Abstract
Lung cancer mortality in the period of 1948–2002 has been analysed for 6,293 male workers of the Mayak Production Association, for whose information on smoking, annual external doses and annual lung doses due to plutonium exposures was available. Individual likelihoods were maximized for the two-stage clonal expansion (TSCE) model of carcinogenesis and for an empirical risk model. Possible detrimental and protective bystander effects on mutation and malignant transformation rates were taken into account in the TSCE model. Criteria for non-nested models were used to evaluate the quality of fit. Data were found to be incompatible with the model including a detrimental bystander effect. The model with a protective bystander effect did not improve the quality of fit over models without a bystander effect. The preferred TSCE model was sub-multiplicative in the risks due to smoking and internal radiation, and more than additive. Smoking contributed 57% to the lung cancer deaths, the interaction of smoking and radiation 27%, radiation 10%, and others cause 6%. An assessment of the relative biological effectiveness of plutonium was consistent with the ICRP recommended value of 20. At age 60 years, the excess relative risk (ERR) per lung dose was 0.20 (95% CI: 0.13; 0.40) Sv−1, while the excess absolute risk (EAR) per lung dose was 3.2 (2.0; 6.2) per 104 PY Sv. With increasing age attained the ERR decreased and the EAR increased. In contrast to the atomic bomb survivors, a significant elevated lung cancer risk was also found for age attained younger than 55 years. For cumulative lung doses below 5 Sv, the excess risk depended linearly on dose. The excess relative risk was significantly lower in the TSCE model for ages attained younger than 55 than that in the empirical model. This reflects a model uncertainty in the results, which is not expressed by the standard statistical uncertainty bands.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Empirical risk models in radiation epidemiology reflect radiobiological processes by simple linear or quadratic dose responses, possibly modified by an exponential term. For example, a damage caused by one hit to a cell is assumed to be associated with a linear term, one caused by two hits with a quadratic term, and an effect caused by cell killing with an exponential term. During the last two decades, however, the situation has become increasingly complicated by the discovery of nonlinear inter-cellular effects in the low-dose responses of various biological indicators of cellular damage.
It is by no means clear how such nonlinear effects should be accounted for in empirical risk models [1]. Models of carcinogenesis, however, provide a useful approach for helping to shed some light on these issues [2]. Dose-response characteristics of inter-cellular radiation effects can be integrated in the equations of such models in a straightforward way. Nonlinear effects on mutations, e.g., influence the conversion rates between different stages of cells during the development to a cancer cell. Nonlinear cell inactivation effects influence the number of cells at the different stages. Within the framework of the two-stage clonal expansion (TSCE) model for carcinogenesis [3, 4], it has been shown that accounting for radiation-induced inactivation of intermediate cells improves the modelling of the age-at-exposure dependence on lung cancer incidence among the atomic bomb survivors [5]. If low-dose hypersensitivity exists in the inactivation of cells involved in the development of human lung cancer, then the model predicts a downward curvature of the dose response at low doses for older ages at exposure.
Radiation-induced bystander effects are an important phenomenon of inter-cellular communication. Bystander effects are caused by the ability of irradiated cells to convey manifestations of damage to non-irradiated cells [6]. Bystander effects are characterized by saturation at higher doses. Among many other biological endpoints, mutations may be caused in bystander (non-irradiated) cells as first observed by Nagasawa and Little [7] in experiments with low fluences of alpha radiation. The mutational bystander effect has been confirmed in experiments with microbeams of alpha particles [8].
One aim of this article is to investigate whether possible consequences of mutational bystander effects of alpha radiation can be detected in an epidemiological data set. Alpha radiation from inhaled plutonium forms the main contribution to the lung dose of workers of the Mayak Production Association. Therefore, this cohort has been analysed in the present work with versions of the TSCE model that take bystander effects into account.
The Mayak Production Association began operation in 1948 and included nuclear reactors, a plant for radiochemical separation of plutonium from irradiated nuclear fuel, and a plutonium production plant. Lung cancer mortality among Mayak workers has been analysed with empirical models, in which the relative risks due to smoking and plutonium exposure were assumed to be multiplicative [9–11]. An analysis of the data with a TSCE model version, in which the interaction of smoking and plutonium exposure was sub-multiplicative, resulted in significantly lower estimates of the excess relative risk per dose than the analyses with multiplicative models [12, 13]. In the present work, empirical and TSCE model versions to lung cancer mortality among Mayak workers are analysed on the basis of the same statistical procedures, in order to further explore the discrepancies in estimated risk values. Quality of fit criteria for non-nested models [14] are applied for a comparison of the different models.
Materials and methods
Description of the data
The dosimetry of the Mayak workers has been described in previous publications (see e.g. [12, 13]). In brief, external exposures were mainly due to photons. The reactor workers had also small dose contributions from neutrons. Neutron ambient dose equivalents were derived from neutron and photon spectra calculated for different work areas, photon ambient dose equivalents measured for the workers with film and TLD dosimeters, and ICRP-60 radiation-weighting factors. Internal lung doses were mainly due to the inhalation of plutonium. Calculations were based on the ICRP-66 lung clearance model [15] with a modification accounting for a fixation depot [16], and on the ICRP-67 biokinetic model for systemic plutonium [17] with an adaptation to Mayak data [18]. Doses were calculated under the assumption of a homogeneous lung tissue.
The cohort was defined by the following criteria: male; first employment at Mayak in the period of 1948–1972; work place in one of the reactors, or in the radiochemical or plutonium production plant; measurement of external dose available; if worker of the radiochemical or plutonium production plant, then the assessment of internal lung dose based on urine measurement available; at least 2 years survival after the first measurement of α-activity in the urine; smoking information available.
The cohort included 6,293 workers. The follow-up used in the analysis started either with the date of hire, or, if the α-activity in the urine was measured, 2 years after the first urine measurement. The follow-up period extended to 31 December 2002. The vital status is known for 6,093 workers (96.8%). For the remaining 200 workers follow-up until the last date of information on vital status was included in the analysis.
In total, there were 3,039 deaths, the cause of death is known for 2,961 cases (97.4%). The remaining 78 workers were treated in the analysis as if they had died from another cause than lung cancer. In total, there were 301 deaths with lung cancer as the primary cause of death (Table 1), only 10 of them occurred among non-smokers.
Smoking rates were about the same in all three plants. The highest contribution of lung cancer to the total death toll (13.2%) was found among workers in the plutonium production plant, who also received the highest lung doses due to plutonium exposure (7.4 Sv on average). Their external dose, however, was relatively small (0.3 Sv on average). The highest external exposures occurred among the workers of the radiochemical plant with a mean value of 1.2 Sv.
For 3,582 workers (56.9%), there was a suspicion of possible plutonium incorporation. For them the plutonium content in the urine has been measured and resulting lung doses have been assessed. Their average internal lung dose was 4.3 Sv, with a median of 0.8 Sv and a 95% range of 0.0–32.6 Sv. The cohort included 137 reactor workers, who also worked at work places with a potential of exposure to plutonium. Their average internal lung dose was 0.6 Sv, with a median of 0.3 Sv and a 95% range of 0–3.9 Sv.
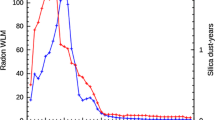
In Fig. 1, the temporal development of the internal lung dose during follow-up is presented for 10 arbitrarily chosen workers. Some workers show a relatively high uptake in the first few years of employment, followed by a lower uptake in the subsequent years. For these workers, the annual lung dose reduces within 5 years from the peak value by a factor of 5 or more. Other workers (mainly after 1956) show a more constant uptake, resulting in an annual lung dose, which increases continuously with a decreasing slope (one example in the lower panel of Fig. 1). For most of the workers, the temporal development of the annual lung doses is intermediate to these two scenarios: A peak of the lung dose in the first years with a half width of about one decade is followed by a slow drop off.
In general, there is no correlation between internal lung doses and external ambient dose equivalents in the cohort. Most of the reactor workers had no internal lung doses and considerable ambient dose equivalents due to external radiation. For 2,815 workers the cumulated internal lung dose and the cumulated ambient dose equivalent due to external radiation exceeded 0.001 Sv (Fig. 2, upper panel). The correlation coefficient between external and internal doses was 0.075. Most of these workers had internal lung doses in the range of 0.1–100 Sv, and ambient dose equivalents due to external radiation in the range of 0.01–5 Sv. Thus, internal lung doses are in this group by one order of magnitude larger than ambient dose equivalents due to external radiation. The distribution of doses of those workers who died of lung cancer (Fig. 2, lower panel) covers the same range. Relatively more of these workers, however, are found in the area of higher doses.
TSCE models for carcinogenesis
The TSCE model is a very simplified description of the process of carcinogenesis. It has already been described in previous publications [e.g., 12, 13]. In brief, it is assumed that healthy cells in the lung convert with an initiation rate ν(t), where t is the age of the worker, to intermediate cells of the carcinogenic process. Intermediate cells divide with a rate α(t) and differentiate or are inactivated with a rate β(t). A malignant conversion rate μ(t) characterizes the complex transformation of an intermediate cell to a malignant cell. Once a malignant cell has been produced, it is assumed to lead to death of the worker due to lung cancer within a given lag time (t lag).
The following model parameter combinations were assumed to be constant for every year j from birth up to the end of follow-up
where N s is the number of healthy susceptible cells. The parameter μ 0 has no influence on the mortality rate and thus cannot be determined from the data [19].
As in a previous analysis [12, 13], in none of the preferred models a dependence of μ on smoking or radiation exposures was found to improve the fit significantly.
Let s be the smoking status (0 if not smoking, 1 if smoking). All workers, who had smoked, were assumed to have started smoking at age 18. Calculations with an age of 15 or 20 years at the beginning of smoking gave similar results.
Let d ext,j and d int,j be the annual external and internal doses in the jth year of exposure, respectively. The first model considered here, the TSCEa model, is the preferred model (Model 1) of a previous work [12, 13]. In contrast, however, a birth-year effect modifier was not considered in the present work, because such a term did not improve the quality of fit for the extended cohort:
where X e, X d , γ 0, γ sm, γ lev, γ d , and q e are fit parameters.
The TSCEb model is the preferred model of the present work:
where q d and r are the additional fit parameters.
For simplicity, it is assumed in the TSCEb model that the relative biological effectiveness of the alpha particles emitted by the plutonium in the lung, 20 r, is independent of dose, and is the same in all biological processes considered. Likelihood ratio tests showed that all parameters in the TSCEb model give a significant improvement of the quality of fit.
The bystander effect was assumed to influence the parameter X, which is proportional to the product of the effective initiation and malignant conversion rates in the model. The preferred model with a protective bystander effect was defined by
where X int and X pint are fit parameters.
The preferred model with a detrimental bystander effect was defined by
where X dlev and X dint are fit parameters.
Empirical model
The baseline hazard, h b, was modelled as a function of attained age and smoking status:
The total hazard, h, was modelled by
where c 0, c 1, c 2, c 3, c sm, c ext and c int are fit parameters, D ext(t) and D int(t) are the external and internal doses cumulated from begin of exposure until age t, and t lag is the lag time. Most of the analyses have been performed for a lag time of 10 years, because slightly better fits (Δ in deviance = 1.3) were obtained than with a lag time of 5 years, as used by Kreisheimer et al. [10] and Gilbert et al. [11] (see below).
Likelihood construction and quality of fit
Statistical procedures to maximize the product of the likelihood for the individual data have been described elsewhere [12, 13]. The empirical model was also fitted by Poisson regressions with AMFIT in the software package EPICURE.Footnote 1
Convergence problems occurred in fitting the parameter t lag. Therefore, a pre-analysis with the TSCEa model was performed with fixed lag times, which were varied in steps of 5 years. The deviance was nearly constant for a wide range of values of t lag with minimum values in the range of 10 and 15 years. A fixed value for t lag of 10 years was therefore used in all further calculations.
For estimating the quality of fit of non-nested models, two criteria AIC and BIC are used in the present work (see [14] for a review). Based on the information theory, Akaike [20] proposed to choose the model for which the Akaike information criterion (AIC; see Eq. 8) is the smallest:
where dev is the deviance and k is the number of fit parameters.
A model A is considered to be an improvement over another model B with 95% probability, if AIC for model A is by six less than AIC for model B.
On the basis of Bayesian theory, Schwarz [21] arrived at the procedure of choosing the model for which the Bayes information criterion (BIC, see Eq. 9) is the smallest:
where n is the number of workers (6,293), in the present application.
Evidence for a model improvement is considered to be strong, if the difference in BIC values of two models is larger than six.
In contrast to the empirical model, in the TSCE model the excess relative risk (ERR) per dose is not a direct fit parameter. The ERR per lung dose, δ i (t), for the exposure history of an exposed cohort member i is defined here by
The average of the ERR per dose of those exposed cohort members included in the follow-up with age t, is compared with the results of the empirical ERR models. Procedures to calculate uncertainty bands have been described elsewhere [12, 13].
Results
Quality of fit
According to AIC, the data are best fitted by the TSCEb model (Table 2), and are also fitted quite well by the TSCE model with a protective bystander effect (ΔAIC = 4.9). The TSCEb model fits the data significantly better than the remaining three models. According to BIC, the data are best fitted by the TSCEa model, and are fitted similarly well by the empirical model (ΔBIC = 1.3). The data are also fitted quite well by the TSCE model with a protective bystander effect (ΔBIC = 5.4). There is strong evidence against the two remaining models. In summary, the TSCE model with a detrimental bystander effects is ruled out by both criteria for choosing the best model from a group of non-nested models. The criteria do not give a strong preference for any one of the other four models.
The number of fatal lung cancer cases observed in different age-attained and dose subgroups of the cohort is predicted equally well by the TSCEa, TSCEb and empirical models (results not shown). For the number of fatal lung cancer cases observed in different age-at-hire and dose subgroups of the cohort, however, there is a tendency for a better prediction by the TSCEb model than by the TSCEa and the empirical models (Table 3).
Fit parameters
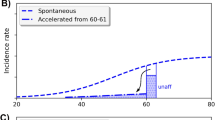
In the TSCE models without bystander effect, the spontaneous value of X, the product of the number of healthy cells, the initiation rate and the malignant conversion rate, is doubled by a dose rate of about 0.08 Sv year−1 (Fig. 3). Since the radiation does not act in the preferred models on the number of healthy cells and on the malignant conversion rate, the effect on X corresponds to an effect on the initiation rate.
In the preferred model with a protective bystander effect, there is a considerable reduction of the radiation effect on the initiation rate in the range of annual internal lung doses below 0.2 Sv (Fig. 3). For higher annual doses, however, there is a stronger effect than in the models without a bystander effect.
The baseline rate, γ 0 + γ sm, of the clonal growth of the number of intermediate cells is about 0.14 year−1 (Table 4). Although there is clear significance of a levelling in the dose dependence of γ, the levelling does not occur before quite high dose rates.
In the TSCEb model, the factor r which modifies an assumed value of 20 for the radiobiological effectiveness of plutonium has a best estimate of 0.76 with a large 95% confidence range (0.29; 5.58).
Values of fit parameters in the empirical models with lag times of 5 and 10 years agreed in general to within 3%. Exceptions are the ERR per internal lung dose, c int, and the exponent of the age dependence of the ERR, c 3. In the model with the longer lag time, the dose considered to be associated with lung cancer death is smaller. Correspondingly, the estimate of the ERR per lung dose is larger (see below).
Poisson regression of the empirical model gave results for the fit parameters similar to the regression based on individual likelihoods. The largest difference was obtained for the parameter c 3, for which the result of the regression with individual data was lower than the result of the Poisson regression by 8%.
Causes of fatal lung cancer
The TSCE models and the empirical model agree on a low contribution of spontaneous cases of about 8% to all lung cancer fatalities (Fig. 4). The main factor is smoking (about 60% in the TSCE models and about 50% in the empirical model). The models are more than additive in the excess absolute risks of smoking and internal radiation. The interaction contributes to the total number of lung cancer fatalities about 15% in the TSCE models and about 20% in the empirical model. Radiation alone is related to about 10 and 5% of the cases according to the TSCE models, and the empirical model, respectively.
The empirical model is by construction multiplicative in the relative risks. The ratio of cases associated with interaction of smoking and internal radiation and of the sum of cases associated with the two single exposures is 0.40 (0.26; 0.55). This ratio is 0.21 (0.14; 0.30) in the TSCEa model, and 0.24 (0.17; 0.38) in the TSCEb model. These values are significantly lower than those in the empirical model (P < 0.013 and P < 0.035, respectively). Thus, the TSCE models are sub-multiplicative in the relative risks due to smoking and due to plutonium exposure.
Excess relative risk in the cohort
Table 5 gives risk estimates for male Mayak workers at age 60. All three models agree on an excess relative risk due to smoking of about 10. The uncertainty ranges are, however, large due to the small number of lung cancer fatalities among non-smokers.
The ERR per plutonium dose in the lung at age 60 has a value of 0.20 (0.13; 0.40) Sv−1 in the TSCEb model compared with 0.27 (0.18; 0.39) Sv−1 in the empirical model. Thus, the two estimates agree within their uncertainty limits. The TSCEa model, however, results in an estimate of the ERR per lung dose, which is significantly smaller than in the estimate of the empirical model (P < 0.008). The difference is related to a small over-prediction of the cases by the empirical model (for age group 50–70 and internal dose 1–5 Sv, e.g., 70.5 cases predicted versus 67 observed) and a small under-prediction by the TSCEa model (60.4 cases predicted). Differences in the modelling of the baseline rate play a minor role. For all dose groups, the TSCEb model predictions are closer to the number of observed cases in the age group 50–70 than the predictions of the other two models.
Reducing the lag time in the empirical model from 10 to 5 years causes a 10% decrease of the estimate for the excess relative risk per internal dose.
The estimate of the ERR per external dose has a large uncertainty in the TSCEb model. In the TSCEa model and in the empirical model, it is even at the borderline of being significant.
Excess relative risk for hypothetical exposure patterns
At cumulated internal doses below 5 Sv, the ERR depends linearly on dose in all three models (Fig. 5). Thus, in this range the complex dependence of the risk on radiation dose can be described by a linear approximation of the model solution.
In the low-dose range, the TSCEb model exhibits a direct dose rate effect: the ERR per dose is smaller for longer lasting exposures. In both TSCE models, the ERR has only a moderate dependence on attained age. For young attained age, the ERR is considerably smaller in the TSCE models than in the empirical model.
At higher doses, the ERR dependence on dose is quite complex in the TSCE models, and there is an indirect dose rate effect.
In general, there is only a modest dependence of the ERR per dose on age at hire (results not shown).
Excess absolute risk
The excess absolute risk (EAR) per dose increases with increasing age attained up to 70, and remains then on a constant level of about seven cases per 104 PY Sv (Table 6). The three models agree within the uncertainty limits on their prediction of the EAR per dose for age attained 70 and older. For age attained 60 and younger, however, the TSCEa model gives a significantly lower result than the empirical model. The TSCEb model gives an intermediate result. Again, these differences are related to relatively small differences in the calculated hazards, where the TSCEb models reproduces the observed number of cases in the attained age range 50–70 best. Effect modifications to the EAR by dose, exposure time and age at hire are similar to those for the ERR.
Discussion
Parameters of the TSCE model
In the present analysis, the best estimate of the baseline growth rate, γ 0 + γ sm, of the number of intermediate cells is about 0.14 year−1. This value is in full agreement with a rate of 0.14 year−1 as derived from lung cancer mortality data of smoking Colorado plateau miners [22], and with a rate of 0.17 year−1 as derived from lung cancer incidence rates among male atomic bomb survivors [5].
The growth rate, γ, of the number of intermediate cells increases in the TSCE models with dose rate. This increase is exponentially weakening at higher dose rates. Such dose dependence is an approximation of a dose response in TSCE models, in which radiation-induced cell killing effects on the number of intermediate cells are taken into account [23]. A weakening dose effect on the growth rate of intermediate cells has also been found in the analyses of lung cancer of the Colorado Plateau miners [22]. If the dose dependence of the growth rate is rescaled according to the ICRP [24] dose conventionFootnote 2, then there is a very good agreement with the present analysis for the Mayak workers (Fig. 6).
Growth rate of the number of intermediate cells as a function of annual lung dose of smokers as derived for male Mayak workers (TSCEa and TSCEb model) and for Colorado miners [22]
For fixed values of X 0, γ 0 and q 0, a positive value of γ 0 implies that μ 0 < q 0 (see Appendix). Thus, the upper confidence bound −8.8 of q e (Table 4) implies an upper bound of the spontaneous malignant transformation rate μ 0 of 1.5 × 10−4 a−1. This value is consistent with the range of upper bounds (3 × 10−6–1 × 10−4 a−1) as derived within the framework of the TSCE model for lung cancer in other cohorts [25].
Other model parameters have large uncertainties. Within their uncertainty bands the parameter estimates are also consistent with previous analyses.
In summary, the analyses of epidemiological data sets with the TSCE model are beginning to provide consistent predictions of the biological parameters needed to describe intermediate cells in the process of carcinogenesis. In the case of lung cancer, candidates of clones of intermediate cells are preneoplastic lesions in the bronchial epithelium, which are characterized by multiple, discrete, 3p loss-of-heterozygosity sites [26]. It might thus become possible to test characteristics of cells in preneoplastic lesions experimentally, which are predicted by TSCE model analyses of epidemiological data. Indeed, an effect of alpha radiation exposure has already been detected in an animal experiment on the initiation and growth of foci of altered hepatocytes, which are considered to be preneoplastic lesions [27].
Lag time
In the present analysis, a lag time of 10 years describes the data somewhat better than other lag times. This result is close to the value of 9 years found in an analysis of the Colorado miners [22]. A lag time of about 10 years is intermediate to values used previously in the analyses of lung cancer mortality among Mayak workers with empirical models: Kreisheimer et al. [10] and Gilbert et al. [11] used a lag time of 5 years, Sokolnikov et al. [28] used a lag time of 20 years. Although the lag times in the TSCE model and in the empirical model have a different definition (see footnote to Table 5), their influence on modelling mortality rates is similar.
Excess relative risk
The confidence intervals given here are formal confidence intervals as obtained in the regression analyses. Estimates of lung doses, especially due to the incorporation of plutonium, however, have a large uncertainty. It was not possible to take these dose uncertainties into account in the present analysis. Further, only the smoking status (yes or no) and not smoking rates were known, introducing another source of uncertainty. Thus, full confidence intervals of the risk estimates could be substantially larger then those given here.
The best estimate for the excess relative risk due to smoking among Mayak workers (Table 5) is higher in the TSCEb model (13) than in the other two models and in previous analyses (8–10). The result of the TSCEb model is closer but still by a factor of 2 lower than the result of 25.8 (21.3; 31.2) of the European pooling study on indoor radon [29]. The results for the Mayak workers on smoking risk are limited because smoking rates are not known.
The ERR per internal lung dose in a previous analysis of the lung cancer mortality among the Mayak workers with a model of carcinogenesis [12, 13] was significantly lower than results obtained by Gilbert et al. [11] with an empirical model. The TSCEa model of the present analysis is very similar to the preferred model (Model 1) in Jacob et al. [12, 13]. Possibly due to the extension of the cohort and the follow-up, the estimate of the ERR per lung dose with the TSCEa model in the present analysis is higher than the result of Model 1 in the previous analysis by 30%. Nevertheless, the result is still significantly smaller than that of the empirical model with the same lag time (P < 0.01). The TSCEb model is more sophisticated than the TSCEa model. The result obtained with the TSCEb model for the ERR per internal lung dose is closer to the results of the empirical models. There is no statistically significant difference in the central estimate of the ERR per lung dose. Nevertheless, there are considerable differences in other results for the ERR per lung dose:
-
For low doses and for young attained age, the ERR per lung dose in the TSCE models is smaller than that in the empirical model
-
For high doses, the ERR per lung dose has in the TSCE models a nonlinear dependence which resembles a quadratic increase with dose, followed by an exponential decrease. In the empirical model, no significant deviation from a linear dose dependence was found.
At the current state, these differences are to be considered as model uncertainties.
Many of the members of the cohort studied in this article were hired at age around 20 and had protracted exposures, which were decreasing with age. In an analysis of the lung cancer mortality in the period 1950–1997 for the Japanese atomic bomb survivors [30], the ERR per unit dose for males with exposures at age 30 was 0.48 (90% CI: 0.23; 0.78) Sv−1. Gilbert et al. [11] analysed lung cancer mortality among the Japanese bomb survivors with age at exposure 15 to 60 and obtained an ERR per dose of 0.40 (95% CI: 0.032; 0.86) Sv−1. These two values for the atomic bomb survivors are consistent with each other. The first assessment has a smaller statistical uncertainty. It is significantly higher than risks obtained in most of the analyses of the Mayak workers for plutonium exposure under the assumption of a radiation-weighting factor of 20 for plutonium (Table 5).
Best estimates of the ERR per external dose in the present analysis are about one order of magnitude larger than the best estimates in previous studies (Table 5). The reason may be the longer follow-up and the extended number of cohort members. The best estimates of the ERR per external dose are now considerably closer to those observed among the atomic bomb survivors.
Excess absolute risk
Under the assumption of a radiation-weighting factor of 20 for plutonium, central estimates of the EAR per dose for Mayak workers and for atomic bomb survivors are similar (Table 6). However, in contrast to the atomic bomb survivors, there is a significant excess risk among the Mayak workers for age attained smaller than 55.
For age attained larger than 75, Gilbert et al. [11] found a significantly lower EAR per dose for the Mayak workers than for the atomic bomb survivors. According to the present analysis, however, EAR per dose values for both cohorts are consistent in this age group, which is possibly due to the extended follow-up period and the increased number of cohort members in the present analysis.
Relative biological effectiveness of plutonium
The estimate of the parameter r in the TSCEb model may be considered as an estimate of the relative biological effectiveness (RBE) of plutonium under the assumption that the RBE is the same for all relevant processes in the radiation induced carcinogenesis. The result in Table 4 corresponds to an estimate of the RBE of 15 (6; 112). A similar analysis with the empirical model resulted in an estimate for the RBE of 22 (9; 81). Gilbert et al. [11] obtained for male and female Mayak workers a value of 33 (14; 98). If that analysis would have been performed for males alone, the result might have been a bit smaller.
All three analyses are consistent within their large uncertainty ranges. Further, compared with their large uncertainties, the best estimates are quite close to the value of 20, which has been recommended by ICRP. This finding is also supported by the above comparison of ERR and EAR per dose values among the Mayak workers and the atomic bomb survivors.
Notes
Hirosoft International Corporation, Seattle, WA, USA.
For the rescaling it is assumed that 1 working level month corresponds to 0.005 Sv effective dose or 0.04 Sv lung dose.
References
Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, Lubin JH, Preston DL, Preston RJ, Puskin JS, Ron E, Sachs RK, Samet JM, Setlow RB, Zaider M (2003) Cancer risk attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci 100:13761–13766
Sachs RK, Chan M, Hlatky L, Hahnfeldt P (2005) Modeling intercellular interactions during carcinogenesis. Radiat Res 164:324–331
Moolgavkar SH, Venzon DJ (1979) Two-events models for carcinogenesis: incidence curves for childhood and adult tumors. Math Biosci 47:55–77
Moolgavkar S, Knudson A (1981) Mutation and cancer: a model for human carcinogenesis. J Natl Cancer Inst 66:1037–1052
Jacob V, Jacob P (2004) Modelling of carcinogenesis and low-dose hypersensitivity: an application to lung cancer incidence among atomic bomb survivors. Radiat Environ Biophys 42:265–273
Coates PJ, Lorimore SA, Wright EG (2004) Damaging and protective cell signalling in the untargeted effects of ionizing radiation. Mutat Res 568:5–20
Nagasawa H, Little B (1999) Unexpected sensitivity to the induction of mutations by very low doses of alpha particle radiation: evidence for a bystander effect. Radiat Res 54:552–557
Zhou HG, Randers-Pehrson G, Waldren CA, Vannais D, Hall EJ, Hei TK (2000) Induction of a bystander mutagenic effect of alpha particles in mamalian cells. Proc Natl Acad Sci 97:2099–2104
Koshurnikova NA, Bolotnikova MG, Ilyin LA, Keirim-Markus IB, Menshikh ZS, Okatenko PV, Romanov SA, Tcvetkov VI, Shilnikova NS (1998) Lung cancer risk due to exposure to incorporated plutonium. Radiat Res 149:366–371
Kreisheimer M, Sokolnikov ME, Koshurnikova NA, Khokhryakov VF, Romanow SA, Shilnikova NS, Okatenko PV, Nekolla EA, Kellerer AM (2003) Lung cancer mortality among nuclear workers of the Mayak facilities in the former Soviet Union. Radiat Environ Biophys 42:129–135
Gilbert ES, Koshurnikova NA, Sokolnikov ME, Shilnikova NS, Preston DL, Ron E, Okatenko PV, Khokhryakov VF, Vasilenko EK, Miller S, Eckerman K, Romanov SA (2004) Lung cancer in Mayak workers. Radiat Res 162:505–515
Jacob V, Jacob P, Meckbach R, Romanov SA, Vasilenko EK (2005) Lung cancer in Mayak workers: interaction of smoking and plutonium exposure. Radiat Environ Biophys 44:119–129
Jacob V, Jacob P, Meckbach R, Romanov SA, Vasilenko EK (2006) Lung cancer in Mayak workers: interaction of smoking and plutonium exposure. Radiat Environ Biophys 44:307 (Erratum)
Walsh L (2007) A short review of model selection techniques for radiation epidemiology. Radiat Environ Biophys. doi:10.1007/s00411–007–0109–0
ICRP Publication 66 (1994) Human respiratory tract model for radiological protection. Ann ICRP 24(1–3):1–482
Khokhryakov VF, Suslova KG, Vostrotin VV, Romanov SA, Eckerman KF, Krahenbuhl MP, Miller SC (2005) Adaptation of the ICRP publication 66 respiratory tract model to data on plutonium biokinetics for Mayak workers. Health Phys 2:125–132
ICRP Publication 67 (1994) Age-dependent doses to members of the public from intake of radionuclides: Part 2. Ingestion dose coefficients. Ann ICRP 23(3–4):1–167
Leggett RW, Eckerman KF, Khokhryakov VF, Suslova KG, Krahenbuhl MP, Miller SC (2005) Mayak worker study: an improved biokinetic model for reconstructing doses from internally deposited plutonium. Radiat Res 164:111–122
Heidenreich WF, Jacob P, Paretzke HG (1997) Exact solutions of the clonal expansion model and their application to the incidence of solid tumors of atomic bomb survivors. Radiat Environ Biophys 36:45–58
Akaike H (1973) Information theory and an extension of the maximum likelihood principle. In: Petrov and BN, Caski F (eds) Proceedings of the 2nd international symposium on information theory. Budapest, Hungary, Akademiai Kiado, pp 267–281
Schwarz G (1978) Estimating the dimension of a model. Ann Stat 6:461–464
Luebeck AG, Heidenreich WF, Hazelton WD, Paretzke HG, Moolgavkar SH (1999) Biologically based analysis of the data for the Colorado uranium miners cohort: age, dose and dose-rate effects. Radiat Res 152:339–351
Jacob P, Walsh L, Eidemüller M (2007) Modelling of carcinogenesis and cell killing in the atomic bomb survivors with applications to the mortality from all solid, stomach and liver cancers. (submitted)
ICRP Publication 60 (1992) 1990 Recommendations of the international commission on radiological protection. Ann ICRP 21(1–3):1–201
Jacob P, Jacob V (2003) Biological parameters for lung cancer in mathematical models of carcinogenesis. Radiat Prot Dosim 104:357–366
Wistuba II, Behrens C, Virmani AK, Mele G, Milchgrub S, Girard L, Fondon JW, Garner HR, McKay B, Latif F, Lerman MI, Lam S, Gazdar AF, Minna JD (2000) High resolution chromosome 3p allelotyping of human lung cancer and preneoplastic/preinvasive bronchial epithelium reveals multiple, discontinuous sites of 3p allele loss and three regions of frequent breakpoints. Cancer Res 60:1949–1960
Kopp-Schneider A, Haertel T, Burkolder I, Bannasch P, Wesch H, Groos J, Heeger S (2006) Investigating the formation and growth of α-particle radiation-induced foci of altered hepatocytes: a model-based approach. Radiat Res 166:422–430
Sokolnikov ME, Khokhryakov VF, Vasilenko EK, Koshournikova NA (2003) Risk of lung cancer development in the personnel exposed to internal radiation as a result of incorporated Pu. Sibirian Med J 5:31–35 (in Russian)
Darby S, Hill D, Auvinen A, Barros-Dios JM, Baysson H, Bochicchio F, Deo H, Falk R, Forastiere F, Hakama M, Heid I, Kreienbrock L, Kreuzer M, Lagarde FC, Mäkeläinen I, Muirhead C, Oberaigner W, Pershagen G, Ruano-Ravina A, Ruosteenoja E, Schaffrath RA, Tirmarche MA, Tomášek L, Whitley E, Wichmann HE (2005) Radon in homes and risk of lung cancer: collaborative analysis of individual data from 13 European case-control studies. BMJ 330:223–226
Preston DL, Shimizu Y, Pierce DA, Suyama A, Mabuchi K (2003) Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and non-cancer disease mortality: 1950–1997. Radiat Res 160:381–407
Acknowledgments
The authors thank Nina Koshurnikova for stimulating discussions. The work has been supported by the German Federal Ministry of Environment, Nature Preservation and Reactor Safety, and the German Federal Office of Radiation Protection under contract number StSch 4479.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The definition of γ j in Eq. 1 and β j > 0 imply
With μ j > 0 it follows that
Further, the definition of q j in Eq. 1 implies
Insertion in Eq. 12 yields
or
So, if γ j > 0, then
Rights and permissions
About this article
Cite this article
Jacob, P., Meckbach, R., Sokolnikov, M. et al. Lung cancer risk of Mayak workers: modelling of carcinogenesis and bystander effect. Radiat Environ Biophys 46, 383–394 (2007). https://doi.org/10.1007/s00411-007-0117-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-007-0117-0