Abstract
We report on a sudden cardiac death case involving a 40-year-old man with no known medical history. Forensic autopsy showed lymphocytic myocarditis associated with lymphocytic thyroiditis. In both the heart and the thyroid gland, the inflammatory foci often had a nodular pattern with a germinal centre. Virological and toxicological analyses were negative. Postmortem biochemistry showed a slight increase in TSH in combination with normal T3 and T4 blood levels suggesting hypothyroidism. High titres of antiperoxidase and antithyroglobulin antibodies with normal levels of TSH receptor antibodies, in addition to biological hypothyroidism and lymphocytic inflammation were consistent with the diagnosis of Hashimoto’s thyroiditis. Immunohistochemical studies excluded a lymphoma and showed no evidence of viral myocarditis. In contrast to Grave’s disease, Hashimoto’s thyroiditis has never been reported in association with myocarditis as a cause of sudden death. We conclude that the cardiac immunological and histological pattern, similar to that found in the thyroid gland suggests an autoimmune myocarditis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocarditis is a frequent cause of sudden death in young adults [1, 2] and a viral infection is the most frequent of the various etiologies reported in the literature [1, 3]. Although myocarditis and Graves’ disease and/or hyperthyroidism are a well known association, Hashimoto’s disease and/or hypothyroidism have never been reported in combination with myocarditis. We report on an autopsy case of myocarditis associated with Hashimoto’s thyroiditis and examined the possible causes.
Case history
A 40-year-old man was found dead in his home early in the morning by his wife. His body was lying on a sofa. The deceased had no known medical history and took no medications.
Autopsy findings
A forensic autopsy was performed, the body mass index was 39.3, the heart weighed 415 g and had a normal appearance. The thyroid gland was slightly increased in weight (36 g), but was otherwise normal. There were no traumatic lesions.
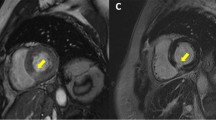
Histological examination of the heart showed numerous inflammatory foci in both ventricles. The inflammatory foci had often a nodular pattern with a germinal centre (Fig. 1) and the inflammation was associated with cardiomyocyte necrosis (Fig. 1). Inflammatory infiltrates consisted of a majority of lymphocytes with some macrophages, small lymphocytes were predominant, associated with larger ones in the nodules (Fig. 1). There were no polymorphonuclear cells. In addition to acute lesions there were also healed lesions.
Immunohistochemistry showed a majority of CD3 (Dako, polyclonal antibody) and CD5 (NovoCastra, monoclonal antibody) T lymphocytes (Fig. 2a), associated with CD20 (Dako, monoclonal antibody) B lymphocytes in nodular inflammatory foci (Fig. 2b). Latent membrane protein-1 (LMP-1) and the EBV EBER probe (PanPath) were negative for Epstein Barr viruses and Bcl2 (Dako, monoclonal antibody) and Ki67 (Dako, polyclonal antibody) were also negative. Histology of the thyroid gland showed numerous lymphoid follicles (Fig. 3) with a CD 20 positive germinal centre (Fig. 4a). Peripheral lymphocytes were mostly of CD3 and CD5 phenotype (Fig. 4b) and a lymphoma was excluded. There were no lymphoepithelial lesions as confirmed by normal cytokeratin AE1-AE3 clone (Dako, monoclonal antibody) expression. Bcl2 and Ki67 were negative and other organs were normal.
Biological findings
Toxicological analyses were negative and virological analyses were also negative including viral cultures and RT-PCR for enterovirus RNA. No Echo viruses or Coxsackie viruses were found and α-IFN postmortem blood levels were not increased.
Table 1 details the results of the postmortem hormonal levels. The thyroxin (T4) blood level was normal, whereas TSH was slightly increased and triiodothyronin (free T3) was found to be in the normal range. There were significantly high titres of autoantibodies including anti-thyroid peroxidase and anti-thyroglobulin, but there were no anti-TSH-receptor or anti-myosin antibodies.
Discussion
The cause of death was assessed to have been a lymphocytic myocarditis associated with a chronic lymphocytic thyroiditis. Such an undiagnosed chronic thyroiditis has been described in cases of sudden death [4] and in our case, postmortem biochemistry results were consistent with Hashimoto’s disease. Edston et al. [5] showed that it is possible to use postmortem measurements of thyroid function in combination with histology but postmortem thyroxin and TSH blood levels must be carefully interpreted. Indeed, thyroxin has also been found to decrease after death [6, 7]. However, according to Coe [6], TSH remains fairly constant within 2 days after death and in our case, the autopsy was performed 24 hours after death. Triiodothyronin (free T3) was found to be in the normal range. However, postmortem values have been shown to vary dramatically after death and therefore this is not considered to be reliable to predict the antemortem thyroid status of the deceased [7]. In our case, the slight increase in TSH in combination with a normal thyroxin level may be indicative of hypothyroidism. High titres of antiperoxidase and antithyroglobulin antibodies without anti-TSH-receptor antibodies, in addition to hypothyroidism and lymphocytic thyroiditis are consistent with the diagnosis of Hashimoto’s thyroiditis.
In contrast to hyperthyroidism and Graves’ disease, hypothyroidism and Hashimoto’s thyroiditis have never been reported in association with myocarditis as a cause of sudden death [8, 9, 10, 11, 12, 13, 14]. Some sudden deaths have been reported in hypothyroidism, but they were found to be related, not to myocarditis but to cardiomyopathy or pericarditis [15]. The reason why myocarditis has been found exclusively in hyperthyroidism and Graves’ disease and not in hypothyroidism and Hashimoto’s thyroiditis is not known.
This raises the question of the possible causes of myocarditis when associated with Hashimoto’s disease. In our case, no viruses were detected but some authors have detected viral genomes in the myocardium of patients with myocarditis, using sensitive molecular techniques [1]. A prevalence of enteroviral RNA in endomyocardial biopsies from patients with myocarditis was found to be 4% in a recent study [3]. Although we cannot exclude viral myocarditis in our case, another possibility is an autoimmune myocarditis associated with Hashimoto’s disease. In our case, the myocardial inflammatory foci often had a nodular pattern with a germinal centre and as this pattern is not encountered in viral infections it might be indicative of an autoimmune process. Furthermore, histological and immunohistochemical patterns of the thyroid inflammatory infiltrates were similar to those found in the heart. In our case, the presence of B lymphocytes in nodular foci might also be indicative of an autoimmune process. The absence of cardiac anti-myosin autoantibodies could be explained by an early postmortem degradation. Our immunohistochemical study excluded both a cardiac and thyroid lymphoma.
In conclusion, our findings are consistent with an autoimmune myocarditis rather than a viral infection. Although the prevalence is likely to be low, it might be underestimated since on the one hand myocarditis may remain asymptomatic, and on the other hand sudden death victims are unfortunately rarely autopsied. As far as medicolegal implications are concerned, myocarditis should be kept in mind when investigating autoimmune thyroiditis in the clinical practice so as not to overlook the risk of sudden death, especially in patients with unexplained thoracic symptoms and/or electrocardiographic changes. In addition, our case report underlines the usefulness of postmortem biochemistry and the necessity of a complete autopsy, including systematic histological examination, toxicological and microbiological analyses, when investigating a sudden unexplained death. A better understanding of cardiac sudden death also requires a full investigation of the cardiac conduction system [16] and useful complementary techniques such as quantification of myocardial contraction bands [17], immunohistochemistry [18] and the TUNEL method [19].
References
Feldman AM, McNamara D (2000) Myocarditis. New Engl J Med 343:1388–1398
Loire R (1999) La mort subite cardiovasculaire. Ann Pathol 19:203–211
Pankuweit S, Portig I, Eckhardt H, Crombach M, Hufnagel G, Maisch B (2000) Prevalence of viral genome in endomyocardial biopsies from patients with inflammatory heart muscle disease. Herz 25:221–226
Edston E (1996) Three sudden deaths in men associated with undiagnosed chronic thyroiditis. Int J Legal Med 109:94–97
Edston E, Druid H, Holmgren P, Öström M (2001) Postmortem measurements of thyroid hormones in blood and vitreous humor combined with histology. Am J Forensic Med Pathol 22:78–83
Coe JI (1973) Postmortem values of thyroxine and thyroid-stimulating hormones. J Forensic Sci 18:20–24
Rachut E, Rynbrandt DJ, Doutt TW (1980) Postmortem behavior of serum thyroxine, trioiodothyronine, and parathormone. J Forensic Sci 25:67–71
Simson LR (1976) Thyrotoxicosis: postmortem diagnosis in an unexpected death. J Forensic Sci 21:831–832
Polikar R, Burger AG, Scherrer U, Nicod P (1993) The thyroid and the heart. Circulation 87:1435–1441
Fatourechi V, Edwards WD (2000) Grave’s disease and low-output cardiac dysfunction: implications for autoimmune disease in endomyocardial biopsy tissue from eleven patients. Thyroid 10:601–605
Nora ED, Flaxman N (1943) The heart in experimental thyrotoxicosis. J Lab Clin Med 28:797–808
Wright EA (1957) A case of malignant exophthalmos associated with a fatal myocarditis. Guy’s Hosp Rep 106:36–46
Letter EA de , Piette MHA, Lambert WE, Leenheer AP de (2000) Medico-legal implications of hidden thyroid dysfunction: a study of two cases. Med Sci Law 40:251–257
Ortmann C, Pfeiffer H, Du Chesne A, Brinkmann B (1999) Inflammation of the cardiac conduction system in a case of hyperthyroidism. Int J Legal Med 112:271–274
Saphir O (1942) Myocarditis. Arch Pathol 33:88–137
Nishida N, Ikeda N, Kudo K, Tsuji A, Kiyoshima A (2002) Forensic significance of conduction system abnormalities as a precise cause of accidental death. Int J Legal Med 116:344–349
Baroldi G, Mittleman RE, Parolini M, Silver MD, Fineschi V (2001) Myocardial contraction bands. Definition, quantification and significance in forensic pathology. Int J Legal Med 115:142–151
Dettmeyer R, Reith K, Madea B (2002) Alcoholic cardiomyopathy versus chronic myocarditis—immunohistological investigations with LCA, CD3, CD68 and tenascin. Forensic Sci Int 126:57–62
Edston E, Gröntoft L, Johnsson J (2002) TUNEL: a useful screening method in sudden cardiac death. Int J Legal Med 116:22–26
Acknowledgements
The authors thank Diane Damotte, MD, PhD, haematopathologist, for her advice in immunohistochemical analyses.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lorin de la Grandmaison, G., Izembart, M., Fornes, P. et al. Myocarditis associated with Hashimoto’s disease: a case report. Int J Legal Med 117, 361–364 (2003). https://doi.org/10.1007/s00414-003-0392-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-003-0392-5