Abstract
The possible cancer risks caused by ionizing radiation doses of ~1 mSv or less are too small to be estimated directly from epidemiological data. The linear no-threshold (LNT) approach to estimating such risks involves using epidemiological data at higher (but still low) doses to establish an “anchor point”, and then extrapolating the excess cancer risk linearly down from this point to the low dose of interest. The study in this issue by Professor Tubiana and colleagues, summarizing a French Academy of Sciences report, argues that such LNT extrapolations systematically give substantial overestimates of the excess cancer risk at very low doses. We suggest that, to the contrary, even if there are significant deviations from linearity in the relevant dose range, potentially caused by the effects of inter-cellular interactions or immune surveillance, we know almost nothing quantitatively about these effects. Consequently, we do not know the magnitude, nor even the direction of any such deviations from linearity—the risks could indeed be lower than those predicted by a linear extrapolation, but they could well be higher.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
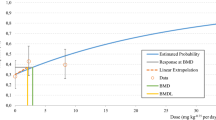
The possible excess cancer risks caused by ionizing radiation doses of ~1 mSv or less are probably too small to be estimated directly from epidemiological data, being buried in the noise of the background cancer risk. The linear no-threshold (LNT) approach to estimating such risks involves using epidemiological data at higher (but still low) doses to establish an “anchor point”, and then extrapolating the excess cancer risk linearly down from this point to the very low doses of interest. The study in this issue [1] by Professor Tubiana and colleagues, summarizing a French Academy of Sciences report [2], provides arguments, which we here critically evaluate, that such LNT extrapolations systematically give substantial overestimates of the excess cancer risk at very low doses.
Microdosimetric argument for the LNT approach
One of the main lines of argument in support of LNT, and one which is strongly criticized by Tubiana and colleagues [1, 2], is the so-called “microdosimetric argument” [3, 4]: Consider a low dose D1 which corresponds to a mean of about one photon passing through a cell nucleus. Let us assume (see below) that there is evidence that this radiation dose causes an increased cancer risk in a human population. Next, suppose that radiation carcinogenesis involves single-cell action, i.e. that radiation effects on separate cells and subsequent development of independent cell lineages dominate, with inter-cellular interactions acting only as comparatively small perturbations of dominant one-lineage effects (the implications of dropping this assumption are discussed later). With these assumptions, of an increased cancer risk at dose D1 and of single-cell action, the same basic biological responses to the radiation damage must operate at, say, a dose of D1/10, as compared with a dose of D1; this follows from the fact that those proportionately fewer cells that were damaged at dose D1/10 would each be subject to the same (single photon) damage as the larger number of cells damaged at dose D1. In other words, at dose D1/10, ten times fewer cells would be damaged, but the nature of damage to those cells would be the same as at dose D1. Given this, the excess risk must simply decrease by the same factor of 10 over the dose range from D1 to D1/10, i.e. linearity would hold.
This microdosimetric argument underlying LNT extrapolations requires, as an anchor point, evidence for a radiation-induced cancer risk in humans at a dose D1, sufficiently low that most exposed cell nuclei are subjected to no more than one energy deposition event. We have argued earlier [4] that the studies of childhood cancer after in-utero exposure of about 6 mGy, as reported, for example, by Mole [5], fulfill the criterion. First, a dose of 6 mGy of 80 kVp X-rays does indeed correspond to a mean of about one photon passing through a cell nucleus [6]. Second, this dose does indeed result in a statistically significant increase in childhood cancer risk; we quote from Mole [5]: “The odds ratio for childhood cancer deaths after X-raying in birth years 1958–61 (1.23, 95% CI 1.04-1.48) and the mean fetal whole body dose from obstetric radiography in 1958 6 mGy can each be derived from nationwide surveys in Britain.... This seems to be the only value for risk of cancer mortality after irradiation in utero based on independent determinations of dose and risk in nationwide samples of the same population of subjects. It is not based on extrapolation or on an unreliable dose response.”
Tubiana et al. [1, 2] have criticized this instance of the microdosimetric argument on three grounds:
-
1.
They suggested that the dose of 6 mGy, reported by Mole [5] in the in-utero study, corresponds to about 10 energy depositions per nucleus. This is not correct for the 80 kVp X-rays used in the in-utero examinations. Based on experimental measurements [6], 6 mGy of 80 kVp X-rays correspond to a mean of about 1 energy deposition in a spherical cell nucleus with a diameter of 7 μm.
-
2.
They suggested that there might not be a causal relationship between the radiation dose and the observed increased cancer risk in the children exposed in utero. Doll and Wakeford [7] reviewed in detail the relationship between the increase in childhood cancer risk and the low-dose radiation exposure, and concluded: “...on review, the evidence against bias and confounding as alternative explanations for the association is strong. Scrutiny of the objections to causality suggests that they are not, or may not be, valid. A causal explanation is supported by evidence indicating an appropriate dose–response relationship and by animal experiments. It is concluded that radiation doses of the order of 10 mGy received by the fetus in utero produce a consequent increase in the risk of childhood cancer”.
-
3.
They questioned the extrapolation from ante- to post-partum exposure; however, they do not give a convincing reason as to why the same dose that causes an increase in cancer risk when delivered in utero, would produce no cancer risk when delivered after birth.
Based on the arguments earlier, we suggest that these three objections by Tubiana et al. [1, 2] to the basis of LNT are not valid—and thus if single-cell action dominates, a linear extrapolation of excess cancer risk from low to very low doses is appropriate for most radiation-induced carcinomas.
Significance of inter-cellular interactions
As we have discussed, the microdosimetric argument in which the LNT model is derived depends on the assumption that a radiation-induced cancer can develop from a single damaged cell, independently of other damaged cells in the tissue of interest. Of course it is known that inter-cellular interactions, and interactions of cells with the extra-cellular matrix, do play a role in radiation carcinogenesis [8–10]; for example, epithelial cancer cells in an organ interact with cells of their own type, with fibroblasts, with inflammatory cells including immune-system cells, and with endothelial cells responsible for vasculature (see reviews in [8–10]). If inter-cellular interactions among radiation-damaged cells play a dominant role during carcinogenesis, rather than being comparatively small modulations of single-cell action, the microdosimetric argument becomes inapplicable, to the extent that the low-dose “anchor-point” dose in the argument now involves many hits to a population of interacting cells, even though any one cell nucleus is unlikely to be hit more than once. Thus a central theoretical underpinning for LNT extrapolation would be called into question. But it would still remain to be determined whether LNT was underestimating or overestimating cancer risks at very low doses.
Specifically, the case made in the French Academy report [2], and by Professor Tubiana and colleagues in this issue [1], is that if inter-cellular interactions are important factors in radiation carcinogenesis, such interactions necessarily imply decreased excess cancer risks per unit dose at very low doses compared to higher doses. But the fact that multi-cellular repair mechanisms are complex and may well control the development of pre-malignant cells [2], does not necessarily imply decreased excess cancer risk per unit dose at very low doses. Many different complex cellular interaction scenarios can be hypothesized, some of which would indeed involve decreased cancer risks per unit dose at low doses (or even zero or negative excess risk), but one can equally well hypothesize inter-cellular carcinogenesis mechanisms that would increase the low-dose risks.
Our understanding of the effect of inter-cellular interactions is still in its infancy, but those multi-cellular effects which have been investigated at low doses, such as bystander responses, often show an increased mutagenic or oncogenic risk per surviving cell [4], compared with what would be estimated using LNT. For example, there is evidence that some bystander effects saturate at quite low doses [11], in which case the first hit to any cell in a communicating population of cells could be more dangerous to the population than subsequent hits to other cells in that population—implying that LNT would underestimate risks at very low doses.
Even for comparatively simple in vitro endpoints, such as DNA double strand breaks, often implicitly considered by Tubiana and colleagues [2] to be mechanistic surrogates for carcinogenesis, we know little about inter-cellular interactions after very low doses of radiation, so it is not surprising that we know little about the quantitative significance of such interactions for low-dose radiation carcinogenesis in vivo.
Significance of immune surveillance
The French Academy report speculated that, at very small doses, immune surveillance or some other mechanism would eliminate, with 100% efficiency, all of the small number of pre-malignantly damaged cells: “at a dose of a few mSv [mGy], lesions are eliminated by disappearance or senescence of the cells” [2]. Such a mechanism would indeed lead to a threshold in dose, below which radiation-induced cancer risks are zero. However, the notion that small numbers of radiation-induced pre-malignant cells can always be highly efficiently “mopped up” seems unlikely for several reasons: firstly, it is well established that we always carry a significant burden of pre-malignant cells which have therefore not been eliminated through immune surveillance or any other mechanism [12]; secondly, what quantitative evidence there is about the dose-dependence of immune surveillance suggests that it is often much less effective when the number of relevant cells is small: this is the well-documented phenomenon of “dilution escape” [13] or “sneaking through” [14], in which small numbers of tumor cells are not recognized and can “sneak through” immune surveillance, while somewhat larger numbers of tumor cells are recognized and are rejected, whereas large numbers of tumor cells can break through immune elimination. Thirdly, a mechanism which is completely effective in removing small numbers of pre-malignant cells would seem to imply that, regardless of radiation exposure, no clonal cancers could ever arise, because pre-malignant clones would always be eliminated when they are still very small in number—in clear contrast to the overwhelming evidence that most cancers are clonal in origin.
Conclusions
The critiques presented by Tubiana and colleagues [1, 2] to the microdosimetric arguments which support LNT do not seem to be valid. It is, however, certainly true that if inter-cellular interactions among radiation-damaged cells dominate carcinogenesis, rather than being small perturbations of the carcinogenesis process, one would expect deviations from LNT. But it would still remain to be determined whether LNT was underestimating or overestimating cancer risks at very low doses, and whether such deviations from linearity were small or large. There is no convincing evidence to support the suggestion that immune surveillance will differentially decrease cancer risks at very low doses, and there is some evidence to the contrary [13, 14].
As we start to learn more about the main mechanisms of inter-cellular communication during carcinogenesis, it will be possible to incorporate this information into quantitative cancer risk models [15]. However, the data summarized in the French Academy report [2], and also in the corresponding US National Academy report [16], both suggest that we currently know little of the magnitude inter-cellular communication effects on radiation carcinogenesis in vivo, whether these effects have similar consequences for different cancer types, or even whether these effects would increase or decrease very low-dose cancer risks compared with the predictions of LNT. In this light it seems premature to use arguments about inter-cellular interactions to justify replacing linearity in cancer risk at very low doses with any non-linear dose–response relationship.
References
Tubiana M, Aurengo A, Averbeck D, Masse R (2006) Recent reports on the effect of low doses of ionizing radiation and its dose–effect relationship. Radiat Environ Biophys 44. DOI 10.1007/s00411-006-0032-9
Tubiana M, Aurengo A, Averbeck D, Bonnin A, Le Guen B, Masse R, Monier R, Valleron AJ, de Vathaire F (2005) Dose–effect relationships and estimation of the carcinogenic effects of low doses of ionizing radiation. Institut de France Académie des Sciences, Paris. (www.academie-sciences.fr/publications/rapports/pdf/dose_effet_07_04_05_gb.pdf)
Rossi HH, Kellerer AM (1972) Radiation carcinogenesis at low doses. Science 175:200–202
Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, Lubin JH, Preston DL, Preston RJ, Puskin JS, Ron E, Sachs RK, Samet JM, Setlow RB, Zaider M (2003) Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA 100:13761–13766
Mole RH (1990) Childhood cancer after prenatal exposure to diagnostic X-ray examinations in Britain. Br J Cancer 62:152–168
Coppola M, Eickel R, Fitzgerald M, Pirrwitz D, Porro F, Booz J (1976) Experimental evaluation of the spectral energy deposition in small volumes by low-LET radiations. In: Booz J, Ebert HG, Smith BGR (eds) Proceedings, Fifth Symposium on Microdosimetry. CEC, Luxembourg
Doll R, Wakeford R (1997) Risk of childhood cancer from fetal irradiation. Br J Radiol 70:130–139
Folkman J (2003) Fundamental concepts of the angiogenic process. Curr Mol Med 3:643–651
Bhowmick NA, Moses HL (2005) Tumor–stroma interactions. Curr Opin Genet Dev 15:97–101
Barcellos-Hoff MH (2005) Integrative radiation carcinogenesis: interactions between cell and tissue responses to DNA damage. Semin Cancer Biol 15:138–148
Brenner DJ, Little JB, Sachs RK (2001) The bystander effect in radiation oncogenesis: II. A quantitative model. Radiat Res 155:402–408
Black WC, Welch HG (1993) Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med 328:1237–1243
Bonmassar E, Menconi E, Goldin A, Cudkowicz G (1974) Escape of small numbers of allogeneic lymphoma cells from immune surveillance. J Natl Cancer Inst 53:475–479
De Boer RJ, Hogeweg P (1985) Tumor escape from immune elimination: simplified precursor bound cytotoxicity models. J Theor Biol 113:719–736
Sachs RK, Chan M, Hlatky L, Hahnfeldt P (2005) Modeling intercellular interactions during carcinogenesis. Radiat Res 164:324–331
National Research Council of the National Academies (2005) Health risks from exposure to low levels of ionizing radiation—BEIR VII. The National Academies Press, Washington, DC
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brenner, D.J., Sachs, R.K. Estimating radiation-induced cancer risks at very low doses: rationale for using a linear no-threshold approach. Radiat Environ Biophys 44, 253–256 (2006). https://doi.org/10.1007/s00411-006-0029-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-006-0029-4