Abstract
Isotretinoin is considered to be a safe and effective therapy in otherwise therapy-resistant acne. Elevated serum creatine phosphokinase values with or without muscle-related symptoms in isotretinoin-treated patients have been reported and interpreted as benign phenomena, lethal cases have not been described yet. We present the case of a 20-year-old male who died from severe generalised rhabdomyolysis associated with isotretinoin treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Isotretinoin was originally designed and is usually prescribed for severe acneiform skin lesions but is also used for patients with moderate or mild acne unresponsive to antibiotic therapy [1]. Properly selected patients given adequate drug doses for 3 to 5 months will most often experience significant clinical improvement or total clearing [2]. It is considered to be a safe and effective therapy in otherwise therapy-resistant acne, particularly if given in a dose regimen of 1 mg/kg/day, or a cumulative dose of >120 mg/kg [3].
However, as most other highly efficient drugs, the adverse effects of isotretinoin cover a wide spectrum. For example isotretinoin is considered to significantly increase plasma levels of cholesterol and low-density-lipoprotein cholesterol [4] and to stimulate tissue plasminogen activator [5]. Furthermore, other side effects including teratogenicity, serotonin-deficient disorders, haematologic, dermatologic, musculoskeletal and ophthalmologic disturbances have been documented [6]. Just recently the drug committee of the German medical fraternity announced a possible association between isotretinoin and chronic inflammatory bowel diseases [7].
Reversible episodes of muscle damage during treatment with isotretinoin were described early in the drug's history, but no adequate explanation for this finding was provided [8, 9]. There is increasing evidence that strenuous exercise might provoke or worsen muscle weakness or pain [10–12]. Elevated serum creatine phosphokinase values with or without muscle-related signs or symptoms in isotretinoin-treated patients with acne have been reported and interpreted as benign phenomena [13–15].
As far as we know, this is the first described case of severe rhabdomyolysis with fatal outcome associated with isotretinoin treatment.
Patient
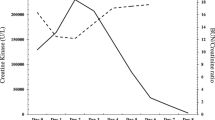
A 20-year-old male with an unremarkable medical history suffered from acne papulopustulosa, partim conglobata. Acne treatment was started 2.5 years before death (b.d.) with a combination of minocyclin tablets and topical gels (Duac® acne gel, Panoxyl® acne gel) which led initially to clinical improvement. About 12 months b.d., acne lesions worsened. Thus, 3.5 months b.d., pharmacological treatment was changed to isotretinoin capsules (40 mg/d). Two months b.d., laboratory blood tests (blood count, AST, ALT, gamma GT, HDL, LDL, triglycerides) during retinoid therapy showed normal results. Six weeks b.d. he first complained of severe myalgia and arthralgia after moderate exercise. The symptoms were reversible with diclofenac. Four weeks b.d. the young man stopped intake of isotretinoin shortly before travelling abroad during the following 3 weeks. This period of time was described by the patient as exhausting and sleepless. He noted increasing muscle pain from the first day of travel and showed signs of vitamin A intoxication (chapped lips, dry skin, loss of appetite, fatigue and aching muscles). Starting 6 days b.d., he suffered from dyspnoea on exertion and therefore decided to fly back home. He confined himself to his hotel during the next 3 days, while awaiting his return flight. On arrival at home 3 days b.d., he was immediately admitted to hospital where a fulminant rhabdomyolysis was diagnosed (CK 82,100 IU/ l; CK-MB 2,038 IU/l; troponin T 0.50 ng/ml). Despite intensive care, the young man died from ventricular fibrillation with a clinical picture of generalised rhabdomyolysis of unknown aetiology.
Results
Autopsy
The autopsy showed a young man of normal build (BMI 25). Macromorphological findings were nonspecific. The lungs exhibited severe oedema (right lung, 1 kg; left lung, 1.15 kg). Both skeletal and myocardial musculature were moist, soft, reddish-to-pale brown and friable. There were no underlying diseases and no signs of active acneiform lesions.
Histopathology
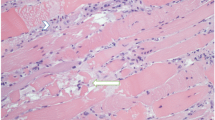
Post-mortem muscle biopsies were taken from quadriceps muscle, gastrocnemius muscle, diaphragm and heart. Histological investigation was performed according to medicolegal standards [16, 17]. Immunohistochemical reactions were performed with the antibodies anti-myogenin (polyclonal rabbit anti-human, DAKO Deutschland GmbH, Hamburg, Germany) and C5b-9 (monoclonal mouse anti-human, abcam Inc., Cambridge, USA). All striated muscles including the myocardium showed severe acute rhabdomyolysis with multiple necroses undergoing phagocytosis, ghost fibres and/or regenerating fibres without signs of inflammation (Fig. 1a and b, Fig. 2a and b). The histochemical stains (NADH-TR, SDH, ATPase, myoadenylate-deaminase, cytochrome-C-oxidase, Oilred O/ sudan-black, PAS-diastase, phosphorylase and acid phosphatase) gave normal results without any hint for muscular dystrophy or metabolic myopathies. Vacuolar myopathy due to dilatation of vesicles of the sarcoplasmic reticulum or t-tubuli indicative of thyreotoxic periodic paralysis or altered homeostasis respectively was not observed. Central-core disease as possible trigger for malignant hyperthermia could be excluded. Anti-myogenin staining of the kidneys showed a remarkable positive result indicating severe myoglobinuria due to the underlying rhabdomyolysis (Fig. 3).
Toxicology
Screening tests for common drugs showed negative results. The blood alcohol concentration was 0.0 %. Only the iatrogenic drugs tramadol, metoclopramide, diphenhydramine, lidocaine and amiodarone could be detected.
Molecular diagnostics
A pathogenic mutation of the carnitine palmitoyltransferase 2 gene was excluded.
Discussion
Subtle findings during autopsy are a great diagnostic challenge and require full correlation with the clinical history, and thorough post-mortem routine and esoteric testing. The importance of forensic histopathology and immunohistochemistry are vividly highlighted by this case report. Other examples of similar diagnostic challenges have been recently described [18–21].
Doubtless, the young man died from severe rhabdomyolysis affecting all striated muscle including vast areals of left and right myocard muscle (Fig. 2a and b). Kidneys showed severe myoglobinuria as morphologic correlate for the late complication of acute renal failure. The most common cause of rhabdomyolysis is muscular trauma; less common causes include drugs, toxins, infectious diseases, metabolic myopathies, muscle enzyme deficiencies, electrolyte abnormalities and endocrinopathies [22]. Rarely, central-core disease may trigger malignant hyperthermia resulting in rhabdomyolysis. Therapeutically administered minocyclin is known to possibly worsen preexisting myasthenia gravis; however, it is unsuspicious for causing rhabdomyolysis [23]. Concludingly, except for strenuous exercise 2 months before death we could not verify any other possible cause for rhabdomyolysis.
In the literature two other cases of acute rhabdomyolysis associated with isotretinoin treatment following physical exercise are reported [10, 11]. Our case, however, is the first described with a fatal outcome, although prescription followed established medical standards. The way that isotretinoin damages the cellular membrane, which leads to intracellular activation of calcium and deliberation of intracellular substances, is unclear.
We support the thesis that physical exercise, maybe even stress in general, provokes rhabdomyolytic symptoms in patients treated with isotretinoin [24]. We also believe that physicians in charge should be able to recognise rhabdomyolysis and manage it as this side effect should always be kept in mind under treatment with isotretinoin [11]. Thus, we suggest that monitoring of CK levels and muscle complaints should be among the standard follow-up for these patients. Patients should abstain from vigorous exercise during isotretinoin treatment and be counselled on the need to seek expert assessment for any musculoskeletal signs or symptoms.
References
Goulden V, Clark SM, McGeown C, Cunliffe WJ (1997) Treatment of acne with intermittent isotretinoin. Br J Dermatol 137:106–108
Shalita AR, Cunningham WJ, Leyden JJ, Pochi PE, Strauss JS (1983) Isotretinoin treatment of acne and related disorders: an update. J Am Acad Dermatol 9:629–638
Layton AM, Knaggs H, Taylor J, Cunliffe WJ (1993) Isotretinoin for acne vulgaris—10 years later: a safe and successful treatment. Br J Dermatol 129:292–296
Bershad S, Rubinstein A, Paterniti JR, Le NA, Poliak SC, Heller B, Ginsberg HN, Fleischmajer R, Brown WV (1985) Changes in plasma lipids and lipoproteins during isotretinoin therapy for acne. N Engl J Med 313:981–985
Dootson GM, Keidan J, Harper PL (1995) The influence of isotretinoin upon fibrinolysis in patients with acne. Br J Dermatol 133:66–70
Rote Liste (2010) Arzneimittelverzeichnis für Deutschland. Rote Liste Service GmbH, Frankfurt
Arzneimittelkommission der deutschen Ärzteschaft (2012) Aus der UAW-Datenbank. Isotretinoin und chronisch-entzündliche Darmerkrankung. Dtsch Ärztebl 109:A-1044/ B-900/ C-892
McBurney EI, Rosen DA (1984) Elevated creatine phosphokinase with isotretinoin. J Am Acad Dermatol 10:528–529
Hodak E, Gadoth N, David M, Sandbank M (1986) Muscle damage induced by isotretinoin. Br Med J 293:425–426
Guttmann-Yassky E, Hayek T, Muchnik L, Bergman R (2003) Acute rhabdomyolsis and myoglobinuria associated with isotretinoin treatment. Int J Derm 42:499–500
Gomez-Bernal S, Rodriguez-Pazos L, Rodriguez-Granados MT, Toribio J (2011) Rhabdomyolysis during isotretinoin therapy. Actas Dermosifiliogr 102:390–391
Trauner MA, Ruben BS (1999) Isotretinoin induced rhabdomyolysis? A case report. Dermatol Online J 5:2
Heudes AM, Laroche L (1998) Muscular damage during isotretinoin treatment. Ann Dermatol Venereol 125:94–97
Landau M, Mesterman R, Ophir J, Mevorah B, Alcalay J, Harel A, Nevo Y (2001) Clinical significance of markedly elevated serum creatine kinase levels in patients with acne on isotretinoin. Acta Derm Venereol 81:350–352
Kaymak Y (2008) Creatine phosphokinase values during isotretinoin treatment for acne. Int J Derm 47:398–401
Brinkmann B (1999) Harmonisation of medico-legal autopsy rules. Committee of Ministers. Council of Europe. Int J Leg Med 113:1–14
Ferrara SD, Bajanowski T, Cecchi R, Snenghi R, Case C, Viel G (2010) Bio-medical guidelines and protocols: survey and future perspectives in Europe. Int J Leg Med 124:345–350
Fracasso T, Karger B, Pfeiffer H, Sauerland C, Schmeling A (2010) Immunohistochemical identification of prevalent right ventricular ischemia causing right heart failure in cases of pulmonary fat embolism. Int J Legal Med 124:537–542
Hartung B, Schott M, Daldrup T, Ritz-Timme S (2010) Lethal thyroid storm after uncontrolled intake of liothyronine in order to lose weight. Int J Legal Med 124:637–640
Cecchi R, Cipollini L, Sestili C, Aromatario M, Ciallella C (2011) Pulmonary embolisation of bone fragments from penetrating cranial gunshot wounds. Int J Legal Med. doi:10.1007/s00414-011-0643-9
Fracasso T, Schmeling A (2009) Delayed asphyxia due to inhalation injury. Int J Legal Med 125:289–292
Huerta-Alardin AL, Varon J, Marik PE (2005) Bench-to-bedside review: rhabdomyolysis—an overview for clinicians. Crit Care 9:158–169
Fachinformation Minocyclin-CT 50 mg Kapseln (2012) http://www.fachinfo.de/data/fi/jsearch?praep. Accessed 18 July 2012
Chroni E, Monastirli A, Tsambaos D (2010) Neuromuscular adverse effects associated with systemic retinoid dermatotherapy. Drug Saf 33:25–34
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hartung, B., Merk, H.F., Huckenbeck, W. et al. Severe generalised rhabdomyolysis with fatal outcome associated with isotretinoin. Int J Legal Med 126, 953–956 (2012). https://doi.org/10.1007/s00414-012-0750-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-012-0750-2