Abstract
The clavicle is the first bone to ossify in the developing embryo and the last to complete epiphyseal union. It is the latter sustained period of growth that has attracted the interest of skeletal biologists and forensic practitioners alike, who collectively recognize the important opportunity this bone affords to estimate skeletal age across the prenatal to early adult lifespan. Current research is largely directed towards evaluating the applicability of assessing fusion in the medial epiphysis, specifically for determining age of majority in the living. This study aims to contribute further insights, and inform medicolegal practice, by evaluating the Schmeling five-stage system for the assessment of clavicular development in a Western Australian population. We retrospectively evaluated high-resolution multiple detector computed tomography (MDCT) scans of 388 individuals (210 male; 178 female) between 10 and 35 years of age. Scans are viewed in axial and multiplanar reconstructed (MPR) images using OsiriX®. Fusion status is scored according to a five-stage system. Transition analysis is used to calculate age ranges and determine the mean age for transition between an unfused, fusing and fused status. The maximum likelihood estimates (in years) for transition from unfused to fusing is 20.60 (male) and 19.19 (female); transition from fusing to complete fusion is 21.92 (male) and 21.47 (female). Results of the present study confirm the reliability of the assessed method and demonstrate remarkable consistency to data reported for other global populations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The specialist assistance of a forensic anthropologist is often necessary in circumstances where the age-at-death of a decedent is unknown or in question. The material referred for investigation will vary from an isolated dry bone or complete skeleton, through to medical images from a living individual, with the latter more commonly encountered in jurisdictions where there are high rates of illegal border crossings and age of majority is at issue (see below). For the anthropologist attached to a forensic morgue, there will also be circumstances requiring removal of body parts diagnostic of age in unidentified fully fleshed individuals, so that an estimated age-at-death can be entered into associated coronial records, alongside visual identifiers of sex (e.g. external genitalia) and ancestry that are already recorded at autopsy.
In the adult skeleton, the pubic symphysis, sternal rib ends and medial clavicle are commonly evaluated towards facilitating an estimation of skeletal age [1]. This typically involves the subjective assessment of morphoscopic traits relative to statistically documented age-stages (e.g. [2–4] and see below for specific reference to the clavicle). It is generally accepted that the assessment of multiple skeletal indicators facilitates greater confidence in the final age estimation largely because it helps to control for intraspecific variation in any single attribute studied (see [5] for more detailed considerations of multifactorial age assessment). With regard to principles of best practice, the Scientific Working Group for Forensic Anthropology (SWGANTH) also recommend, “Whenever possible, standards for age assessment should be used that are most appropriate for the ancestry/population origin of the remains examined” [5]. That group also highlights the importance of quantifying intra- and inter-observer error rates. In regard to criteria pertaining to age estimation in living individuals, the Study Group on Forensic Age Diagnostics (AGFAD) similarly stresses the importance of reference studies utilizing representative population samples, in addition to advocating specific methodological approaches designed to increase diagnostic accuracy [6, 7]. The latter group also considers, within a medicolegal context, the appropriate preparation of expert reports and requirements for ongoing quality assurance through annual proficiency testing.
Cognizant of the above recommendations, the present study focuses on the morphoscopic assessment of the clavicle—a bone that has demonstrated potential for age assessment in a variety of medicolegal contexts [8–14]. The clavicle is a long bone that articulates with the manubrium medially (sternoclavicular joint) and the acromion process of the scapula laterally (acromioclavicular joint); functionally, it provides a framework for muscle attachment and facilitates stability and movement in the shoulder joint [15, 16]. The clavicle has a relatively complex and atypical developmental sequence relative to other bones in the human skeleton; it is the first to ossify in the developing embryo, and it is the last to complete epiphyseal union [17, 18]. The primary ossification centres appear at approximately 5–6 weeks of gestation, and fusion of the medial epiphysis generally occurs in the second to early third decade of life [16]. The sustained period of growth-related clavicular metamorphosis is of particular interest to skeletal biologists and forensic practitioners alike, because assessment and quantification of the latter affords a unique opportunity to use this bone to estimate skeletal age across the prenatal, juvenile, adolescent and early adult lifespan.
The nonmolecular anthropological approaches applied for estimating skeletal age in the clavicle fall into two broad methodological categories: morphometric—measurements of diaphyseal length [19] or morphoscopic—stage assignation of ossification and/or fusion status relative to full maturity [8]. The assessment of the medial clavicle is one such example of the latter method, albeit not necessarily performed to estimate a specific skeletal age per se, but rather to determine whether an individual (e.g. nonnationals without valid identification documents) has reached a specific threshold age of legal responsibility. The age of criminal liability varies across jurisdictions, but it typically lies between 16 and 22 years [9]. Establishing the age of majority is especially important in criminal proceedings where minors have special protection as victims and/or perpetrators of criminal activities; the consequences of minors being incarcerated in an adult correctional facility and vice versa is of serious concern and one that was recently highlighted in an inquiry held by the Australian Human Rights Commission [20].
The deep research interest in the age-related developmental progression of the medial clavicle is firmly entrenched in a large repository of published literature, with a rapid increase in research output over the last two decades coinciding with both the availability of, and technological improvements in, medical imaging. A further driving force of such research is documented population variation in skeletal growth and development, which means that there is no single globally representative ‘forensic standard’ available for age assessment using the medial clavicle; to that end, the literature is abound with empirical research investigating the forensic utility of this bone in a variety of global populations [e.g.10–14]. Although clear intra- and inter-population variation in the timing of skeletal maturity has been demonstrated, there is a growing awareness that socioeconomic conditions are most likely a stronger influence on growth, compared to variation in inherited genetic markers related to ancestral origin [21, 22]. The relative importance of the developmental ‘socioeconomic environment’ is thus inherently related to the demonstrated plasticity of human growth in relation to external stimuli, whether physical or even psychosocial [23–26]. The latter mandates statistically quantitative research specifically tailored towards ensuring not only methodological soundness (see above) but also the concurrent formulation of population-specific age estimation standards.
The primary objective of the present study is to statistically quantify ossification and fusion timing in the medial clavicle epiphysis as visualized in high-resolution multislice CT scans. The specific aims, in the context of forensic practice, are as follow: (i) to quantify intra- and interobserver accordance of the five-stage medial clavicular epiphysis system of Schmeling et al. [8]; (ii) to develop sex-specific age-at-transition standards and determine the upper and lower developmental age boundaries for this structure in a contemporary Western Australian population; and (iii) to evaluate these data in relation to comparable published research in contemporary Australian and other global populations.
Materials and methods
Materials
The present study involves the retrospective analysis of 388 patients, representing 210 male and 178 female individuals between 10 and 35 years of age. The sample comprises individuals who presented for clinical thoracic evaluation in the Western Australian hospital system between 2006 and 2013; 80 % of those patients were admitted between 2010 and 2013. The symptoms most frequently requiring clinical referral relate to trauma, tumours of various aetiology and vascular disease. Each individual scan was screened prior to analysis, and those presenting obvious abnormal morphologies were accordingly removed; exclusions were most commonly made on the basis of anatomical shape variants associated with the medial end (e.g. ‘bowl-like’ or ‘fish-mouth-like’ variants) that, according to Wittschieber et al. [27], preclude assessment according to the Schmeling [8] five-stage system because…“it is uncertain whether such variants are associated with the same correlations between developmental speed and morphological appearance [27: p.187]”. The sample after exclusion of unsuitable scans comprised 333 individuals in total, of which 185 are male and 148 female (Fig. 1). It is also important to note that an inherent limitation of using patient data is the possible influence of development retardation (e.g. due to tumour involvement or genetic disorders), although in the context of medicolegal age estimation, this would not have negative consequences for the individual referred for examination.
Following the relevant Australian legislation for research involving human subjects and/or their biological data (National Statement on Ethical Conduct in Human Research [28]), all information regarding patient identity was removed prior to receipt by the senior author; the only data retained is patient age and biological sex. As is commonplace for most medical imaging modalities requested specifically for clinical evaluation, there is no record of patient ancestry, as such data are deemed medically irrelevant. It is thus only possible to suggest that the sample examined here is generally expected to be representative of the overall Western Australian population, which according to the latest census data is predominantly Caucasian in origin [29].
Methods
Computed tomography data
Thoracic patient medical imaging was performed using multiple detector computed tomography (MDCT) on a Philips Brilliance 64 scanner (Philips Healthcare, North Ryde, Australia). Image resolution is an important consideration because greater ambiguity in assessing developmental morphologies can be introduced in low-resolution (thick-slice) MDCT scans [11, 30]. The present study thus analyses high-resolution scans with an average beam width of 1 mm (range, 0.625–2.00 mm; 75 % of samples ≤1 mm) and images reconstructed to the same slice thickness. The MDCT scans are viewed in axial and multiplanar reconstructed (MPR) images using OsiriX® (version 3.9–64 bit).
Assessment of ossification status
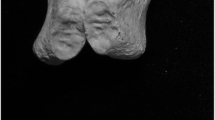
The fusion status of the medial clavicle is assessed following the five-stage scoring system developed by Schmeling et al. [8]. In Fig. 2, five individuals (12–29 years of age) are presented as exemplars for each successive ossification stage; definitions of the features used to describe ossification status in each stage are outlined in Table 1.
Stages 1 to 5 of clavicular ossification as visualized by MDCT in the coronal plane. See Table 1 for associated descriptions of each stage. Note: data is cross-sectional whereby the associated images at each age represent a single individual
Statistical analyses
-
(i)
Observer error and bilateral variation
All evaluations are made by both authors, and the repeatability of the five-stage scoring system was statistically quantified prior to primary data collection. Intra-observer error in clavicular epiphyseal stage assignation is evaluated based on the repeat assessment of 50 individuals, with a 4-week interval left between re-evaluation; the magnitude of inter-observer error is determined based on the scores assigned by each examiner. The Kappa statistic is used to provide a quantitative measure of the magnitude of agreement within and between observers [31, 32]. Bilateral assessment of clavicular fusion status is recorded, and the statistical significance of any developmental differences in stage assignation is explored using the Wilcoxon signed-rank test [33]. In accordance with previous research [e.g. 11, 34] for those individuals presenting any disparity between scores assigned to the left and right sides, the more developmentally advanced side is used to quantify the degree of ossification.
-
(ii)
Modelling ossification status
Descriptive statistics calculated include mean age, 95 % confidence intervals, standard deviations, range and percentiles for stage of clavicular fusion. Spearman rank correlations are used to examine the relationship between chronological age and fusion stage according to sex. It is acknowledged that the latter descriptives can be relatively sensitive to outliers and other sampling biases (e.g. broad age ranges) and thus represent a basic (albeit judicially admissible) means of data summation. To that end, the present study also uses transition analysis to calculate age ranges for each of the defined clavicular stages [14]. Transition analysis represents a parametric modelling method suitable for application to small samples and is designed for the analysis of skeletal trait(s) that can be arranged into an invariant series of senescent stages [36]. This method is thus used as a basis for inferring the timing of unidirectional transitions between the successive clavicular ossification stages. Transition analysis uses a log-age cumulative probit model to calculate the mean and standard error of the age of transition between the developmental phases [36, 37].
The relevance of this method for age differentiation in legal proceedings continues to be explored in the literature. Lucy [38] provides a detailed exploration of the suitability of Bayesian approaches to answer questions of evidence and discusses issues surrounding the necessity of specifying a prior age-at-death distribution. Konigsberg et al. [39] also explored the latter issue in the context of evidentiary requirements and demonstrated that the application of appropriate explicit prior age-at-death prior distributions facilitates statistically robust models. In the present study, the transition analyses are performed using the Nphases2 programme (http://konig.la.utk.edu/nphases2.htm)—see Boldsen et al. [35] and Kimmerle et al. [36] for a more detailed discussion of the statistical basis of this method and [14, 40] for practical applications.
Results
Observer error and bilateral variation
In the assessment of practitioner repeatability of the five-stage medial clavicular development method of Schmeling et al. [8], the levels of intra-observer accordance based on the repeat assessment of 50 individuals are: DF ϰ = 0.915 (3/50 non-agreements); AF ϰ = 0.945 (2/50 non-agreements) (Table 2). The level of inter-observer agreement is ϰ = 0.889 (4/50 non-agreements—all between stages 4 and 5) (Table 2). In the evaluation of both intra- and inter-observer accordance, there were no repeat assessments that differed by more than one stage. Those Kappa values, according to the criteria outlined by Landis and Koch [33], indicate an ‘almost perfect’ agreement. The Wilcoxon signed-rank test indicated that developmental differences between the right and left clavicles were statistically nonsignificant (z = −0.186; P = 0.853), a total of 27/332 (8 %) of individuals had a one-stage discrepancy between the left and right sides, with no individual having a variation of more than one stage.
Ossification status
Spearman rank correlations indicate a significant positive relationship between age and stage of clavicular development in both sexes: male r s = 0.920; sig = P < 0.0001, female r s = 0.934; sig = P < 0.0001. Summary data and distribution frequencies for age of clavicular fusion are presented in Tables 3 and 4 and Fig. 3, respectively. It is important to note that the descriptive statistics for the first and last stages are inherently dependent on the lower and upper age boundaries of the sample; accordingly, the mean ages for stages 1 and 5 may not be a true reflection of associated population variability [14]. It is evident that the youngest age of complete fusion of the epiphysis (stage 4) is 21 and 20 years of age in males and females, respectively; for males, this represents 1.6 % of individuals assessed as stage 4, whereas for females, it is 2.2 %. Evidence of an epiphyseal scar (remnant) was present in individuals beyond 30 years of age in both sexes (Tables 3 and 4). The youngest age for obliteration of the epiphyseal scar (stage 5) is 24 and 25 years of age in males and females, respectively. The latest age of non-fusion (≤stage 2) is 22 and 21 years in males and females, respectively; this accounts for 2.9 % of males and 3.6 % of female individuals assessed as stage 2.
Transition analysis
Using the five successive clavicular fusion stages of Schmeling et al. [8], a total of four transition stages are modelled. Descriptive statistics for the age of transition between the successive stages are shown in Table 5; probability density plots for male and female transition distributions are presented in Figs. 4 and 5, respectively. It is evident that the transition to complete fusion (stages 3 to 4) occurs at 22.24 and 21.38 years of age in males and females, respectively. Following our previous approach [40] based on the method described by Shirley and Jantz [37], ‘unfused’, ‘fusing’ and ‘fused’ age limits are derived from the upper and lower bounds of stage transition distribution using ±1 and ±2 standard deviations, representing 68 and 95 % of the prediction intervals, respectively. The unfused age limit is based on the upper age boundary of stages 1 and 2, the fused age limit is based on the lower age boundary of stages 4 and 5. The latter represents the oldest age at which an individual is likely to present non-fusion, and the former, the youngest age of complete fusion of the medial clavicular epiphysis. The fusing age limits are based on the stages 3–4 transition distributions and represents the youngest probable age of initial clavicular fusion (Tables 5 and 6).
Discussion
Statistical quantification of the time frame for the ossification of the medial clavicle has direct relevance to medicolegal investigations requiring a noninvasive estimation of age in living individuals (supplemented by results of other assessments—e.g., physical examination and dental evaluation [6]). Such data are particularly important in Europe, where research is driven by the growing need for forensic age assessments in European immigrants from non-European Union countries [11], which between 2012 and 13 represented approximately 13,000 individuals [41]. The fusion status of the medial clavicle also has practical application in the assessment of dry skeletal material referred to a forensic anthropologist, facilitating a relatively narrow age estimate in nonskeletally mature individuals, through to a minimum age threshold in individuals where growth is complete. The aims of the present study were to evaluate the robustness of the Schmeling et al. [8] five-stage system for quantifying fusion status in the medial clavicle in a modern Western Australian population, generate developmental age boundaries for this structure, and to interpret that data in the broader context of previous national and international research.
Observer error and bilateral asymmetry
Statistical testing of observer accordance indicates that the assessment of clavicular fusion following the five-stage system of Schmeling et al. [8] is reproducible, both within and between examiners (Table 2). Intra-observer accordance was high for each examiner (ϰ ≥ 0.900), with a slight decrease in interobserver accordance between the two same individuals (ϰ = 0.889). Following the nomenclature used to describe the relative strength of agreement associated with Kappa statistics, Landis and Koch [32] suggest that the latter results indicate an almost perfect agreement. The levels of observer agreement reported in the present study are mostly comparable to, albeit in some cases considerably higher than, previous studies examining the same developmental attribute (e.g. Cameriere et al. [11]; Bassed et al. [13]; Schulze et al. [42] and Hillewig et al. [43]). The relatively higher levels of observer accordance (especially interobserver) in the present study are likely related to high levels of examiner experience (see below) combined with the use of thin-slice MDCT scans (75 % of the sample ≤1 mm); see also Wittschieber et al. [27] and Mühler et al. [30] for further discussion of the influence of slice thickness in the assessment of the medial clavicular epiphysis.
It is largely accepted that the accurate assessment of subjective morphological skeletal attributes relies on experience in both appropriate method application and knowledge of anatomical variants [27, 44, 45]. With specific reference to the morphological development of the medial clavicle, the effect of examiner experience in the determination of ossification stage was explored by Wittschieber et al. [27]. Based on the repeat assessment of the medial clavicular epiphysis visualized in thin-slice MDCT scans, it was demonstrated that examiner experience has a “…strong influence on stage assessment” [27; p. 189]. These authors also warn that Cohen’s Kappa statistic should be critically evaluated in relation to examiner experience and qualification; in other words, Kappa values directly depend on examiner experience, and thus, comparisons between examiners of differential experience levels are not necessarily objective [27]. In the present study, both observers (DF and AF) are equally experienced in the assessment of such biological structures, and thus, their respective Kappa statistics can be directly compared.
There is empirical evidence demonstrating slightly higher intra- and interobserver accordance using three- [14] and four-stage [43] systems for assessing clavicular fusion. In the latter study, a perceived ambiguity in discerning the presence of a physeal scar is effectively removed by merging Schmeling’s tages 4 and 5, whereby the last stage is defined as “…complete union of the ossified epiphysis with the clavicular metaphysis” [47; p. 1117]. The Fleiss Kappa values (average for left and right sides) for the Schmeling (five-stage) and Kreitner (four-stage) systems are 0.705 and 0.750, respectively [43]. It is important to note that direct comparison of observer accordance values in Hillewig et al. [43] to the present study must be cognizant of potential variation introduced due to different imaging modalities—the former utilizing magnetic resonance imaging (MRI) and the latter, high-resolution MDCT. Irrespective, observer accordance within the present study is demonstrably high in applying a five-stage system; this importantly, provides confidence in the derived statistical models.
The present study did not find any evidence of statistically significant bilateral developmental asymmetry in the fusion timing of the medial clavicular epiphysis. A total of 27 individuals (8 % of the total sample) had a one-stage discrepancy between the left and right sides. In examining the latter within the context of select previous research in different global populations, it is evident that rates of bilateral asymmetry in this particular developmental attribute vary widely irrespective of the imaging modality and scoring system applied, ranging between 1.6 and 20.1 % (Table 7). Bilateral variation exceeding more than one developmental stage was not observed in the present study. In those comparative studies that do provide data specific to the level of bilateral divergence, it appears extremely rare that it exceeded one developmental stage, with the three-stage discrepancy reported by Bassed et al. [13] being somewhat unusual (albeit likely attributable to the methodological approach employed—see below). The point of commonality between all of the studies listed in Table 7, however, is that the rate of developmental asymmetry observed was not statistically significant in each instance.
Ossification status
There are many studies in the published literature statistically quantifying the timeframe for ossification of the medial clavicular epiphysis. To facilitate a simple comparison to the present study, a selection of relevant findings of previous research is summarized in Table 8. To avoid potential sampling bias (see above), latest age limits are provided for stage 1 and the earliest age limits for stages 4 and 5. In the present study, it was observed that females are developmentally more advanced than males across stages 1 to 4 (range 0.50 to 1.75 years—Table 3); this same relative relationship is evident in the age at transition statistics (range 0.86 to 1.47 years—Table 5). The same relationship is also apparent in the comparative populations, whereby female individuals are generally more developmentally advanced than their male counterparts, albeit the differences are relatively small (Table 8).
In the Western Australian sample, the oldest age at which stage 1 persists was 17 and 16 years of age in males and females, respectively. Morphologically, this stage represents the absence of the rudimentary and ‘flake-like’ medial epiphysis (secondary ossification centre) that usually appears as a small nodule in the centre of the sternal cartilage mass of the clavicle [16]. There is remarkable consistency in the latest age at which this stage is observed, albeit Bassed et al. [13] demonstrated comparatively high age limits in both sexes in an Australian (Victorian) population (21 and 19 years for males and females, respectively). The variations in age ranges for stage 2 again demonstrate considerable consistency between the Western Australian and other comparative populations (Table 8). In considering the age ranges for stage 3, the lower limit in the male Western Australian sample is slightly higher than all of the other comparative populations (Table 5). This, however, may be related to the fact that there were only 14 males classified into this stage (see Table 4), and thus, this lower age limit may not be truly representative of the true level of population variability—the only way to further investigate this issue is by increasing the male sample in the appropriate age range (see below).
The stated ages for the earliest onset of complete fusion with a physeal scar still present (stage 4) are again remarkably consistent between all of the comparative groups, with the only noticeable outlier being the male Victorian (Australian) population, for which the earliest indications of complete epiphyseal fusion is recorded at 17 years of age [13]. All of the other comparative populations outlined in Table 8 demonstrate that the earliest attainment of stage 4 occurs at 21 years of age (with the exception of 20 years of age in the Western Australian females). In the present study, we identified remnants of a physeal scar in individuals well beyond 30 years of age (Table 4), a phenomenon that accords with similar research [34]; observation of the latter was most likely facilitated by the assessment of thin-slice scans. It is plausible, therefore, that the assessment of thicker-slice scans may result in the incorrect attribution of stage 5 due to reduced spatial resolution masking fine anatomical structures, such as the epiphyseal scar [30]. In a forensic context, it is thus important that stage 5 only be assigned if there is no trace of a physeal scar in any of the multiple axial CT slices in the region of interest.
The age of earliest onset of stage 5 is somewhat more variable between the comparative populations, with the result of the present study situated between the ranges reported in the literature (Table 8). The most divergent results are again for the Victorian (Australian) population, with the earliest onset of complete fusion without any associated evidence of an epiphyseal scar noted at 17 and 20 years of age in males and females, respectively (Table 8). The unusual results of Bassed et al. [13] may be related to the specific methodological approach employed, which involved applying the minimum age of the less developed side based on scoring the most representative slice in two CT images (see also Wittschieber et al [34]). It is perhaps prudent to suggest that any practical assessments made using that data should be interpreted in relation to the potential limitations described above.
Potential sources of variation
In the interpretation of the results of the present study to the data shown in Table 8, it is important to consider such comparisons in relation to the complex interaction of both intrinsic (e.g. physiological and genetic) and extrinsic (e.g. environmental and methodological) sources of potential variation. The complexity of different factors influencing growth and maturation is perhaps best explained by Sinclair, who states “…the sequence of ossification are primarily genetically controlled; the timing of ossification is partly influenced by genetic factors and partly by environmental ones” [46; p. 141]. As the latter topic has been considered in the biological literature, and more recently in relation to forensic practice, only a small selection of relevant extrinsic factors are considered here; further sources of information are accordingly provided for those readers seeking a more detailed treatment of this topic. Potential variation introduced by methodological approach and observer experience has also already been explored (see above) and is thus not discussed further. Other sources of potential variation that are not discussed further include anatomical shape variants in the morphology of interest (see above and [11, 27, 34]).
Partial volume effect
From Table 8, it is readily apparent that there is variation in the slice thickness of the scans assessed, ranging from 0.6 to 8 mm. It has been noted in the literature that discrepancies in ossification timing may relate to the assessment of lower-resolution scans (thicker slices) and the ‘partial volume effect’, which can result in the non-visualization of the requisite morphological features used to distinguish between successive developmental stages [10, 27]. Based on the assessment of CT scans reconstructed to slice thicknesses of 1, 3, 5 and 7 mm, Mühler et al. [30] empirically demonstrated that increasing slice thickness resulted in the assignation of higher clavicular ossification stages. Mühler et al. concluded that “The slice thickness of CT scans has a crucial impact on the evaluation of clavicle ossification status” and in relation to forensic practice, recommended “…that a slice thickness of 1 mm should be used for CT examinations of the clavicle to evaluate the ossification stage for forensic age estimation purposes, to ensure maximum accuracy and diagnostic reliability” [30; p. 17]. Artificially inflated age estimates are of obvious concern (and disadvantage) to individuals subject to assessment for age of majority [30].
Sampling bias
It is not unreasonable to posit that a larger sample will encompass a greater proportion of the total variation in the timing of skeletal development within a given population and thus be more representative of the region from which that data are derived. There are, however, acknowledged limitations of deriving population data based on the analysis of individuals referred for clinical evaluation, one of which is that there may be a lack of suitably high-resolution scans available for analysis representative of a particular age cohort (see above). The latter is somewhat more prevalent in relation to obtaining large numbers of thin-slice scans of juvenile individuals because standard clinical protocols generally align with ethical requirements to minimize dosage levels of potential deleterious radiation. So, as noted by Milenkovic et al. [10], clinicians will follow the ‘As Low as is Reasonably Achievable’ principle (ALARA), which is not necessarily conducive (albeit justifiably) to facilitating scans suitable for studies quantifying skeletal ontogeny (see also Cameriere et al. [11]). This can result in the unequal representation of individuals across different age groups, which could potentially bias the observed ranges of the developmental stages being assessed [47].
Although the latter may to some degree be unavoidable, in the interests of facilitating critical evaluation, it is important that studies of this nature outline sex-specific age distributions, especially given the fact that any bias present in the reference sample will likely affect age estimations based on that data [48]. This problem is known as ‘age mimicry’, which is defined as “…the tendency of age estimates to mimic the structure of the known-age reference samples…” [35; p. 73]. The application of Bayesian statistical approaches are, however, known to be less sensitive to the influence of age mimicry and developmental outliers [14, 35], which highlights the importance of such approaches in the identification sciences.
Socioeconomic status
It has been suggested that socioeconomic status reflects a complicated mixture of genetic and environmental influences contributing to variation in human skeletal development [49]. The exact aetiology of socioeconomic related growth differentials is difficult to discern, as there are many cofactors with inherently complex interrelationships that are not mutually exclusive, including (but not limited to) the following: nutrition (including regular, adequate and balanced meals); access to health education and appropriate medical care; poor home environment (e.g. dilapidated and/or crowded); and high stress levels (e.g. familial instability, increased risk of violence and uncontrollable life events) [23, 24]. With specific reference to the timing of ossification, it has been shown that a relatively low socioeconomic status delays development [21, 22], which means that the application of reference standards from a socioeconomically advanced population to a lower status group would result in an underestimation of skeletal age [8, 50].
In relation to the comparative populations shown in Table 8, they are all derived from regions considered to be of advanced socioeconomic standards, as indicated by ‘high’ to ‘very high’ Human Development Index (HDI) rankings [51—see also Milenkovic et al. [10] for further discussion specific to the European region]. It is thus unlikely that the variation observed in the timing of clavicular maturation between the comparative populations shown in Table 8 is the result of any significant variation in socioeconomic development. The latter assertion, however, cannot be empirically quantified without access to both the required data to determine socioeconomic standing, which in Western Australia is not recorded during clinical assessment (as such information is unlikely to have any medical relevance) and an amendment to legislation (National Statement on Ethical Conduct in Human Research—NHMRC) allowing the collection and dissemination of detailed patient information [28].
Conclusion
This study further supports the reliability of the five-stage medial clavicular epiphysis system of Schmeling et al. [8] as applied in high-resolution MDCT scans. The present study also presents for the first time sex-specific data for the timing of clavicular epiphyseal fusion based on the analysis of a contemporary Western Australian population. The developmental trajectory of the medial clavicle in the latter population is highly consistent to data reported for other global populations. The thorough statistical testing and evaluation of methods for forensic age estimation is essential because the ramifications of an incorrect assessment include the potential to bias judicial evidence leading to a miscarriage of justice; such issues were made poignantly clear in the findings of a recent Australian Human Rights Commission inquiry into the treatment of individuals suspected of people-smuggling offences [20].
References
Hartnett KM (2010) Analysis of age-at-death estimation using data from a new, modern autopsy sample—part I: pubic bone. J Forensic Sci 55:1145–1151
Işcan MY, Loth SR, Wright RK (1984) Age estimation from the rib by phase analysis: white males. J Forensic Sci 29:1094–1104
Meindl RS, Lovejoy CO, Mensforth RP, Walker RA (1985) A revised method of age determination using the os pubis, with a review and tests of accuracy of other current methods of pubic symphyseal aging. Am J Phys Anthropol 68:29–45
Buckberry JL, Chamberlain AT (2002) Age estimation from the auricular surface of the ilium: a revised method. Am J Phys Anthropol 119:231–239
The Scientific Working Group for Forensic Anthropology (SWGANTH) (2013) Age estimation. http://www.swganth.org/products--drafts.html
Schmeling A, Grundmann C, Fuhrmann A, Kaatsch HJ, Knell B, Ramsthaler F, Reisinger W, Riepert T, Ritz-Timme S, Rösing FW, Rötzscher K, Geserick G (2008) Criteria for age estimation in living individuals. Int J Leg Med 122:457–460
AGFAD. (2014). Study Group on Forensic Age Diagnostics of the German Association of Forensic Medicine. http://agfad.uni-muenster.de/english/start.htm
Schmeling A, Schulz R, Reisinger W, Mühler M, Wernecke KD, Geserick G (2004) Studies on the time frame for ossification of the medial clavicular epiphyseal cartilage in conventional radiography. Int J Leg Med 118:5–8
Schmeling A, Reisinger W, Geserick G, Olze A (2006) Age estimation of unaccompanied minors. Part I. General considerations. Forensic Sci Int 159:S61–S64
Milenkovic P, Djukic K, Djonic D, Milovanovic P, Djuric M (2013) Skeletal age estimation based on medial clavicle—a test of the method reliability. Int J Leg Med 127:667–676
Cameriere R, De Luca S, De Angelis D, Merelli V, Giuliodori A, Cingolani M, Cattaneo C, Ferrante L (2012) Reliability of Schmeling’s stages of ossification of medial clavicular epiphyses and its validity to assess 18 years of age in living subjects. Int J Leg Med 126:923–932
Tangmose S, Jensen KE, Villa C, Lynnerup N (2014) Forensic age estimation from the clavicle using 1.0T MIR—preliminary results. Forensic Sci Int 234:7–12
Bassed RB, Drummer OH, Briggs C, Valenzuela A (2011) Age estimation and the medial clavicular epiphysis: analysis of the age of majority in an Australian population using computed tomography. Forensic Sci Med Pathol 7:148–154
Langley Shirley N, Jantz RL (2010) A Bayesian approach to age estimation in modern Americans from the clavicle. J Forensic Sci 55:571–583
Bernat A, Huysmans T, Glabbeek F, Sijbers J, Gielen J, Tongel A (2014) The anatomy of the clavicle. Clin Anat 27:712–723
Scheuer L, Black S (2000) Developmental juvenile osteology. Academic, London
Ogata S, Uhthoff HK (1990) The early development and ossification of the human clavicle—an embryologic study. Acta Orthop 61:330–334
Black S, Scheuer L (1996) Age changes in the clavicle: from the early neonatal period to skeletal maturity. Int J Osteoarch 6:425–434
Fazekas IG, Kósa F (1978) Forensic fetal osteology. Akadémiai Kiadó, Budapest
Australian Human Rights Commission (2012) An age of uncertainty—inquiry into the treatment of individuals suspected of people smuggling offences who say that they are children. https://www.humanrights.gov.au/publications/age-uncertainty-inquiry
Schmeling A, Reisinger W, Loreck D, Vendura K, Markus W, Geserick G (2000) Effects of ethnicity on skeletal maturation: consequences for forensic age estimations. Int J Leg Med 113:253–258
Schmeling A, Olze A, Reisinger W, Geserick G (2005) Forensic age estimation and ethnicity. Leg Med 7:134–137
Bradley RH, Corwyn RF (2002) Socioeconomic status and child development. Annu Rev Psychol 53:371–399
Harrison GA, Weiner JS, Tanner JM, Barnicot NA (1977) Human biology: an introduction to human evolution, variation, growth and ecology. Oxford University Press, Oxford
Bogin B, MacVean RB (1983) The relationship of socioeconomic status and sex to body size, skeletal maturation, and cognitive status of Guatemala City schoolchildren. Child Dev 54:115–128
Adler NE, Ostrove JM (1999) Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci 896:3–15
Wittschieber D, Schulz R, Vieth V, Küppers M, Bajanowski T, Ramsthaler F, Püschel K, Pfeiffer H, Schmidt S, Schmeling A (2014) Influence of the examiner’s qualification and sources of error during stage determination of the medial clavicular epiphysis by means of computed tomography. Int J Leg Med 128:183–191
National Health and Medical Research Council (NHMRC) (2013) National statement on ethical conduct in human research—updated 2013. http://www.nhmrc.gov.au/guidelines/publications/e72
Australian Bureau of Statistics (ABS) (2012) Ancestry. http://www.abs.gov.au/websitedbs/censushome.nsf/home/factsheetsa?opendocument&navpos=450
Mühler M, Schulz R, Schmidt S, Schmeling A, Reisinger W (2006) The influence of slice thickness on assessment of clavicle ossification in forensic age diagnostics. Int J Leg Med 120:15–17
Cohen J (1968) Weighted kappa: nominal scale agreement provision for scaled disagreement or partial credit. Psych Bull 70:213
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Wilcoxon F (1945) Individual comparisons by ranking methods. Biom Bull 1:80–83
Wittschieber D, Schulz R, Vieth V, Küppers M, Bajanowski T, Ramsthaler F, Püschel K, Pfeiffer H, Schmidt S, Schmeling A (2014) The value of sub-stages and thin slices for the assessment of the medial clavicular epiphysis: a prospective multi-center CT study. Forensic Sci Med Pathol 10:163–169
Boldsen JL, Milner GR, Konigsberg LW, Wood JW (2002) Transition analysis: a new method for estimating age from skeletons. In: Hoppa RD, Vaupel JW (eds) Paleodemography: age distributions from skeletal samples. Cambridge University Press, Cambridge, pp 73–106
Kimmerle EH, Konigsberg LW, Jantz RL, Baraybar JP (2008) Analysis of age-at-death estimation through the use of pubic symphyseal data. J Forensic Sci 53:558–568
Shirley NR, Jantz RL (2011) Spheno-occipital synchondrosis fusion in modern Americans. J Forensic Sci 56:580–585
Lucy D (2010) The presentation of results and statistics for legal purposes.
Konigsberg LW, Herrmann NP, Wescott DJ, Kimmerle EH (2008) Estimation and evidence in forensic anthropology: age at death. J Forensic Sci 53:541–557
Franklin D, Flavel A (2014) Brief communication: timing of spheno-occipital closure in modern Western Australians. Am J Phys Anthropol 153:132–138
Rudolf E (2014) Comments to Focardi et al. Age estimation for forensic purposes in Italy: ethical issues. Int J Leg Med. doi:10.1007/s00414-014-1043-8
Schulze D, Rother U, Fuhrmann A, Richel S, Faulmann G, Heiland M (2006) Correlation of age and ossification of the medial clavicular epiphysis using computed tomography. Forensic Sci Int 158:184–189
Hillewig E, Degroote J, Van der Paelt T, Visscher A, Vandemaele P, Lutin B, D’Hooghe L, Vandriessche V, Piette M, Verstraete K (2013) Magnetic resonance imaging of the sternal extremity of the clavicle in forensic age estimation: towards more sound age estimates. Int J Leg Med 127:677–689
Hefner JT (2009) Cranial nonmetric variation and estimating ancestry. J Forensic Sci 54:985–995
Nakhaeizadeh S, Dror IE, Morgan RM (2014) Cognitive bias in forensic anthropology: visual assessment of skeletal remains is susceptible to confirmation bias. Sci Justice 54:208–214
Sinclair DC, Dangerfield P (1998) Human growth after birth. Oxford University Press, Oxford
Kreitner KF, Schweden FJ, Riepert T, Nafe B, Thelen M (1998) Bone age determination based on the study of the medial extremity of the clavicle. Eur Radiol 8:1116–1122
Wärmländer SK, Sholts SB (2011) Sampling and statistical considerations for the Suchey–Brooks method for pubic bone age estimation: implications for regional comparisons. Sci Justice 51:131–134
Tanner JM (1962) Growth at adolescence. Blackwell Scientific Publications, Oxford
Kellinghaus M, Schulz R, Vieth V, Schmidt S, Pfeiffer H, Schmeling A (2010) Enhanced possibilities to make statements on the ossification status of the medial clavicular epiphysis using an amplified staging scheme in evaluating thin-slice CT scans. Int J Leg Med 124:321–325
Anand S, Sen A (1994) Human Development Index: methodology and measurement (No. HDOCPA-1994-02). Human Development Report Office (HDRO), United Nations Development Programme (UNDP).
Kellinghaus M, Schulz R, Vieth V, Schmidt S, Schmeling A (2010) Forensic age estimation in living subjects based on the ossification status of the medial clavicular epiphysis as revealed by thin-slice multidetector computed tomography. Int J Leg Med 124:149–154
Schmidt S, Mühler M, Schmeling A, Reisinger W, Schulz R (2007) Magnetic resonance imaging of the clavicular ossification. Int J Leg Med 121:321–324
Webb PAO, Suchey JM (1985) Epiphyseal union of the anterior iliac crest and medial clavicle in a modern multiracial sample of American males and females. Am J Phys Anthropol 68:457–466
Jit I, Kulkarni M (1976) Times of appearance and fusion of epiphysis at the medial end of the clavicle. Indian J Med Res 64:773–782
Acknowledgments
The authors would like to thank A/Prof. Rob Hart, Frontier Medical Imaging International, Western Australia, for assistance with obtaining the CT scans. We also offer our thanks to the two anonymous reviewers who spent considerable time and effort in helping us to greatly improve this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Franklin, D., Flavel, A. CT evaluation of timing for ossification of the medial clavicular epiphysis in a contemporary Western Australian population. Int J Legal Med 129, 583–594 (2015). https://doi.org/10.1007/s00414-014-1116-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-014-1116-8