Abstract
Recently, gold-coated iron oxide nanoparticles (Au@IONPs) have received a great deal of attention in cancer therapy. In this in vitro study we aimed to investigate the anti-cancer effects of Au@IONPs core–shell nanoparticles when applied in thermo-radiotherapy. Moreover, we investigated the level of apoptosis induced in U87-MG human glioma cells after receiving a combinatorial treatment regimen (Au@IONPs + hyperthermia + radiotherapy). Firstly, the Au@IONPs nanocomplex was prepared and characterized. Cytotoxicity of the nanoparticles (various concentrations; 4 h incubation time) was investigated on U87-MG cells and finally the concentrations of 10 and 15 µg/mL were selected for further studies. After incubation of the cells with nanoparticles, they received hyperthermia (43 °C; 1 h) and then were immediately exposed to 6 MV X-ray (2 and 4 Gy). Following the treatments, MTT assay was used to analyze cell viability and flow cytometry was used to determine the level of apoptosis in each treatment group. The results revealed that nanoparticles have no significant cytotoxicity at concentrations lower than 10 µg/mL. Also, we observed that nanoparticles are able to enhance the cytotoxic effect of hyperthermia and radiation. The major mode of cell death was apoptosis when nanoparticles, hyperthermia and radiation were concomitantly applied to cancer cells. In conclusion, Au@IONP nanoparticle can be considered as a good thermo-radio-sensitizer which triggers significant levels of apoptosis in cancer therapy.
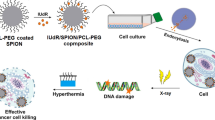
Graphical abstract

In this in vitro study, we report the anti-cancer effects of gold-coated iron oxide nanoparticles (Au@IONPs) when applied in thermo-radiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common and malignant type of brain tumors which is characterized by outspread invasion through the brain. Unrestricted cellular multiplications, durable angiogenesis, gentle necrosis, resistance against apoptosis and conventional treatment, molecular instability and normal brain tissue loss are the most important signs of glioblastoma tumors (Furnari et al. 2007). Surgery, chemotherapy, and radiation therapy are the main treatment modalities of brain tumors. In spite of broad advancement in these fields, the survival of patients is poor (Mahdavi et al. 2016; Sun et al. 2013). In the process of treatment, each of the mentioned methods has particular restrictions. Brain tumors are often inaccessible and sometimes are not available for neurosurgeons during operation (Hehr et al. 2003). The most important limitation that prevents a successful use of chemotherapy is intolerable side effects (due to systemic distribution and high toxicity of drugs) imposed to the patients (Sudhakar 2009). Considering the benefits of radiotherapy, particularly for brain tumors, this method also has serious complications. One of the most important complications is that the recommended high doses of radiotherapy are harmful for the healthy brain tissue around the tumor (Witteles 2011; Manjili et al. 2014). These restrictions encourage investigations of new methods for cancer therapy (Sun et al. 2013; Zhou et al. 2011).
In addition to all conventional treatment modality mentioned above, hyperthermia is considered as another cancer treatment method (Beik et al. 2016a, b). In hyperthermia, the temperature of the whole body or a part of the body is raised to 43–48 °C which causes destruction of intracellular structures and changes in cytoskeleton organization, cytoplasmic membranes and proteins. These damages lead to cancer cell death. Another advantage of hyperthermia is its efficient effects when combined with radiotherapy. Heating the tissue enhances blood flow and, consequently, increases tumor tissue oxygen level that can strengthen radiotherapy response. Therefore, hyperthermia can be considered as a method of radiosensitizing cancer cells (Chicheł et al. 2007; Hildebrandt et al. 2002). In spite of all benefits mentioned for hyperthermia, it suffers from non-selectivity (Samadian et al. 2016). This means that both normal and cancer cells absorb the heat, limiting the therapeutic benefit (Verma et al. 2014).
With the advent of nanotechnology and considering the profound effects of various nanomaterials, new cancer treatment methods are under investigation (Bañobre-López et al. 2013; Cabuy 2011; Van der Zee 2002; Beik et al. 2017). The gold nanoparticle (AuNP) has a high atomic number (Z) and, as a result, a high photon absorption cross-section (Li et al. 2016). The nanoparticle can enhance the biological effects of radiation in cancer cells, such as increasing the level of apoptosis. Since they have high biocompatibility, AuNPs are a good choice to be applied in various biomedical fields, particularly in cancer hyperthermia and radiotherapy (Khoshgard et al. 2014). Magnetic nanoparticles, such as iron oxide nanoparticle (IONP), are considered as another class of nanoparticles with a high potential in various fields of biomedicine (for example in cancer diagnosis and therapy) (Eyvazzadeh et al. 2017). IONPs can play a role as a contrast agent in magnetic resonance imaging contributing to better and more sensitive cancer diagnosis protocols (Manjili et al. 2014). Nanoparticles with high magnetic power, high heat absorption, low toxicity and large amounts of accumulation in the tumor are helpful and have been recently introduced into the area of cancer hyperthermia and radiotherapy (Verma et al. 2014; Mirrahimi et al. 2017; Silva et al. 2011). There is a possibility that in the presence of magnetic nanoparticles, the cell absorbs more heat increasing oxidative stress, ultimately augmenting cell death (Soares et al. 2012; Esmaelbeygi et al. 2015; Cabada et al. 2012). Moreover, significant effects of IONPs on cancer cell thermosensitizing and radiosensitizing have been recently reported (Esmaelbeygi et al. 2015).
A major problem in treating brain tumors using nanotechnology-based hyperthermia or radiotherapy is the blood–brain barrier (BBB) that does not allow the therapeutic agents to enter the brain tissue. However, there is some evidence demonstrating that nanotechnology-assisted cancer therapy overcomes the BBB by several mechanisms: (1) brain tumors cause serious damage to the BBB and disrupt its integrity, (2) radiation can also destruct the BBB enabling nanoparticles to cross the BBB, (3) some nanoparticles, such as magnetic nanoparticles, can cross the BBB through leaky vessels of brain tumors and remain in the lesion because of a physiologic phenomenon known as enhanced permeability and retention (EPR) (Maeda et al. 2009; Joh et al. 2013).
Considering the potentials of gold and magnetic nanoparticles outlined above, it is interesting to investigate the biological effects of both AuNPs and IONPs. Hoopes et al. have recently studied the effect of IONPs and AuNPs in combination with hyperthermia and radiotherapy. The results of their studies confirm that the application of these nanoparticles induce better responses to radiotherapy and hyperthermia (Hoopes et al. 2007; Hu et al. 2017). In addition, the Au@IONPs core–shell nanoparticles have received a great deal of attention in cancer therapy (Miyake et al. 2008). The aim of the present in vitro study was to investigate the anti-cancer effect of Au@IONPs nanoparticles in combination with radiotherapy and hyperthermia using U87-MG human glioma cells. Given the diverse biological consequences of inducing necrosis versus apoptosis, we specifically focused on the process of apoptosis induction.
Materials and methods
Materials
Au@Fe2O3 core–shell nanoparticles (NP, code: NB-CS-30) were purchased from Nanobon Company (Tehran, Iran). A brief explanation of the nanoparticle synthesis procedure is given in the next section. The U87-MG cell line was received from the Pasteur institute (Tehran, Iran). Dulbecco’s Modified Eagle’s Medium (DMEM) and fetal bovine serum (FBS) were purchased from GIBCO (Invitrogen, Germany). Trypsin ethylene diamine tetra acetic acid (EDTA) and penicillin–streptomycin solution and dimethyl sulfoxide (DMSO) and MTT(3-(Hehr et al. 2003)-2, 5-diphenyltetrazolium bromide) were purchased from Sigma (St Louis, MO, USA). Flow cytometry kit (Annexin V/PI) was purchased from eBioscience company (San Diego, CA, USA).
Synthesis of Au@IONPs nanoparticles
Au@Fe2O3 core–shell NPs were prepared through the oxidation of Fe3O4 NPs in the aqueous phase (Kang et al. 1996). Briefly, 2.6 g of FeCl3 and 1.0 g of FeCl2 were dissolved in HCl solution (12 M) and 12.5 mL of H2O. The solution was introduced into a NaOH solution through dropwise addition (125.0 mL, 1.5 M) with vigorous stirring. The generated black precipitate was collected using a magnet and the supernatant was removed from the precipitate through decantation. After being washed three times using 50 mL of water, HCl solution (250 mL, 0.01 M) was added to neutralize the anionic charges of the precipitate; the resulting Fe3O4 NPs were obtained after washing with water. The freshly prepared Fe3O4 NPs were further dissolved in HNO3 (0.01 M) and heated under stirring at 100 °C for 1 h to completely oxidize the Fe3O4 NPs to Fe2O3 NPs. The solution was then cooled to room temperature and washed twice using water, followed by centrifugation at 10,000 RPM for 15 min. Au@Fe2O3 core–shell NPs were synthesized through the deposition of Au on Fe2O3 NPs using the modified Lyon’s iterative hydroxylamine-seeding procedure (Lyon et al. 2004). First, Fe2O3 NPs (1.0 mL, 1.1 mM) were mixed with sodium citrate (1.0 mL, 0.1 M) for 10 min, followed by dilution to 20 mL using H2O. Subsequently, 0.1 mL of NH2OH·HCl solution and 1.0 mL of HAuCl4 solution were added dropwise under stirring for a total of 50 min. The addition of NH2OH·HCl and HAuCl4 was repeated twice more. The solution changed to garnet after three iterative additions.
Characterization of nanoparticles
The morphology and shape of Au@IONPs were determined using transition electron microscopy at an accelerating voltage of 200 KV and a scanning electron microscopy at 26 KV (EM3200 model, KYKY company, China). The hydrodynamic size and zeta potential distributions of nanoparticles were investigated by a Nano-ZS 90 Nanosizer (Malvern Instruments Ltd., Worcestershire, UK).
Cell culture
The human glioblastoma cell line U87-MG was used in this in vitro study. U87-MG cells were cultured in high-glucose DMEM containing 10% FBS and 1% penicillin/streptomycin. Cells were kept in an 37 °C incubator with 5% CO2 and the cells were sub-cultured twice a week upon reaching approximately 80% confluency.
Nanoparticle cytotoxicity and cellular uptake assay
To test the cytotoxicity of core–shell nanocomplex, the viability of the cells incubated with various concentrations of the nanocomplex was evaluated using the MTT tetrazolium assay, which measures the ability of metabolically active mitochondria in live cells to reduce a colorless tetrazolium compound to a blue formazan product. To perform this assay, we seeded 1 × 104 U87-MG cells into each well of a 96-well microplate and after 24 h incubation, cells were incubated with various concentrations of nanocomplex (0–30 µg/mL) for 4 h. Then, the nanocomplex was removed and cells were washed with PBS. MTT assay was performed 24 h post-treatment. After adding 100 µl of FBS-free culture medium, 10 µl of MTT dye (at a concentration of 5 mg/mL) was also added to each well, and the plate was incubated for 4 h. Then, MTT-containing medium was removed and replaced with DMSO (10 µl per well) to dissolve the formazan crystals and kept in the dark at room temperature for 15 min. Finally, the absorbance of the dissolved formazan was read at a wavelength of 570 nm by an ELISA reader (DYNEX MRX, USA) using a reference wavelength of 630 nm. The relative survival of U87-MG cells was expressed as the absorbance of the treated sample/absorbance of the control group. The optical density (OD) of dissolved formazan is directly proportional to the number of living cells. All experiments were done in triplicate. In our experiments, we designed control groups beside the treated groups and the percentage of viable cells was calculated by the following formula:
After incubation of U87-MG cells with nanoparticles for 4 h, ICP-MS and TEM analyses were performed to determine the uptake of the nanoparticles by cancer cells. The cells that had been exposed to nanoparticles at a concentration of 15 µg/mL and incubated for 4 h were processed for TEM analysis. Samples were fixed with 2.5% glutaraldehyde, pH 7.2. After primary fixation, the samples were intensively rinsed with 0.1M phosphate buffer (pH 7.2), then post-fixed with 1% OsO4 for 2 h and finally dehydrated in an acetone solution. The resulting dried specimens were embedded in Epoxy Resin (TAAB 812) which was polymerized at 60 °C for 48. Thin, 70 nm sections were sliced for TEM analysis using an ultramicrotome. Sections were transferred on 200 mesh grids and stained with heavy metals (uranyl acetate and lead citrate). Stained samples were visualized under TEM LEO 906 (80 kV).
For ICP-MS studies, 4 × 105 cells incubated with nanoparticles at a concentration of 15 µg/mL for 4 h and were analyzed using ICP-MS ELAN DRC-e spectrometer (PerkinElmer SCIEX, Concord, Ontario, Canada). The incubated cells were digested in 3 mL of aqua regia. Following digestion, samples were diluted to 10 mL with reagent water and analysis was performed for gold.
Hyperthermia and radiation therapy
Hyperthermia was applied to the cells using a water bath hyperthermia system. In this treatment method, U87-MG cells were immersed in a water bath and maintained at a constant temperature of 43 °C for 1 h.
For analyzing the impact of radiation, the U87-MG cells were irradiated by a medical LINAC accelerator (Siemens, Germany, running at 6 MV) with doses of 2 and 4 Gy. Cells received the exposure from posterior at a distance of 100 cm from the bottom of the plate and radiation field size was 40 × 40 cm.
Combined effect of hyperthermia and radiotherapy
To study the combinatorial effects of hyperthermia and radiotherapy (with or without nanoparticles), the U87-MG cells were cultured in 96-well microplates and maintained in an incubator for 24 h. After removing the culture medium, nanoparticles at concentrations of 10 and 15 µg/mL were added to each well and then maintained in an incubator for 4 h. Then, U87-MG cells received hyperthermia (at 43 °C) for 1 h. After hyperthermia, the cells were irradiated with 2 and 4 Gy of X-ray. The average time between hyperthermia and radiotherapy was 10 min. After a combined treatment, the cells were kept in an incubator for 24 h and analyzed for viability by the MTT assay.
Flow cytometry
The level of apoptosis was measured using an annexin V–fluorescein isothiocyanate (FITC) apoptosis detection kit, as described in the manufacturer’s instruction (eBioscience, USA). In brief, cells were plated in 6-well plates at a concentration of 5 × 105 cells/mL and the plates were kept in an incubator for 24 h. Then, various treatment modalities were applied. After 24 h, the cells were harvested and centrifuged at 300 g for 5 min. Then, the cells were washed once with PBS and once with 1 × binding buffer. After that, cells were suspended in 1 × binding buffer and 5 µl of fluorochrome-conjugated annexinV was added to 100 µl of cell suspension and incubated for 15 min in dark at room temperature. Cells were washed with 2 mL of binding buffer and suspended in 200 µl of 1 × binding buffer. Finally, 5 µl of propidium iodide (PI) staining solution was added to 200 µl of cell suspensions and assessed by a flow cytometer (BD FACSCantoII, USA).
Statistical analysis
Statistical analysis was performed using the SPSS software (version 11). One-way analysis of variance (ANOVA) was used to evaluate the significance of results. A value of p < 0.05 was considered as statistically significant.
Results
Nanoparticles: characteristics and cell uptake
The size, shape and morphology of the prepared Au@IONPs were investigated by TEM and SEM. Images of nanoparticles are shown in Fig. 1. The nanoparticles were spherical in shape and the gold shell on iron oxide core is evident. Figure 2 shows that the hydrodynamic size distribution of nanoparticles ranged from 20 to 50 nm. Zeta potential is an indicator of the surface charge of nanoparticles and it was estimated as 17.9 mV (Fig. 3). To confirm that the nanoparticles were efficiently taken up by the cells, TEM visualization was conducted. The result confirmed the presence of particles in the cell cytoplasm and mitochondria (Fig. 4). ICP-MS studies also confirmed the internalization of nanoparticles (0.1 ng Au per cell).
Cytotoxicity of nanoparticles
Following a 4-h incubation of cells with different concentrations of nanoparticles (0–30 µg/mL), cell viability was evaluated 24 h later using the MTT assay. As shown in Fig. 5, Au@IONPs at concentrations below 10 µg/mL had no significant effect on cell viability, but higher concentrations considerably decreased the viability of U87-MG cells.
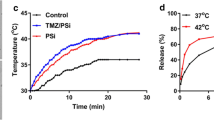
Thermosensitizing and radiosensitizing effect of nanoparticles
In vitro thermal effects of nanoparticles were investigated as described in the section “Hyperthermia and radiation therapy”. Moreover, to assess the radiosensitizing effect of nanoparticles, cells were incubated with nanoparticle concentrations of 10 and 15 µg/mL for 4 h and then exposed to 2 and 4 Gy of 6 MV X-ray radiation. Cell viability was analyzed after 24 h by the MTT assay. As seen in Fig. 6, nanoparticles potentiated the effect of hyperthermia in a dose-dependent manner. Figure 7 shows the impact of nanoparticles on the viability of cells exposed to ionizing radiation. The combination of radiation and nanoparticles induced a modest inhibition of cell growth. For example, when cells were exposed to 2 Gy alone, cell viability was 87%, while it was 75% and 73% for cells incubated with 10 and 15 µg/mL of Au@IONPs, respectively.
Combination of hyperthermia, radiation and nanoparticles
The details of this experiment are described in section “Combined effect of hyperthermia and radiotherapy”. 24 h after the combined treatment the MTT assay was performed and the results are shown in Fig. 8. In comparison to hypothermia and radiation alone, cell viability decreased when the cells were exposed to hyperthermia and radiation in the presence of nanoparticles.
Apoptosis analysis
One of the most important types of cell death is apoptosis. We, therefore, quantified apoptosis induced by each treatment group. Only the nanoparticle concentration of 15 µg/mL was applied and apoptosis was analyzed by flow cytometry. The results are shown in Figs. 9 and 10. Right lower and upper quadrants of the flow cytometry diagrams show early and late apoptosis, respectively. The sum of the two apoptosis types is presented in Fig. 11 as total apoptosis. No apoptosis was seen in control cells. The combination of hyperthermia and 2 and 4 Gy of radiation induced 18% and 23% apoptotic cells, respectively. 15 µg/mL of nanoparticles increased these values to 39% and 42%.
Discussion
Gold-coated iron oxide nanoparticles (Au@IONPs) have a high potential in biomedical research areas such as cancer diagnosis and therapy (Mahdavi et al. 2016). In this study, we have prepared the Au@IONP nanocomplex and examined its properties as a thermo-radio-sensitizer in therapy of gliomas. The nanocomplex is made of iron oxide nanoparticles which is advantageous for enhancing hyperthermia effects and has a gold layer in its structure which enhances the radiotherapy efficacy (Ban et al. 2005; Park et al. 2007).
We observed an inverse correlation between the dose of the Au@IONP nanoparticles and cell viability. A similar result was reported by Mateo et al. who studied the effect of AuNPs on HL-60 and HepG2 cells (Mateo et al. 2014). The reason of cell death induced by nanoparticles is most probably due to the induction of reactive oxygen species (ROS) leading to apoptosis (Wahab et al. 2014; Gopinath et al. 2010; Butterworth et al. 2010).
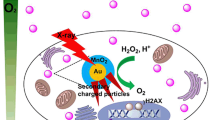
Moreover, we observed that Au@IONPs can act as a potent radiosensitizer for megavoltage X-rays as used in external beam radiotherapy. The mechanism of the radiosensitizing effect strongly depends on the X-ray energy. In orthovoltage radiotherapy, the major effects of nanoparticles are due to the photoelectric phenomenon. In megavoltage radiotherapy, nanoparticles enhance the radiotherapy response through chemical or biological mechanisms such as the formation of ROS, induction of DNA damage and DNA repair inhibition (Her et al. 2015; Butterworth et al. 2013; Sicard-Roselli et al. 2014). Yi et al. investigated the radiosensitizing effect of PEGylated Au@MnO2 nanoparticles in combination with megavoltage X-rays (Yi et al. 2016). They demonstrated that the level of DNA damage was highest in the treatment group receiving both Au@MnO2 nanoparticles and radiation. In another study, Wang et al. tested thioglucose-AuNP as a radiation enhancer in the breast cancer cell line MDA-MB-231. Their results showed that the nanoparticles influence cell cycle progression and sensitize the cells to ionizing radiation so that a significant reduction in survival fraction can be achieved (Wang et al. 2015). In addition, McMahon et al. demonstrated that heavy atom nanoparticles potentiate the effect of radiation by increasing the level of radiation-induced DNA damage (McMahon et al. 2011).
To achieve a better efficacy in cancer treatment, we tested the impact of Au@IONPs on the combination of hyperthermia and radiotherapy. Au@IONPs decreased the viability of cells exposed to both factors beyond the effect expected by assuming additivity (Table 1). To mimic the scenario of radiotherapy, hyperthermia was applied first, then followed by radiation. According to other studies, heat increases the blood flow so that more oxygen can arrive to the tumor, reducing hypoxia. A reduction in the number of hypoxic cells increases the sensitivity of the tumor. As a result, hyperthermia can help to kill radio-resistant cells and in this way plays a critical role in increasing the efficacy of cancer therapy (Hildebrandt et al. 2002; Ma et al. 2016; Thapa et al. 2015).
We used flow cytometry to analyze the percentage of necrotic and apoptotic cells and found that Au@IONPs increased the apoptosis level in cells exposed to a combination of hyperthermia and radiation. Au@IONPs had no impact on the effect of hypothermia alone but potentiated the effect of both 2 and 4 Gy of X-rays given alone. These findings are in agreement with other studies listed in Table 2.
Conclusions
In this study, we synthesized and characterized the Au@IONP nanocomplex and investigated its potential as adjuvant of hyperthermia and radiotherapy in glioma therapy. Our results demonstrated that Au@IONPs potentiate the effect of hyperthermia and radiation suggesting that gold-coated iron oxide nanoparticles in combination with hyperthermia and radiation are a promising factor in treatment of therapy-resistant gliomas.
References
Ban Z, Barnakov YA, Li F, Golub VO, O’Connor CJ (2005) The synthesis of core–shell iron@ gold nanoparticles and their characterization. J Mater Chem 15(43):4660–4662
Bañobre-López M, Teijeiro A, Rivas J (2013) Magnetic nanoparticle-based hyperthermia for cancer treatment. Rep Pract Oncol Radiother 18(6):397–400
Beik J, Abed Z, Ghoreishi FS, Hosseini-Nami S, Mehrzadi S, Shakeri-Zadeh A, Kamrava SK (2016a) Nanotechnology in hyperthermia cancer therapy: From fundamental principles to advanced applications. J Controlled Release 235:205–221
Beik J, Abed Z, Shakeri-Zadeh A, Nourbakhsh M, Shiran MB (2016b) Evaluation of the sonosensitizing properties of nano-graphene oxide in comparison with iron oxide and gold nanoparticles. Physica E 81:308–314
Beik J, Khademi S, Attaran N, Sarkar S, Shakeri-Zadeh A, Ghaznavi H, Ghadiri H (2017) A nanotechnology based strategy to increase the efficiency of cancer diagnosis and therapy: folate conjugated gold nanoparticles. Curr Med Chem 24(39):4399–4416
Butterworth K, Coulter J, Jain S, Forker J, McMahon S, Schettino G, Prise K, Currell F, Hirst D (2010) Evaluation of cytotoxicity and radiation enhancement using 1.9 nm gold particles: potential application for cancer therapy. Nanotechnology 21(29):295101
Butterworth KT, McMahon SJ, Taggart LE, Prise KM (2013) Radiosensitization by gold nanoparticles: effective at megavoltage energies and potential role of oxidative stress. Translational Cancer Research 2(4):269–279
Cabada TF, de Pablo CSL, Serrano AM, del Pozo Guerrero F, Olmedo JJS, Gomez MR (2012) Induction of cell death in a glioblastoma line by hyperthermic therapy based on gold nanorods. Int J Nanomed 7:1511
Cabuy E (2011) Hyperthermia in cancer treatment. Reliab Cancer Ther Energy-Based Ther 1(2):1–48
Chen D, Tang Q, Li X, Zhou X, Zang J, Xue W-q, Xiang J-y, Guo CQ (2012) Biocompatibility of magnetic Fe3O4 nanoparticles and their cytotoxic effect on MCF-7 cells. Int J Nanomed 7:4973
Chicheł A, Skowronek J, Kubaszewska M, Kanikowski M (2007) Hyperthermia–description of a method and a review of clinical applications. Rep Pract Oncol Radiother 12(5):267–275
Esmaelbeygi E, Khoei S, Khoee S, Eynali S (2015) Role of iron oxide core of polymeric nanoparticles in the thermosensitivity of colon cancer cell line HT-29. Int J Hyperth 31(5):489–497
Eyvazzadeh N, Shakeri-Zadeh A, Fekrazad R, Amini E, Ghaznavi H, Kamrava SK (2017) Gold-coated magnetic nanoparticle as a nanotheranostic agent for magnetic resonance imaging and photothermal therapy of cancer. Lasers Med Sci 32(7):1469–1477
Furnari FB, Fenton T, Bachoo RM, Mukasa A, Stommel JM, Stegh A, Hahn WC, Ligon KL, Louis DN, Brennan C (2007) Malignant astrocytic glioma: genetics, biology, and paths to treatment. Genes Dev 21(21):2683–2710
Gao B, Shen L, He K-W, Xiao W-H (2015) GNRs@ SiO2-FA in combination with radiotherapy induces the apoptosis of HepG2 cells by modulating the expression of apoptosis-related proteins. Int J Mol Med 36(5):1282–1290
Gopinath P, Gogoi SK, Sanpui P, Paul A, Chattopadhyay A, Ghosh SS (2010) Signaling gene cascade in silver nanoparticle induced apoptosis. Colloids Surf B 77(2):240–245
Hehr T, Wust P, Bamberg M, Budach W (2003) Current and potential role of thermoradiotherapy for solid tumours. Oncol Res Treat 26(3):295–302
Her S, Jaffray DA, Allen C (2015) Gold nanoparticles for applications in cancer radiotherapy: Mechanisms and recent advancements. Adv Drug Deliv Rev 109:84–101
Hildebrandt B, Wust P, Ahlers O, Dieing A, Sreenivasa G, Kerner T, Felix R, Riess H (2002) The cellular and molecular basis of hyperthermia. Crit Rev Oncol/Hematol 43(1):33–56
Hoopes P, Strawbridge R, Gibson U, Zeng Q, Pierce Z, Savellano M, Tate J, Ogden J, Baker I, Ivkov R (2007) Intratumoral iron oxide nanoparticle hyperthermia and radiation cancer treatment. In: Thermal treatment of tissue: energy delivery and assessment IV. International Society for Optics and Photonics, p 64400K
Hu R, Zheng M, Wu J, Li C, Shen D, Yang D, Li L, Ge M, Chang Z, Dong W (2017) Core-shell magnetic gold nanoparticles for magnetic field-enhanced radio-photothermal therapy in cervical cancer. Nanomaterials 7(5):111
IP Soares P, MM Ferreira I, AGBN Igreja R, MM Novo C, PMR Borges J (2012) Application of hyperthermia for cancer treatment: recent patents review. Recent Pat Anti-Cancer Drug Discov 7(1):64–73
Joh DY, Sun L, Stangl M, Al Zaki A, Murty S, Santoiemma PP, Davis JJ, Baumann BC, Alonso-Basanta M, Bhang D (2013) Selective targeting of brain tumors with gold nanoparticle-induced radiosensitization. PloS One 8(4):e62425
Kang YS, Risbud S, Rabolt JF, Stroeve P (1996) Synthesis and characterization of nanometer-size Fe3O4 and γ-Fe2O3 particles. Chem Mater 8(9):2209–2211
Khoshgard K, Hashemi B, Arbabi A, Rasaee MJ, Soleimani M (2014) Radiosensitization effect of folate-conjugated gold nanoparticles on HeLa cancer cells under orthovoltage superficial radiotherapy techniques. Phys Med Biol 59(9):2249
Li P, Shi Y-w, Li B-x, Xu W-c, Shi Z-l, Zhou C, Fu S (2015) Photo-thermal effect enhances the efficiency of radiotherapy using Arg-Gly-Asp peptides-conjugated gold nanorods that target αvβ3 in melanoma cancer cells. J Nanobiotechnol 13(1):52
Li S, Penninckx S, Karmani L, Heuskin A-C, Watillon K, Marega R, Zola J, Corvaglia V, Genard G, Gallez B (2016) LET-dependent radiosensitization effects of gold nanoparticles for proton irradiation. Nanotechnology 27(45):455101
Lyon JL, Fleming DA, Stone MB, Schiffer P, Williams ME (2004) Synthesis of Fe oxide core/Au shell nanoparticles by iterative hydroxylamine seeding. Nano Lett 4(4):719–723
Ma N, Jiang Y-W, Zhang X, Wu H, Myers JN, Liu P, Jin H, Gu N, He N, Wu F-G (2016) Enhanced radiosensitization of gold nanospikes via hyperthermia in combined cancer radiation and photothermal therapy. ACS Appl Mater Interfaces 8(42):28480–28494
Maeda H, Bharate G, Daruwalla J (2009) Polymeric drugs for efficient tumor-targeted drug delivery based on EPR-effect. Eur J Pharm Biopharm 71(3):409–419
Mahdavi SR, Yahyapour R, Nikoofar A (2016) Cytotoxic effects of hyperthermia, chemotherapy (Navelbine) and radiation on glioma spheroids. Radiat Phys Chem 123:20–24
Manjili HK, Naderi-Manesh H, Mashhadikhan M, Ma’mani L, Nikzad S (2014) The effect of iron-gold core shell magnetic nanoparticles on the sensitization of breast cancer cells to irradiation. J Paramed Sci 5(2):85–90
Mateo D, Morales P, Ávalos A, Haza AI (2014) Oxidative stress contributes to gold nanoparticle-induced cytotoxicity in human tumor cells. Toxicol Mech Methods 24(3):161–172
McMahon SJ, Hyland WB, Muir MF, Coulter JA, Jain S, Butterworth KT, Schettino G, Dickson GR, Hounsell AR, O’sullivan JM (2011) Biological consequences of nanoscale energy deposition near irradiated heavy atom nanoparticles. Sci Rep 1:18
Mirrahimi M, Hosseini V, Kamrava SK, Attaran N, Beik J, Kooranifar S, Ghaznavi H, Shakeri-Zadeh A (2017) Selective heat generation in cancer cells using a combination of 808 nm laser irradiation and the folate-conjugated Fe2O3@ Au nanocomplex. Artif Cells Nanomed Biotechnol. https://doi.org/10.1080/21691401.2017.1420072
Miyake K, Shimada M, Nishioka M, Sugimoto K, Batmunkh E, Uto Y, Nagasawa H, Hori H (2008) The novel hypoxic cell radiosensitizer, TX-1877 has antitumor activity through suppression of angiogenesis and inhibits liver metastasis on xenograft model of pancreatic cancer. Cancer Lett 272(2):325–335
Park H-Y, Schadt MJ, Wang L, Lim I-IS, Njoki PN, Kim SH, Jang M-Y, Luo J, Zhong C-J (2007) Fabrication of magnetic core@ shell Fe oxide@ Au nanoparticles for interfacial bioactivity and bio-separation. Langmuir 23(17):9050–9056
Samadian H, Hosseini-Nami S, Kamrava SK, Ghaznavi H, Shakeri-Zadeh A (2016) Folate-conjugated gold nanoparticle as a new nanoplatform for targeted cancer therapy. J Cancer Res Clin Oncol 142(11):2217–2229
Sicard-Roselli C, Brun E, Gilles M, Baldacchino G, Kelsey C, McQuaid H, Polin C, Wardlow N, Currell F (2014) A new mechanism for hydroxyl radical production in irradiated nanoparticle solutions. Small 10(16):3338–3346
Silva AC, Oliveira TR, Mamani JB, Malheiros SM, Malavolta L, Pavon LF, Sibov TT, Amaro E Jr, Tannus A, Vidoto EL (2011) Application of hyperthermia induced by superparamagnetic iron oxide nanoparticles in glioma treatment. Int J Nanomed 6:591
Sudhakar A (2009) History of cancer, ancient and modern treatment methods. J Cancer Sci Therapy 1(2):1
Sun J, Guo M, Pang H, Qi J, Zhang J, Ge Y (2013) Treatment of malignant glioma using hyperthermia. Neural Regener Res 8(29):2775
Thapa R, Galoforo S, Kandel SM, El-dakdouki MH, Wilson TG, Huang X, Roth BJ, Wilson GD (2015) Radiosensitizing and hyperthermic properties of hyaluronan conjugated, dextran-coated ferric oxide nanoparticles: implications for cancer stem cell therapy. J Nanomater 16(1):400
Van der Zee J (2002) Heating the patient: a promising approach? Ann Oncol 13(8):1173–1184
Verma J, Lal S, Van Noorden CJ (2014) Nanoparticles for hyperthermic therapy: synthesis strategies and applications in glioblastoma. Int J Nanomed 9:2863
Wahab R, Dwivedi S, Khan F, Mishra YK, Hwang I, Shin H-S, Musarrat J, Al-Khedhairy AA (2014) Statistical analysis of gold nanoparticle-induced oxidative stress and apoptosis in myoblast (C2C12) cells. Colloids Surf B 123:664–672
Wang C, Jiang Y, Li X, Hu L (2015) Thioglucose-bound gold nanoparticles increase the radiosensitivity of a triple-negative breast cancer cell line (MDA-MB-231). Breast Cancer 22(4):413–420
Witteles RM (2011) Radiation therapy for breast cancer. J Am Coll Cardiol 57(4):453–454
Yi X, Chen L, Zhong X, Gao R, Qian Y, Wu F, Song G, Chai Z, Liu Z, Yang K (2016) Core–shell Au@ MnO2 nanoparticles for enhanced radiotherapy via improving the tumor oxygenation. Nano Res 9(11):3267–3278
Zhang A-w, Guo W-h, Qi Y-f, Wang J-z, Ma X-x, Yu DX (2016) Synergistic effects of gold nanocages in hyperthermia and radiotherapy treatment. Nanoscale Res Lett 11(1):279
Zhou J, Wang X, Du L, Zhao L, Lei F, OuYang W, Zhang Y, Liao Y, Tang J (2011) Effect of hyperthermia on the apoptosis and proliferation of CaSki cells. Mol Med Rep 4(1):187–191
Funding
This study was conducted with financial and instrumental supports received from IUMS and ZaUMS.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
A. Neshasteriz declares that he has no conflict of interest. Z. Khosravi declares that she has no conflict of interest. H. Ghaznavi and A. Shakeri-Zadeh declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Neshastehriz, A., Khosravi, Z., Ghaznavi, H. et al. Gold-coated iron oxide nanoparticles trigger apoptosis in the process of thermo-radiotherapy of U87-MG human glioma cells. Radiat Environ Biophys 57, 405–418 (2018). https://doi.org/10.1007/s00411-018-0754-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-018-0754-5