions of IL-1beta, COX-2, MCP-1 mRNA in skin wounds of rabbits. Forensic Sci Int 175:193–197. https://doi.org/10.1016/j.forsciint.2007.07.006
Zhang H, Zhu S, Qin Q (2004) Immunohistochemical and morphometrical study on the expression of interleukin-10 (IL-10) in different expressive parts during cutaneous wound healing in mice. Fa Yi Xue Za Zhi 20:70–72
Ohshima T, Sato Y (1998) Time-dependent expression of interleukin-10 (IL-10) mRNA during the early phase of skin wound healing as a possible indicator of wound vitality. Int J Legal Med 111:251–255
Kondo T, Ohshima T, Mori R et al (2002) Immunohistochemical detection of chemokines in human skin wounds and its application to wound age determination. Int J Legal Med 116:87–91. https://doi.org/10.1007/s004140100260
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with live human participants or animals performed by any of the authors. The study protocol was approved by the French Agency of Biomedicine, Nr. PFS15-003.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
414_2021_2659_MOESM1_ESM.docx
Supplementary Fig 1 ROC curves for the cytokines and the predictive score to discriminate between vital and post-mortem wounds in the training set (a) and the validation set (b) (DOCX 286 KB)
Rights and permissions
About this article
Cite this article
Peyron, PA., Colomb, S., Becas, D. et al. Cytokines as new biomarkers of skin wound vitality. Int J Legal Med 135, 2537–2545 (2021). https://doi.org/10.1007/s00414-021-02659-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-021-02659-z