Abstract
Introduction
Postmortem computed tomography (PMCT) data in gunshot-related death were evaluated by two reader groups and compared to the gold standard autopsy for the determination of forensic pathology criteria.
Materials and methods
Reader group I consisted of two board-certified radiologists whereas one board-certified radiologist and one board-certified forensic pathologist formed group II. PMCT data of 51 gunshot-related deaths were evaluated for the forensic pathology criteria number of gun shots, localization of gunshot injury, caliber, and direction of the gunshot differentiating between entry and exit wound as well as associated injury to surrounding tissue. The results of both reader groups were compared to the each other and to autopsy findings considered as gold standard.
Results
Reader groups I and II and as gold standard the autopsy evaluation showed in general a good correlation between all results. The overall discrepancy rate was 12/51 (23.4 %) cases for group I and 8/51 (15.6 %) for group II.
Discussion
Ultimately, the designated reader is able to draw the following conclusion from the presented data. At first, physical autopsy is better than PMCT regarding the localization of most gunshot injuries. Second, PMCT presents with better results than physical autopsy in locating fragmented bullets/fragment clouds, and finally, PMCT results of two radiologists were equivalent to the results of one evaluating radiologist and one pathologist with the exception of caliber assessment. However, referring to the pure numbers, the slight but not significant difference in the overall discrepancy rate of both reader groups might indicate the advantage of combining expertise in evaluating imaging in cases of gunshot-related death.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autopsy is of crucial importance for determining the cause, manner, and circumstances of death [1, 2]. Therefore, it represents the gold standard in the evaluation of nonnatural or unclear death following Recommendation No. R (99) 3 E of the Committee of Ministers to member states on the harmonization of medico-legal autopsy rules. Regarding potential projectile-related death, the forensic investigation comprises first the determination of the entry and exit of the projectile, second the projectile’s path within the body, and third the associated injury of surrounding tissue. In the past, substantial scientific effort has been undertaken to analyze the behavior of projectiles in soft tissue ballistic simulants especially using ballistic gelatin and computed tomography [3].
Very early after Conrad Roentgen had made the discovery of X-ray in 1895, first reports of pathologists using X-rays to examine the human body in firearm injuries can be found in the literature. Ever since, X-ray examinations are routinely performed before autopsy in cases of firearm injuries in the forensic medicine department to search for vital pieces of evidence [4]. In consequence, in the recent past, it has been demonstrated that postmortem computed tomography (PMCT) provides useful information when determining the cause of death, particularly in cases of gunshot injury. PMCT is meanwhile widely established in several countries all over the world—for example in Switzerland, Germany, France, Sweden, and Australia, supplementing classical autopsy as a noninvasive complement [5–7].
Especially regarding lethal ballistic wounds, PMCT presents an effective technique to localize bullets as well as to reconstruct the bullet track [6–11]. Moreover, PMCT is regarded unavoidable for analysis of lethal gunshot wounds to the head [3, 12, 13].
Although PMCT is regarded that useful, there is no study in the current literature comparing PMCT and standard autopsy of lethal gunshot injury-related deaths regarding the key issues: localization of entry and exit wound, projectile track, associated injury to the surrounding tissue, and information concerning the projectile. Moreover, it remains unclear whether PMCT data are best evaluated by radiologists or by interdisciplinary reader groups, consisting of radiologists and forensic pathologists.
Therefore, the aims of this study were first to compare PMCT findings to autopsy in cases of gunshot-related deaths for the utmost important forensic criteria and second to evaluate whether there are differences regarding the findings of radiologists and a collaborating reader group, consisting of radiologists and forensic pathologists.
Material and methods
The study was performed after approval of the local board of ethics (reference no. 151/08). All whole-body PMCT examinations with the suspicion of gunshot-related deaths in terms of either suicide or homicide were enrolled. The study was performed between October 2008 and April 2011 at our academic department of radiology.
Postmortem computed tomography
PMCT was performed in a standardized manner with the corpses lying in a supine position. All victims were kept within the body bag; they were deposited after finding on scene. A native CT scan, i.e., without administration of contrast agent was performed either on a 64-slice scanner (Brilliance 64 Philips, Amsterdam, Netherlands) or on a GE Discovery 750 HD (GE Healthcare, MA, USA). In parallel to patient whole-body exams, first a scan scout of the head and cervical spine was performed followed by the CT scan itself with axial reformats in 3.75 mm thickness. In the second step, the body scan scout was performed either in two orthogonal planes (GE Discovery 750 HD) or in only one plane (Brilliance 64). The CT scan of the thoracic and abdominal cavity including the pelvis and parts of the lower extremities up to a maximum scan length of 200 cm (GE) and 180 cm (Philips) was reformatted in 1.25-mm axial slices. Following scan procedure, PMCT data was transferred to the Picture Archiving Computer System (PACS) for storage and further evaluation.
Autopsy
Following PMCT, the corpses underwent autopsy at our academic Institute of Forensic Medicine. Autopsies were performed by forensic pathologists according to the standards of the German Government’s guidelines (§87, 89 German Code of Criminal Procedure). Only expert forensic pathologists, being at least registered, performed the autopsies. The standard autopsy in case of a lethal ballistic injury includes primarily the inspection of the entire skin looking for the entrance and exit wound, respectively, followed by the opening of all three body cavities (skull, thorax, and abdomen), and the dedicated examination of all internal organs. In the actual enrolled cases, also the direction of the gunshot was evaluated.
Data processing and image evaluation
Each PMCT data set was analyzed twice. The primary image reading was performed by two board-certified radiologists (group I). Afterwards, a second image reading was done by group II, consisting of one board-certified radiologist and one board-certified forensic pathologist. The evaluating radiologists of group I are experienced general radiologists with advanced experience of at least 1 year in forensic radiology. In contrast, the forensic pathologist (group II) is an expert in his specialty being additionally acknowledged in the field of ballistics. He additionally has an excellent experience in forensic imaging. The radiologist (group II) is an expert emergency as well as musculoskeletal radiologist, working on forensic imaging for 4 years.
All readings and analysis were performed on PACS workstations certified for image reporting.
The evaluation criteria were as follows:
-
1.
Number of gunshots
-
2.
Localization of gunshots
-
3.
Entrance vs. exit wound—gunshot direction
-
4.
Type of shot, caliber, and projectile fragments
To determine entrance and exit gunshot wound, the gunshot direction was evaluated. Four directions had to be differentiated with the centerline dividing the corpse into a right and left half:
-
1.
Right to left in transversal plane (horizontal)
-
2.
Left to right in transversal plane (horizontal)
-
3.
Anterior to posterior in sagittal plane
-
4.
Posterior to anterior in sagittal plane
In addition, the direction up–down and down–up, respectively, was taken in account as relevant regarding the gunshot direction but not considered as majorly relevant for the evaluation of the gunshot direction. After image analysis, the PMCT results of group I and group II, respectively, were compared to the findings of autopsy. In addition, the correlation of the PMCT findings of group I and group II was calculated.
Statistics
Intergroup difference regarding the total number of gunshots was assessed using the Mann–Whitney U test. The level of significance was set at p < 0.001. For analyzing interreader reliability, i.e., correlation of the reader groups to autopsy, the Cohen’s kappa test was performed. Statistical analysis was performed using Sigma Stat 3.1 software (SYSTAT Inc, Chicago, IL, USA).
Results
Overall in the time period between October 2008 and April 2011, 51 PMCTs (40 men, 11 women) meeting the inclusion criteria were enrolled. Age ranged between 14 and 89 years with a median age of 56.2 years.
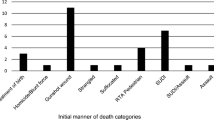
Number of gunshots
Regarding the number of gunshots, autopsy described in 43 victims one gunshot (84.3 %), in five victims two gunshots (9.8 %), in two victims three gunshots (3.9 %), and in one victim seven gunshots (1.9 %). Reader group I (radiologists) detected one gunshot in 47 PMCTs (92.2 %), two gunshots in three corpses (5.9 %), and three gunshots in one corpse (1.9 %). Group I did not recognize more than three gunshots in one victim. In contrast, reader group II (interdisciplinary) found one gunshot in 48 victims (94.1 %), two gunshots in two victims (3.9 %), and four gunshots in one victim (1.9 %, see Table 1).
Evaluating data on an injury-by-injury basis, autopsy detected in total 66 gunshots; out of these, reader groups I and II detected each a significantly lower number of only 56 gunshots (84.8 %, p < 0.001). The correlation of group I and group II was calculated with a Cohen’s kappa of 0.89. Analyzing the cases of disagreement of PMCT and autopsy, different results were found for the reader groups. Group I missed the second gunshot in three (60 %) out of five cases with two gunshots, whereas group II missed the second gunshot in four (80 %) cases. Both reader groups missed one gunshot to the knee in one victim. In another case, group I did not recognize a gunshot to the scrotum. Group II at least mentioned the scrotum as questionable pathological in this case. In the third case, both reader groups missed one out of two chest gunshots. Reader group II solely missed one out of two head gunshots. Regarding victims with three gunshots (n = 2), group I missed only in one case a single gunshot within the chest, whereas group II missed each one gunshot in both cases. In one victim, autopsy revealed seven gunshots, one located within the head–neck area and six gunshots within the trunk, majorly in the chest. Group I found three gunshots in total, the one shot described by autopsy within the head and two within the chest. In contrast, reader group II was able to detect one additional gunshot within the chest.
Localization of gunshots
Regarding evaluation of the gunshot localizations on an injury-by-injury basis, autopsy described 25 (37.9 %) gunshots to the head, 18 (27.3 %) to the mouth, 4 (6.1 %) to the mouth floor, and 19 (28.8 %) to the trunk. Group I found 29 (51.8 %) gunshots to the head, 12 (21.4 %) to the mouth, 2 (3.6 %) to the mouth floor, and 13 (23.2 %) in the trunk. Group II found 28 (50 %) gunshots to the head, 13 (23.2 %) to the mouth, 3 (5.4 %) to the mouth floor, and 12 (21.4 %) gunshots to the trunk.
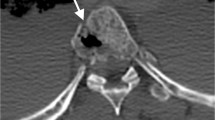
Reader group I described in several cases simply “gunshot to the head,” while the gunshots in fact have been located in the mouth or even the mouth floor (see Fig. 1). Both reader groups did not describe one gunshot to the right knee and one to the scrotal area. Moreover, both reader groups did not detect one gunshot directing through the heart and one other gunshot to the cornu superior of the thyroid cartilage.
The axial CT scans displayed in the bone window show the case of suicide by mouth floor shot. Reader group I described a gunshot to the head with the entry wound in the left temporal bone (a, see octothorpe), which was not confirmed by autopsy but a mouth floor shot directing from the mouth floor towards the left temporal region presenting with some projectile fragments within the left paraorbital region (b, see plus sign). Following the energy of the mouth floor shot, fractures of the upper and lower jaw (c see section sign) resulted. Reader group II correctly described the correct projectile path. On the axial CT image of the mouth floor (d), some gas as well as soft tissue damage is recognizable typically found in cases of mouth floor gunshots
Statistic analysis regarding the correlation of localization of gunshots of group I and group II, a Cohen’s kappa of 0.98 was calculated. The Cohen’s kappa of group I and autopsy accounted for 0.71, whereas Cohen’s kappa of group II and autopsy accounted for 0.73.
Entrance vs. exit wound—gunshot direction
In contrast to the results mentioned so far for describing gunshot direction, first of all only the number of enrolled PMCT was taken in account considering only the major gunshot in case of multiple gunshots being present.
Autopsy stated a gunshot direction right to left in 15 victims (29.4 %) and left to right in 6 victims (11.8 %). Gunshots were directed anterior to posterior in 29 victims (56.9 %) and in one single victim (1.9 %) posterior to anterior. Group I described in 17 victims (33.3 %) the gunshot direction as right to left, in 14 (27.5 %) as left to right, and in 20 victims (39.2 %) as anterior to posterior. Group II found in 21 a gunshot direction from right to left, in 7 from left to right, and in 23 an anterior to posterior direction (see Table 2). Both reader groups did not describe any gunshot direction from posterior to anterior.
For the secondary injury-by-injury-based evaluation of gunshot direction, autopsy (n = 66) revealed for 21 gunshots (31.8 %) a direction from right to left, for 8 gunshots (12.1 %) from left to right, for 36 gunshots (54.5 %) from anterior to posterior, and for 1 gunshot (1.5 %) from posterior to anterior. In contrast, group I described the direction from right to left in 23 (41.1 %) (21 correct), from left to right in 19 (33.9 %) (8 correct), from anterior to posterior in 14 (25.0 %) (14 correct), but for none from posterior to anterior (0 correct). Reader group II found the direction of 25 (44.6 %) (21 correct) gunshots from right to left, for 16 (28.6 %) (8 correct) gunshots from left to right, for 15 (26.8 %) (15 correct) gunshots from anterior to posterior, but also for no gunshot from posterior to anterior (0 correct). In summary, this leads to a misdiagnosis rate of the projectile path of 21 % for group I vs. 19 % of reader group II.
The correlation of findings regarding gunshot direction of group I and group II was calculated with a Cohen’s kappa of 0.79. The Cohen’s kappa of group I and autopsy accounted for 0.53, whereas the Cohen’s kappa of group II and autopsy accounted for 0.54.
Type of shot, caliber, and projectile fragments
Autopsy assigned from the overall 66 gunshots 9 (13.6 %) as bullet lodged in, whereas 57 (86.4 %) were perforating shots. Group I rated 19 (33.9 %) gunshots as bullet lodged in shots and 37 (66.1) as perforating shots. Group II found 21 (37.5 %) lodged in and 35 (62.5 %) perforating shots. The autopsy reconstructed 60 (90.9 %) projectiles’ calibers whereas group I described nine (13.6 %) and group II 20 (30.3 %, see Table 3).
In autopsy, 11 (19.6 %) projectiles were recognized as fragmented. As for the fragmentation of the projectiles, group I evaluated 12 (21.4 %) projectiles as fragmented whereas group II found 17 (30.4 %) fragmented projectiles. Moreover, in 10 cases, fragment clouds as well as projectile fragments were found by both groups (see Fig. 2), whereas these so-called projectile fragment clouds were not recognized in autopsy as well as singular fragments with a diameter below 7 mm (see Table 4).
The axial CT scans of the head in a bone window show a rather large metal isodense foreign body (a, red circle) in terms of a projectile fragment which had not been detected by autopsy but on PMCT. The “normal” brain window in axial (b) presents severe streak artifacts surrounding the bullet fragment limiting the evaluation of the surrounding tissue for bleeding, etc. However, a three-dimensional volume rendering technique in a view from superior (c) allows for a detailed evaluation of the location and character of such metal fragments (see red circle)
Furthermore, a foreign body within the right main bronchus which turned out to be a bone fragment and a fracture of the arcus zygomaticus were only found by the PMCT groups.
Group I (radiologists) vs. group II (interdisciplinary) vs. autopsy
In comparing the results of group I to the gold standard in 12 of the overall 51 evaluated PMCTs, disagreements (23.4 %) were found. In five cases, the gunshot direction was the cause for these discrepancies mostly misjudging entry versus exit wound and consequently resulting in a wrong channel direction mostly from right to left and vice versa. In another two cases, the description of the gunshot wound location was wrong in terms of one case of a mouth gunshot and one case of a gunshot through the mouth floor, both being described as simple cases of head gunshots by group I. The comparison of reader group II results’ to autopsy revealed discrepancies in only 8 of the overall evaluated 51 PMCTs (15.6 %). In one case, a disagreement of both readers regarding the gunshot direction was present. In another case, the gunshot entrance wound was wrongly described as compared to autopsy in terms of localizing the entrance in the mouth and not at the mouth floor. In a third case, entrance and exit wound were inverted.
Discussion
The presented study compares for the first time the results of two reader groups interpreting PMCT data of gunshot-related death to the gold standard autopsy to find the advantages and disadvantages of PMCT in cases of projectile-related death. The overall discrepancy rate based on a case-by-case evaluation of both reader groups was found to be equivalently low for all four evaluation criteria. Regarding the first evaluation criterion in terms of number of gunshots, both groups detected significantly lower numbers compared to the gold standard especially in cases of multiple gunshots found in autopsy. However, calculating the interreader reliability in terms of correlation between both groups revealed an almost perfect consensus performing the Cohen’s kappa test.
For the second evaluation criterion in terms of localization of gunshots, an even better correlation of both reader groups resulted for the Cohen’s kappa test in terms of an almost perfect correlation, whereas the correlation between both groups and autopsy was lower but still reaching considerable consensus. Regarding the evaluation of the entrance versus exit wound and the projectile track, respectively, also a considerably high correlation resulted whereas the correlation between groups I and II and autopsy was only considered as moderate consensus. In summary, for all four criteria, a by trend higher correlation to the gold standard resulted for group II evaluating PMCT data in an interdisciplinary approach.
One of the most common discrepancies was the description of wrong gunshot directions and accordingly the confusion of entry and exit wounds (see Fig. 1). In the current literature, a number of studies comparing PMCT and autopsy findings in gunshot-related death exist, but none of them features the experimental setup of the presented study.
In this context, Makhlouf et al. compared gunshot-related PMCT findings to autopsy, whereas the PMCT data were interpreted by one radiologist without any specific forensic training stated as limitation of the study [8]. Furthermore, Jacobsen et al. compared PMCT data to autopsy findings whereas the CT data were interpreted by one physician with 13 years experience in forensic pathology but no experience in reading postmortem CT, so that the missing radiologic expertise was described as a study limitation [14]. To evaluate possible advantages and disadvantages, respectively, of PMCT in the analysis of projectile-related death, the dedicated setting of the presented study in terms of two reader groups consisting of two board-certified radiologists and of one board-certified radiologist and one forensic pathologist, respectively, reading the PMCT data was chosen and the results compared to the considered gold standard in terms of autopsy to overcome the limitations of the just mentioned studies [8, 14].
The criteria being elaborated by both reader groups were considered to be comprehensible on PMCT [5, 6, 13]. In the presented study, the comparability between both reader groups was the main goal. Since both reader groups evaluated the same cases, had the same information on the cases, and performed even the same types of mistake regarding the evaluated criteria in identical cases, comparability is given. Thus, direct comparison and evaluation of the reader groups’ results were provided.
As inclusion criterion, the performance of PMCT in cases of suspected projectile injury-related death in terms of homicide or suicide was set. General exclusion criteria were missing documentation in one or both reader groups and the use of other weapons besides firearms. Consequently, six cases were excluded because of missing data. The decision on which CT scanner PMCT was performed at was made due to availability at our University Radiology Department. The PMCT examinations were performed with the corpses laying in body bags as found on scene to overcome hygienic, ethical, and legal reasons [5, 6].
The general trend of the presented results showed a good correlation taking the results of both reader groups compared to the autopsy as gold standard in consideration. Discrepancies made by both groups were identical in five cases. In two cases, the discrepancy was caused by describing a wrong number of gunshots in the same body cavity. In one, case both reader groups evaluated one gunshot in the trunk whereas autopsy described three gunshots. For the other case, the PMCT evaluation revealed three and four gunshots, respectively, evaluated by reader groups I and II, whereas the autopsy described seven gunshots with one located within the head–neck area and six of them located in the trunk majorly within the chest. These findings are in context with the work of Makhlouf et al. who stated that the differentiation of single bullet tracks on PMCT gets difficult when more than one shot in the same body cavity is present [8].
However, as a typical limitation of PMCT, the poor soft tissue differentiation between organs and vascular structures due to the lack of intravenous contrast agent should be mentioned. Therefore, vascular injury often remains undetected, unfortunately often leading to the result of overlooked gunshot injuries especially in cases of perforating gunshots. But the collection of gas or the presence of hematoma along a wound track allows for the prediction of vascular injury. In this context, the performance of postmortem CT angiography might increase the results of PMCT in detecting vascular injury and integrity, respectively [2, 15]. The use of intravenous contrast agent for postmortem CT is focus of an ongoing study of our study group, and the initial results especially regarding a better evaluation of multiple gunshot injuries is promising.
Another limitation of PMCT to be mentioned is that wounds which are easily visible during gross inspection may be subtle or not visible/detectable at all on PMCT because the characteristics of the entry and exit wounds may change due to extrinsic pressure from adjacent body parts, clothes, and dependent postmortem positioning. Also, the supine position chosen for the PMCT examination may lead to interpretation problems of especially the bullet track since the bullet track is related to the victim’s position at the time of the deadly injury. Post- and or perimortem pneumothorax or hemorrhage may result in a significant shift of especially the lung, mediastinum, and heart, thus might be crucial when interpreting PMCT data.
Interestingly, when comparing autopsy and PMCT findings, both reader groups described projectile fragments or fragment clouds on PMCT, which were not referred to in the autopsy report. However, this is in context with the current literature where several authors note this fact as a distinct advantage of PMCT in the ballistic analysis [6, 12, 16]. As it is common knowledge, such bullet fragments have been and still are detected in many institutions using conventional radiography. However, in this context, not only detecting such bullet fragments as it is possible using radiography but also defining its exact location and three-dimensional display of the fragments are the great advantages of PMCT along with the evaluation of damage to the surrounding tissue, which will also be improved if iv contrast agent will be routinely used for postmortem CT imaging.
In correlating the evaluation results of groups I and II performing the Cohen’s kappa test, a near perfect conformity between the two reader groups on each of the defined evaluation criterion resulted. Yet, the only aspect of the study when reader group II presented with better results compared to group I is in the assessment of bullet caliber on PMCT. In every other regard, the performance of group I and group II is nearly identical. In the assessment of bullet caliber, the expertise in forensic pathology is crucial, and even in forensic imaging, trained radiologists have by far significantly worse skills.
Therefore, the potential expectation in our study that an interdisciplinary reader team is supposed to reveal superior results clearly cannot be supported by our results. In contrast, interdisciplinarity seems not to be of distinct impact to the reading result. However, a discrete trend was recognizable regarding slight superior evaluation results of PMCT data if the expertise of radiology and forensic pathology is combined.
Considering the current literature, in general, the experience of the radiologist with the interpretation of PMCT data seems to be a crucial point and is of utmost importance especially regarding the ballistic forensic analysis [16]. Vice versa, a profound training of forensic pathologists evaluating PMCT data is vital [14]. However, up to date, there exists no worldwide standard of how PMCT should be performed and interpreted [17]. Also, in this context, a standardized training in forensic radiology for both medical fields is in discussion in the respective associations right now planning on the introduction of a specialized training of both the radiologist as well as the forensic pathologist [18].
Though, a number of questions are raised by the current study. First, we did not evaluate a third reader group consisting only of forensic pathologists so that no final answer to the question which medical specialization in terms of radiology and forensic pathology plays the more important role in reference to the actual problem.
Second, our results seem to support the hypothesis that, a two-reader system as a measure of quality control might ensure accuracy. This fact may also explain the close conformity in the presented results between the two reader groups. However, this issue has to be addressed in an upcoming study evaluating the performance of single readers, radiologists, as well as forensic pathologists.
Conclusion
In conclusion, the actual presented comparison of two reader groups evaluating PMCT data in cases of projectile-related death shows that if the essential concepts of analysis of projectile trajectory and track are applied to PMCT data, it allows for a certain characterization of penetrating and perforating gunshot-related injuries. In summary, PMCT presents for a noninvasive imaging technique with certain potential to improve autopsy results still considered as the gold standard. However, evaluation of PMCT can also result in some confusion of the autopsy reports if medical professionals of either specialty do it without any specific experience regarding either side in terms of forensic radiology and medicine, respectively. Regarding the presented data, one can draw the conclusion that first of all physical autopsy is better than PMCT regarding the localization of most gunshot injuries. Second of all, PMCT is performing better in locating fragmented bullets and/or fragment clouds and allows for additional evaluation of damage to the surrounding tissue, e.g., intracranial bleeding and pneumothorax. Third of all, PMCT results of two evaluating radiologists were equivalent to the evaluation results of an interdisciplinary reader team consisting of one radiologist and one forensic pathologist with one exception regarding the assessment of the projectiles’ caliber. In the assessment of bullet caliber, the expertise in forensic pathology is crucial, and even in forensic imaging, trained radiologists have by far significantly worse skills.
References
Brogdon B (1998) Forensic radiology. CRC Press, Boca Raton
DiMaio VJ (2002) Gunshot wounds: practical aspects of firearms, ballistics, and forensic techniques. CRC press
Korac Z, Kelenc D, Baskot A, Mikulic D, Hancevic J (2001) Substitute ellipse of the permanent cavity in gelatin blocks and debridement of gunshot wounds. Mil Med 166(8):689–694
Thali MJ, Viner MD, Brogdon BG (2010) Brogdon’s forensic radiology. CRC Press
Andenmatten MA, Thali MJ, Kneubuehl BP, Oesterhelweg L, Ross S, Spendlove D, Bolliger SA (2008) Gunshot injuries detected by post-mortem multislice computed tomography (MSCT): a feasibility study. Legal Med (Tokyo, Japan) 10(6):287–292. doi:10.1016/j.legalmed.2008.03.005
Thali MJ, Yen K, Vock P, Ozdoba C, Kneubuehl BP, Sonnenschein M, Dirnhofer R (2003) Image-guided virtual autopsy findings of gunshot victims performed with multi-slice computed tomography and magnetic resonance imaging and subsequent correlation between radiology and autopsy findings. Forensic Sci Int 138(1-3):8–16
Harcke HT, Levy AD, Getz JM, Robinson SR (2008) MDCT analysis of projectile injury in forensic investigation. AJR Am J Roentgenol 190(2):W106–W111. doi:10.2214/ajr.07.2754
Makhlouf F, Scolan V, Ferretti G, Stahl C, Paysant F (2013) Gunshot fatalities: correlation between post-mortem multi-slice computed tomography and autopsy findings: a 30-months retrospective study. Legal Med (Tokyo, Japan) 15(3):145–148. doi:10.1016/j.legalmed.2012.11.002
Thomsen AH, Jurik AG, Uhrenholt L, Vesterby A (2009) An alternative approach to computerized tomography (CT) in forensic pathology. Forensic Sci Int 183(1-3):87–90. doi:10.1016/j.forsciint.2008.10.019
Thali MJ, Jackowski C, Oesterhelweg L, Ross SG, Dirnhofer R (2007) VIRTOPSY—the Swiss virtual autopsy approach. Legal Med (Tokyo, Japan) 9(2):100–104. doi:10.1016/j.legalmed.2006.11.011
Poulsen K, Simonsen J (2007) Computed tomography as routine in connection with medico-legal autopsies. Forensic Sci Int 171(2-3):190–197. doi:10.1016/j.forsciint.2006.05.041
Oehmichen M, Meissner C, Konig HG, Gehl HB (2004) Gunshot injuries to the head and brain caused by low-velocity handguns and rifles. A review. Forensic Sci Int 146(2-3):111–120. doi:10.1016/j.forsciint.2004.06.023
Thali MJ, Kneubuehl B, Vock P, Allmen G, Dirnhofer R (2002) High-speed documented experimental gunshot to a skull-brain model and radiologic virtual autopsy. Am J Forensic Med Pathol 23(3):223–228. doi:10.1097/01.paf.0000023002.14999.5e
Jacobsen C, Lynnerup N (2010) Craniocerebral trauma—congruence between post-mortem computed tomography diagnoses and autopsy results: a 2-year retrospective study. Forensic Sci Int 194(1-3):9–14. doi:10.1016/j.forsciint.2009.10.001
Grabherr S, Djonov V, Yen K, Thali MJ, Dirnhofer R (2007) Postmortem angiography: review of former and current methods. AJR Am J Roentgenol 188(3):832–838. doi:10.2214/ajr.06.0787
Filograna L, Tartaglione T, Filograna E, Cittadini F, Oliva A, Pascali VL (2010) Computed tomography (CT) virtual autopsy and classical autopsy discrepancies: radiologist’s error or a demonstration of post-mortem multi-detector computed tomography (MDCT) limitation? Forensic Sci Int 195(1-3):e13–e17. doi:10.1016/j.forsciint.2009.11.001
Bedford PJ, Oesterhelweg L (2013) Different conditions and strategies to utilize forensic radiology in the cities of Melbourne, Australia and Berlin, Germany. Forensic Sci Med Pathol 9(3):321–326. doi:10.1007/s12024-013-9424-8
Rutty GN, Gorincour G, Thali M (2013) Post-mortem cross-sectional imaging: are we running before we can walk? Forensic Sci Med Pathol 9(3):466. doi:10.1007/s12024-013-9464-0
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kirchhoff, S.M., Scaparra, E.F., Grimm, J. et al. Postmortem computed tomography (PMCT) and autopsy in deadly gunshot wounds—a comparative study. Int J Legal Med 130, 819–826 (2016). https://doi.org/10.1007/s00414-015-1225-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-015-1225-z