Abstract
An analysis is presented of solid cancer incidence during 11 years of follow-up (1991–2001) of Chernobyl emergency workers residing in Russia. The analysis is based on data from the cohort of male emergency workers from 6 regions in Russia including 55,718 persons with documented external radiation doses in the range of 0.001–0.3 Gy who worked within the 30 -km zone in 1986–1987. The mean age at exposure for these persons was 34.8 years and the mean external radiation dose 0.13 Gy. In the cohort 1,370 cases of solid cancer were diagnosed and 3 follow-up periods were considered: 1991–1995, 1996–2001 and 1991–2001. The second follow-up period was chosen to allow for a minimum latency period of 10 years being characteristic of solid cancers. For risk assessment two control groups have been introduced, the first ‘external’ one representing incidence rates for corresponding ages in Russia in general, the second ‘internal’ one consisting of emergency workers. The risk estimates were based on spontaneous incidence rates of solid cancer. The estimated standardized incidence ratio (SIR) is in good agreement (95% CI) with that of the control. The values of excess relative risk per unit dose (ERR/Gy) for solid malignant neoplasms have been estimated to be 0.33 (95% CI: −0.39, 1.22) (internal control) for the follow-up period 1991–2001 and 0.19 (95% CI: −0.66, 1.27) for 1996–2001.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is important to study the health status of the Chernobyl emergency workers, because cancer incidence rates among emergency workers should be compared with those of the general population and it is necessary to examine the dependence of incidence rates and relatively low radiation doses in the cohort (the mean external gamma radiation dose to emergency workers was 0.1 Gy).
The dose-response relationship of cancer incidence was studied for the Japanese atomic bomb survivors [1], the derived estimates of radiation risks, however, pertained to relatively high doses and dose rates and in this context the cohort of emergency workers (with an average dose of 0.1 Gy) can serve as an additional source of information on the relationship between low radiation doses (up to 0.3 Gy) and solid cancer incidence rates.
For a better understanding of cancer incidence and cancer mortality in the low dose range, studies of workers from the nuclear industry are of particular interest. For these cohorts fairly accurate medical and dosimetric data are available, since nuclear workers are normally under enhanced health monitoring and have individual dose records. To assess the dose-response relationship in the range of low doses and low dose rates, several large-scale studies of cancer incidence among nuclear workers were performed in the UK, Canada, USA, and in other developed countries and the data of existing radiation-epidemiological registries were used [2, 3, 4, 5, 6, 7, 8, 9].
In most of these studies the dependence of mortality (including cancer mortality) on radiation dose was examined. Cancer morbidity and cancer mortality are closely interrelated due to the high lethality of cancer diseases, the dose-response relationship for cancer mortality can, therefore, also be considered characteristic for cancer morbidity.
Any conclusions drawn from the results of such studies regarding radiation risks are rather conflicting (see also Discussion section) and there is evidence for the complexity of the problem when taking into account the significant amount of information required for an adequate statistical power of the study.
Several similar studies have been conducted in Russia [10, 11, 12, 13, 14]. Specifically, some issues of nuclear workers were discussed [10, 12] and the mortality of emergency workers is the subject of [11]. These studies show that cancer incidence has a positive trend as a function of radiation dose.
The analysis of cancer incidence among emergency workers produced some initial results that were presented in 1998 [15]. This study is based on the data of the Russian National Medical and Dosimetric Registry (RNMDR) [16] accumulated in the years 1986–1995. The value ERR 1 Sv was estimated to be above zero for three classes of diseases (all solid cancers, malignant neoplasms of digestive and respiratory organs). A statistically significant excess of ERR 1 Sv above zero was found only for the classes ‘all solid cancers’ and ‘malignant neoplasms of digestive organs’.
The present study is a continuation of the research on cancer incidence among emergency workers. Between 1995 and 2001 the distribution of cancer cases changed significantly: the number of cancer cases registered in this period and diagnosed earlier increased, diagnoses were refined and dates of diagnosis were determined more accurately.
One group selected for the analysis consisted of emergency workers who worked in the 30 -km zone in 1986–1987. These workers received, on average, higher doses than those involved in recovery operations in 1988–1990 and have been subject to annual health examinations, while medical check-ups for other emergency workers are done once every 2 years.
The data used in the study are from medical and dosimetric types for males from six territorial-economic regions of Russia (North-West, Volgo-Vyatsky, Povolzhsky, Central-Chernozemny, North-Caucasus and Urals), because data supplied from these regions are more accurate and reliable.
Comparisons were carried out between cancer incidence in the emergency workers cohort and the general population of Russia, and special attention is given to dose dependences.
Materials and methods
General description of the cohort
The cohort under study has the same dosimetric and demographic characteristics as the general cohort of emergency workers (as of 31.12.2001, the whole cohort registered in the RNMDR included a total of 183,867 male emergency workers). The performed analysis encompasses only males who comprise the overwhelming majority of the cohort (more than 95%).
It should be pointed out that the data to be entered into the registry for a specific period can be added during 1 or 2 years thereafter. For this reason, the last year taken for our study was 2001. Based on the analysis of the dynamics of the standardized cancer incidence ratio since 1986, the year 1991 was chosen as the starting point of the period under consideration, because the SIR increased from 1986 to 1991 and stabilized in the following years. Such changes in SIR are probably explained by varying completeness of the data on cases and other members of the cohort that were submitted in the initial period.
To minimize the possibility that the cohort included emergency workers with existing spontaneous cancer diseases, the time at risk was calculated starting from 2 years after registration. For instance, the time at risk for an emergency worker registered in 1986 has been calculated starting from the beginning of the follow-up period, i.e. 1991. The time at risk for an emergency worker registered in 1992 has been calculated starting from 1994, both for cases and other members of the cohort.
The total cohort included 55,718 persons (as of 31.12.2001), i.e. emergency workers who have been subjected to medical examinations at least once in the considered period (between 1991 and 2001) and for whom data are available on birth date, registration date, documented dose, date of arrival in and departure from the zone of recovery operations.
Three follow-up periods were considered: 1991–1995, 1996–2001 and 1991–2001. The second follow-up period was chosen to allow for a minimum latency of 10 years which is characteristic for solid cancers.
The number of follow-up person-years in 1991–2001 in this cohort was 509,141. A total of 1,370 solid cancer cases were detected in the period under study.
The time at risk for each emergency worker was determined as the time between the date of registration plus a lag of 2 years and the date of latest examination (or date of cancer diagnosis).
Table 1 shows the distribution of cancer incidence for the studied cohort and Table 2 shows the main dosimetric characteristics for the emergency workers.
In the present work, the term ‘dose’ is understood as a documented external radiation dose for an emergency worker. The analysis of dose-response relationship is focused on emergency workers with doses between 1 and 300 mGy.
For the method of radiation dose measurement, the dosimetric data for the studied cohort can be divided into three major groups:
-
1.
Exposure or absorbed dose recorded by individual dosimeters. All emergency workers who worked in the exclusion zone from July 1986 onwards had individual thermoluminescence (TLD) or film dosimeters [16]. A total of 47,451 emergency workers (or 85% of the cohort under study) were covered by individual dosimetric monitoring.
-
2.
Group dose recording assigned to members of the group working in the zone, based on the reading of an individual dosimeter carried by one member of the group.
-
3.
Imputed dose estimation from the mean dose rate in the workplace and duration of stay of that group.
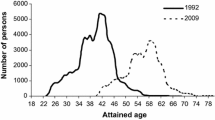
Methods 2 and 3 were used only until June 1986 when dosimeters were in short supply. Figure 1 shows the distribution of emergency workers by radiation dose. As follows from Fig. 1, the distributions for cancer cases and other members of the cohort are very close, which actually means no effect of dose on cancer incidence.
Statistical methods
Risk assessment was performed with the software AMFIT [17] where the cross-tabulation of cases and person-years has dose categories with cut-off points of 1, 50, 95, 125, 175, 210, 300 mGy, along with 5-year intervals of attained ages and 1-year intervals of calendar time. Dose groups were selected to be such that cut-off points did not fall on the limiting (permissible) dose values. According to national regulations the maximum allowable dose in 1986 was 0.25 Gy, in 1987 the dose limit was lowered to 0.1 Gy.
The analysis was based on a general excess relative risk model. The model can be stated formally as:
where λ is the baseline cancer incidence, ρ is the dose-response function, and the function ε describes the dose-effect modification. The baseline rates were modeled as a function of attained age and year of birth. Year of birth was included to allow for time trends in the baseline rates. The effect modifiers included the covariates, as well as time since exposure and age at exposure. The linear dose-response function is written as:
In this equation ERR 1 Gy is the excess relative risk per Gy, and d is the external dose (Gy).
The risk estimates were made using the external (the general spontaneous rate in Russia in 1991–1997 obtained from official statistics) and internal control groups (spontaneous cancer incidence among emergency workers with zero doses).
In calculations with the external control group the risk model takes the form:
in which λ R(a,t) is the spontaneous cancer incidence rate in Russia corresponding to the attained age a and calendar time t; SIR u is the coefficient accounting for the difference between the spontaneous incidence in the emergency workers cohort and the general population of corresponding ages in the time period considered. In the model used this coefficient is equal to the standardized incidence ratio (SIR) for unexposed members of the cohort. The variation of the coefficient SIR u from unity may be explained by completeness and reliability of incidence data in the registry, or possibly ‘the healthy workers effect’ resulting from additional medical check-ups for emergency workers before going to work in the zone. The selected risk model has the advantage of estimating both the dose-response and the difference in spontaneous cancer incidence in the followed up cohort and the reference Russian population.
When risk coefficients were estimated using the internal control, data were stratified by attained age and calendar time.
Results
Figure 2 shows the dependence of SIR on time (1991–2001) and as can be seen, the value of SIR is in agreement with the control within statistical errors.
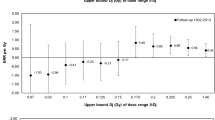
Tables 3, 4, and 5 include the results of estimating the radiation risk coefficients for cancer by the dose groups as a function of the follow-up period. The risk coefficients obtained using external and internal controls are practically identical. It can be seen from the presented results that radiation risks for all cancers are positively correlated, but not statistically significant.
The values of relative risk exceed unity in dose groups 4, 5, and 6, the excess was statically significant in groups 4 and 5 (see Table 5).
To verify the statistical significance of risk coefficients, all data in these groups were divided into two groups regarding absorbed dose: i) 1–150 mSv, and ii) 150–300 mSv. Results of the calculations are presented in Table 6 and, as can be seen, the value of excess relative risk per 1 Gy (ERR 1 Gy ) is positive, but not statistically significant.
Table 7 contains estimates of ERR 1 Gy for major subcategories (sites) of malignant neoplasms. The maximum values of ERR 1 Gy were obtained for digestive organs, male genital organs, mesothelial and soft tissues. It should be kept in mind, however, that for the last two sites the number of cases is quite limited. The value of excess relative risk per unit dose for all subcategories of malignant neoplasms is not statistically significant. As can be seen from Table 7, malignant neoplasms of respiratory organs represent the major number of cases. It should be stressed that risk estimates for this cancer site did not consider any confounding factor, such as smoking. Unfortunately, there are no data on this harmful habit in the RNMDR and it can, therefore, not be taken into consideration.
Discussion
The present work is a logical extension of the study of cancer incidence among emergency workers conducted in Russia [15]. The issue of cancer incidence or mortality continues to be of importance because emergency workers, on average, received higher radiation doses than the general population of the affected areas. The value ERR 1 Sv was estimated to be above zero for three classes of diseases, i.e. all solid cancers, malignant neoplasms of digestive and respiratory organs, respectively (see [15]). The statistically significant excess of ERR 1 Gy above zero was found only for the two classes ‘all solid cancers’ and ‘digestive organs’. The values of risk coefficients derived in this study are much lower than those presented in [15]. ERR 1 Gy was 1.13 (0.14, 2.13, 95% CI) for all solid cancers and 2.41 (0.10, 4.71, 95% CI) for digestive organs. As shown by the analysis of data since 1986, the risks were highest in the first 5 years after the Chernobyl accident. This can hardly be due to the effect of exposure during this time period and is most probably explained by the way information was compiled in the database in the first years of the registry, which goes beyond the scope of the present paper.
When comparing the results of the present study with the estimates reported in [15], it is evident that the radiation risk of cancer decreases with time, that means we are comparing a value of 1.13 for the period 1986–1995 with corresponding values of 0.76 for the period 1991–1995 and 0.2 for 1996–2001 (this study). The reasons for such time variations in risk are actually unknown and need to be investigated separately. Several hypotheses can be suggested. First, there might be a bias in estimates due to the short follow-up period after exposure and due to a possible effect of latent spontaneous incidence on the risk estimates. In this respect, the results obtained for 1996 through 2001 are bound to be more reliable. The changes in risk may also have something to do with the heterogeneity of the population (people having different radiosensitivity and states of health). The heterogeneity tends to decrease with time due to the death of weak cohort members and, thus, an increasing health level in the cohort. This can be illustrated by the mortality peak in Russia in 1994–1995 resulting from social and economic problems at that time [11] and a decrease in mortality in later years. It should be pointed out that a mortality peak was detected among males of 40–45 years of age, which was the age of emergency workers during those years. A similar effect was probably observed in the LSS cohort and it was partly responsible for the increased life expectancy among the surviving members of the cohort. On the other hand, the results of radio-epidemiological studies available in the literature pertain to a latency time of 10 years after exposure.
It cannot be ruled out that risk estimates are influenced by the heterogeneity of the emergency workers’ cohort with varying social status. For example, improved registration levels among emergency workers belonging to government officials and highly qualified personnel characterized by enhanced health monitoring can lead to reassessment of risk. The mean doses for these categories of emergency workers are generally not very high: up to 0.1 Gy and an increase in registration level in the low dose range will result in a larger angle of the linear dose-response relationship.
Another important aspect of the conducted risk analysis has to be emphasized: the influence of uncertainty in radiation doses on radiation risk estimates. As indicated in the ‘Materials and methods’ section, three different methods were used for the determination of doses. The majority of doses (about 85%) were measured using individual dosimeters, the rest included group dose determinations or imputed doses. The proportion of the least accurate imputed doses, as shown by the survey of 700 emergency workers from the Kaluga Oblast within the Registry, is about 5% [19]. The uncertainty associated with dose estimations according to [19] could be as high as 50% at maximum when using the first method of measurements, 300% with the second method and 500% with the third. The source of error in the first case could have been an improper way of carrying a dosimeter (intended overexposure or underexposure). With the second method, errors could be due to significant gradients of dose rates at working sites, whereas for the third method errors might be associated with inaccurate information on time and place of operations plus uncertainty in dose rate. However, it is believed that doses have no systematic bias towards overestimation, as both physical and biological methods of dose determination give about the same mean doses.
The above statement is confirmed by the estimates of radiation risk for emergency workers with individual dosimetry (working in the exclusion zone from July 1986). The value of ERR per Gy for these emergency workers is estimated to be 0.24 (−0.7; 1.4) which is close to the value of 0.20 derived for the whole cohort: in other words there seems to be no bias in risk estimate.
The values of radiation risk coefficients calculated for the period of 1991–2001 agree with the LSS cohort studies [20] where the value of ERR per 1 Gy is 0.39±0.20 for radiogenic solid cancers for males exposed at the age of 30 years and having received doses of 100–200 mSv. The derived results are in qualitative agreement with the results of an analysis on dose-relationship of mortality due to malignant neoplasms in nuclear workers (Table 8), furthermore, the positive trend of cancer mortality as a function of dose has been revealed in most of the studies.
Thus, the results of the study lead us to conclude that there is a positive, yet statistically insignificant excess relative risk of radiogenic solid cancers in the cohort of emergency workers.
Given the derived risk estimates and the low doses, the number of radiation-induced cancers will be insignificant. Even with the maximum estimate of excess relative risk for all solid cancers (with the upper bound of 95% CI equal to 1.22 Gy−1) from Table 5, the attributable risk of radiogenic cancers will be 10% (with a mean dose of 0.1 Gy), which corresponds to 25 radiation-induced cancers among 100,000 emergency workers per year and with the spontaneous incidence rate being 196×105/8×104=250 per 100,000 persons (Table 3, first line).
It is the authors’ opinion that risk coefficients can be estimated using the relative age distribution of spontaneous cancer incidence normalized to national rates (external control). In our study the risk coefficients estimated with external and internal controls have been shown to be close. The proposed approach, in our view, could be particularly advantageous for consideration of rare cancer sites when the accuracy of determination of spontaneous cancer incidence is not high.
Conclusions
-
1.
For the considered dose interval (1–300 mSv) and for the period 1991–2001, the spontaneous incidence rate of solid cancer among emergency workers agrees, within confidence intervals, with that for the general Russian population.
-
2.
The values of the excess relative risk per unit dose (ERR/Gy) for malignant neoplasms are estimated to be 0.34 (−0.39, 1.22, 95% CI) for the follow-up period 1991–2001 and 0.20 (−0.66, 1.30, 95% CI) for the follow-up period 1996–2000, respectively.
-
3.
The presented estimates of radiation risk should be treated as preliminary because the follow-up period is rather short and the number of cases considered in the analysis is relatively small.
-
4.
The values of the excess relative risk per unit dose have been found to be positive, even though not statistically significant and, therefore, the question of dose-dependence of cancer incidence among emergency workers remains open and requires further investigation.
References
Thompson DE, Mabuchi K, Ron E et al. (1994) Cancer incidence in atomic bomb survivors. Part II. Solid tumors, 1958–1987. Radiat Res 137:S17–67
Gilbert ES, Cragle DL, Wiggs LD (1993) Updated analysis of combined mortality data for workers at the Hanford Site, Oak Ridge National Laboratory and Rocky Flats Nuclear Weapons Plant. Radiat Res 136:408–421
Kendall GM, Muirhead CR, MacGibbon BH et al. (1992) Mortality and occupational exposure to radiation: first analysis of the National Registry for radiation workers. BMJ 304:220–225
Muirhead CR, Goodill AA, Haylock RGE et al. (1999) Occupational radiation exposure and mortality: second analysis of the National Registry for radiation workers. J Radiol Prot 19:3–26
Asmore JP, Krewsky D, Zielinsky JM et al. (1998) First analyses of mortality and occupational radiation exposure based on National Dose Registry of Canada. Am J Epidemiol 148:564–574
Cardis E, Gilbert ES, Carpenter L et al. (1995) Effects of low doses and low dose rates of external ionizing radiation: cancer mortality among nuclear workers in three countries. Radiat Res 142:117–132
Carpenter L, Higgins C, Douglas A, Fraser P, Beral V, Smith P (1994) Combined analysis of mortality in the three United Kingdom Nuclear industry workforces, 1946–1988. Radiat Res 138:224–238
Gribbin MA, Weeks JL, Howe GR (1993) Cancer mortality (1956–1985) among male employees of atomic energy of Canada limited with respect to occupational exposure to external low-linear-energy-transfer ionizing radiation. Radiat Res 133:375–380
Ron E, Muirhead C (1998) The carcinogenic effects of ionizing radiation: epidemiological evidence. In: Low doses of ionizing radiation: biological effects and regulatory control. Invited papers and discussion. Proceedings of an International Conference, Seville, Spain, 17–21 November 1997. International Atomic Energy Agency, Vienna, pp 165–180
Koshurnikova NA, Bysogolov GD, Bolotnikova MG et al. (1996) Mortality among personnel who worked at the Mayak complex in the first years of its operation. Health Phys 71:90–93
Ivanov VK, Gorski AI, Maksioutov MA, Tsyb AF, Suchkevitch GN (2001) Mortality among the Chernobyl emergency workers: estimation of radiation risks (preliminary analysis). Health Phys 81:514–521
Ivanov VK, Tsyb AF, Rastopchin EM et al. (2001) Cancer incidence among nuclear workers in Russia based on data from the institute of physics and power engineering: a preliminary analysis. Radiat Res 155:801–808
Ivanov VK, Tsyb AF, Petrov AV, Maksioutov MA, Shilyaeva TP, Kochergina EV (2002) Thyroid cancer incidence among liquidators of the Chernobyl accident: absence of dependence of radiation risks on external radiation dose. Radiat Environ Biophys 41:195–198
Ivanov VK, Tsyb AF, Gorsky AI et al. (1997) Leukemia and thyroid cancer in liquidators of the Chernobyl accident: estimation of radiation risks (1986–1995). Radiat Environ Biophys 36:9–16
Ivanov VK, Rastopchin EM, Gorski AI, Ryvkin VG (1998) Cancer incidence among liquidators of the Chernobyl accident: solid tumors, 1986–1995. Health Phys 74:309–315
UNSCEAR (2000) Report. Sources and effects of ionizing radiation. Vol.II: Effects. UNSCEAR United Nations Scientific Committee on the Effects of Atomic Radiation, United Nations, New York, pp 470–471
Preston DL, Lubin JH, Pierce DA, McConney ME (1993) EPICURE. Hirosoft International Corporation, Seattle, USA
WHO (1977) International classification of diseases, 10th revision. World Health Organization, Geneva
Pitkevich VA, Ivanov VK, Tsyb AF (1995) Dosimetric data of the All-Russian Medical and Dosimetric State Registry for emergency workers. Special Issue. Bulletin of the All-Russian Medical and Dosimetric State Registry, Moscow
Pierce A, Preston DL (1997) Commentary on: no evidence for increased tumor rates below 200 mSv in the atomic bomb survivors’ data. Radiat Environ Biophys 36:209–210
Douglas AJ, Omar RZ, Smith PG (1994) Cancer mortality and morbidity among workers at the Sellafield plant of British nuclear fuels. Br J Cancer 70:1232--1243
Fraser P, Carpenter L, Maconochie N, Higgins C, Booth M, Beral V (1993) Cancer mortality and morbidity in employees of the United Kingdom Atomic Authority. Br J Cancer 67:615--624
Beral V, Fraser P, Carpenter L, Booth A, Brown A, Rose G (1988) Mortality of employees of the atomic weapons establishment 1951--82. Br Med J 297:757--770
Frome EL, Cragle DL, Watkins JP, Wing S, Shy CM, Tankersley WG, West GM (1997) A mortality study of employees of the nuclear industry in Oak Ridge. Radiat Res 148:64--80
Wing S, Shy CM, Wood JL, Wolf S, Cragle DL, Frome EL (1991) Mortality among workers at Oak Ridge National Laboratory: Evidence of radiation effects in follow-up through 1984. J Am Assoc 265:1397--1402
Gilbert ES, Omohundro E, Buchanan JA, Holter NA (1993) Mortality of workers at the Hanford site: 1945--1986. Health Phys 64:577--590
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ivanov, V.K., Gorski, A.I., Tsyb, A.F. et al. Solid cancer incidence among the Chernobyl emergency workers residing in Russia: estimation of radiation risks. Radiat Environ Biophys 43, 35–42 (2004). https://doi.org/10.1007/s00411-003-0223-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-003-0223-6