Abstract
Purpose
The immuno-nutritional status is closely related to the prognosis in many cancers. Controlling nutritional status (CONUT) score is a new parameter that reflects the immuno-nutritional status and is prognostic in some cancers. However, the prognostic significance of the CONUT score in small cell lung cancer (SCLC) is unknown. We aimed to demonstrate the prognostic significance of the CONUT score in patients with SCLC.
Methods
Two hundred sixteen patients who were followed up with SCLC were included in the study retrospectively. According to the receiver operating characteristic (ROC) curve analysis, the optimal cutoff values were determined for the CONUT score, and the patients were divided into low (< 2) and high (≥ 2) CONUT groups. Neutrophil–lymphocyte ratio (NLR), systemic immune-inflammation index (SII), and prognostic nutritional index (PNI) were grouped based on a cutoff point 2.84, 626, and 46.1, respectively. Cox regression analyses were used to assess their prognostic values for progression-free survival (PFS) and overall survival (OS).
Results
The high CONUT group had significantly worse PFS and OS than the low CONUT group (p < 0.001, p < 0.001). In univariate analysis, stage, prophylactic cranial irradiation, extrapulmonary lesion, PNI, body mass index, CONUT score were found to be significant for both PFS and OS. In multivariate analysis, only CONUT score and stage were found as independent prognostic factors for both PFS (p: 0.018, p: 0.046) and OS (p: 0.038, p: 0.006).
Conclusion
The CONUT score at the time of diagnosis is an independent prognostic parameter that predicts recurrence and survival times in SCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Small cell lung cancer (SCLC) accounts for about 15% of lung cancers, which make up 11.6% of all cancers [1, 2]. SCLC has a more aggressive biological nature compared to lung cancers in other histologies, and they tend to grow faster and metastasis earlier [1]. In addition to conventional chemotherapy, thoracic radiotherapy, and prophylactic cranial irradiation (PCI) in the treatment of patients with SCLC, immune checkpoint inhibitors have recently been included, particularly in extensive disease [1, 3, 4]. Although some clinical variables such as performance status, age, weight loss, stage, and serum lactate dehydrogenase (LDH) are considered to be prognostic in patients with SCLC, there is no standardized prognostic parameter yet [5]. For this reason, new prognostic markers that can be used in daily practice are still needed to predict the prognosis of patients with SCLC at the time of diagnosis and to determine treatment strategies.
Recently, there is growing evidence that increased systemic inflammation and impaired immuno-nutritional status is closely related to carcinogenesis [6]. Pro-inflammatory mediators increase during the development of cancer cells and increased systemic inflammation mediates the proliferation, invasion and migration of tumor cells [6]. Inflammatory cytokines such as tumor necrosis factor α (TNF-α), interleukin (IL) -1, IL-6, interferon-γ which are overexpressed in the tumoral microenvironment, impairs the host's immuno-nutritional status with both direct and indirect effects [6, 7]. Many studies in murine models have shown the effects of some cytokines and their relationships with each other [8,9,10,11]. Of these cytokines, TNF-α and IL-1 penetrate the blood–brain barrier and interact with epithelial cells in the brain [7, 8]. The findings from animal studies showed that this process may be related with anorexia [7, 8]. In addition, TNF-α directly increases gluconeogenesis, promotes the breakdown of fats and proteins [8]. It also reduces the synthesis of proteins, lipids and glycogen [8]. Additionally, TNF-α increases the activity of reactive oxygen radicals in tissues and then activates the ubiquitin–proteasome pathway and causes degradation of muscle proteins [9]. Increased IL-1 has a similar effect to TNF-α [8]. IL-6, one of the important cytokines for the systemic inflammatory response, increases the breakdown of adipose tissue [10]. It also induces catabolism in tissues and causes protein degradation in skeletal muscles [10]. Also due to increased inflammatory response, increased catabolism cause lipolysis of adipose tissue, proteolysis of muscle tissue, and susceptibility to nutritional defect (ND) [11]. As a result of these complex pathways, in patients with SCLC, the nutritional status is often abnormal [12].
Some markers such as neutrophil–lymphocyte ratio (NLR), systemic immune-inflammation index (SII), and prognostic nutritional index (PNI), which are systemic inflammatory and immuno-nutritional indicators, are associated with prognosis in many malignancies such as SCLC, non-SCLC (NSCLC), gastric cancer (GC), hepatocellular carcinoma (HCC), and colorectal cancer (CRC) [13,14,15].
Controlling nutritional status (CONUT) score is a relatively new immuno-nutritional biomarker derived from serum albumin concentration, total lymphocyte count (TLC), and total cholesterol concentration (TC) [16]. CONUT score has a significant relationship with prognosis and survival in hematological malignancies such as multiple myeloma (MM) and some solid organ malignancies such as GC, renal cell carcinoma (RCC), and HCC [17,18,19,20]. Regarding lung cancer, in two studies with patients with squamous and adenocarcinoma histology, the CONUT score was a prognostic factor for both disease-free survival (DFS) and overall survival (OS) [12, 21]. In a study with patients with stage I NSCLC, a high CONUT score was associated with poor prognosis [22]. However, the prognostic significance of the CONUT score in SCLC is unknown. In this study, we aimed to reveal the prognostic importance of the CONUT score at the time of diagnosis in patients with SCLC.
Methods and Materials
Patients
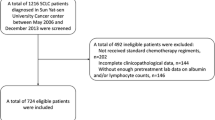
In this study, 276 patients who were followed up with the diagnosis of SCLC at Ataturk University Research and Application Hospital (AURAH) between January 2010 and August 2019 were retrospectively analyzed. Patients with a previous solid organ malignancy and systemic infection were excluded from the study. Besides, those with diseases such as liver and thyroid disease and those undergoing hyperlipidemia treatment, which may affect the level of TC, and those with hematological and non-hematological malignancies, autoimmune, chronic inflammatory and rheumatological diseases and those who use drugs such as steroids, which may affect TLC level, were excluded. Therefore, 60 patients were excluded from the study. Tumors of a total of 216 SCLC patients included in the study were classified based on the tumor node metastasis (TNM) system of the 2017 American Joint Committee on Cancer (AJCC) [23].
Data Collection and Definition
Clinical variables such as gender, age, Eastern Cooperative Oncology Group (ECOG) performance status, and tumor placement characteristics were obtained from the patient file records. The value 18.5 kg/m2, which the World Health Organization (WHO) accepts as the normal weight lower limit for body mass index (BMI), was taken as the determining value [24]. Therefore, the patients were divided into groups as < 18.5 and ≥ 18.5 kg/m2 according to their BMI. Laboratory findings such as neutrophils, lymphocytes, and platelets at the time of diagnosis were obtained from the AURAH electronic data system.
Blood results at the time of diagnosis of all patients were evaluated. As shown in Table 1, the CONUT score was calculated using the albumin concentration, TLC, and TC concentration [11]. NLR was computed by dividing the neutrophil count by the lymphocyte count. SII was determined with the formula of (platelet × neutrophil/lymphocyte). PNI values were worked out with the formula of [(10 × albumin (g / L)) + (0.005 × TLC)].
Follow-Up
During the treatment period from the date of diagnosis, physical examination, and serum chemistry of the patients were performed monthly, and chest-abdominal computed tomography (CT) was performed when necessary. In limited disease, follow-up of patients was performed quarterly for the first two years, semi-annually for the third year, and annually in the following years. In extensive disease, follow-up was performed bimonthly for the first year, quarterly in the 2nd and 3rd years, semi-annually in the 4th and 5th years, and then annually. Chest-abdominal CT was performed at each visit, and brain magnetic resonance imaging (MRI) or CT was performed every three months in the first year and every six months for two years after the first year.
Study Endpoints
Progression-free survival (PFS) was determined as the time interval from the time of diagnosis to progression or death. OS was defined as the period from the time of diagnosis until death and the last follow-up period for living patients.
Statistics
The receiver operating characteristic (ROC) curve analysis was performed to determine the best cutoff value for variables, and the areas under the curve (AUCs) were calculated. CONUT score and the other parameters were evaluated as dichotomized variables by obtaining the best cutoff value. Shapiro–Wilk test was used to determine if variables were normally distributed. The Chi-square (Χ2) test or Fisher's exact test was used to analyze the relationship between the group of low and high CONUT with clinic-pathological parameters.
Associations between parameters with survival were analyzed using Kaplan–Meier curves and compared by the log-rank test. Hazard ratios (HRs) estimated from the Cox analysis were reported as relative risks with corresponding 95% confidence intervals (CIs). All variables with a p-value < 0.05 in the univariate analysis were included in multivariate Cox regression analysis with backward selection. p < 0.05 was considered statistically significant in multivariate Cox regression analysis. All analyses were performed using the SPSS statistical software package (SPSS statistics 21.0).
Results
Determination of Optimal Cut-Off Values of CONUT Score and Other Parameters
According to the ROC curve analysis, the best cutoff point for the CONUT score was 2, which provided the most appropriate sensitivity of 63% and specificity of 85%. The cutoff values for the highest sensitivity and specificity for NLR, SII, PNI were 2.84, 626, 46.1, respectively. Among the prognostic factors, the CONUT score has the highest AUC (0.73). AUC values for NLR (0.61), SII (0.58), and PNI (0.71) were found as indicated.
Distribution of the Components by the CONUT Groups
The albumin, TLC, and TC scores of the patients in the high CONUT group were significantly higher than those in the low CONUT group. Table 2 shows the distribution of the CONUT score components by CONUT groups.
Associations of the CONUT Score with the Clinical and Pathological Variables
The median age of 216 patients included in the study was 61 (36–83) years. One hundred eleven (51.4%) of the patients were over 60 years old, and 105 (48.6%) were 60 years old or younger. Median serum albumin, TLC, and TC values were 3.6 (2–4.84) g/dl, 1.8 × 109/l (0.47–7.70), and 200 (81–350) mg/dl, respectively. One hundred and twenty-seven (58.7%) patients had a high CONUT score (≥ 2), and 89 (41.3%) patients had a low CONUT score (< 2). High CONUT score group was significantly relationship with the presence of high NLR (≥ 2.84), high SII (≥ 626), low PNI (< 46.1), and low BMI (< 18.5). There was no significant difference between the high and low CONUT score groups in terms of other clinical and pathological parameters (Table 3).
Associations of CONUT Score with Survival Outcomes
At the end of 10 (1–74) months of median follow-up, 201 (93.1%) of patients were progressed, while 195 (90.3%) patients died. The median PFS duration of the patients was 7 months, and the median OS duration was 10 months. In the patient group with a high CONUT score, both PFS (5 vs. 10 months, p < 0.001) and OS (9 vs. 14 months, p < 0.001) were shorter than the group with low CONUT score (Fig. 1).
According to the Kaplan–Meier survival analysis, in the extensive stage group, both PFS (6 vs 11 months, p < 0.001) and OS (9 vs 15 months, p < 0.001) were shorter than in the limited stage group. Both PFS and OS were significantly higher in patients who received PCI than patients who did not receive PCI (11 vs 7 months, p: 0.028; 16 vs 10 months, p: 0.008, respectively). PFS/OS were 11/15, 7/10, 6/9 months in extrapulmonary lesion 0, 1, > 1 groups, respectively, and the differences between these values were significant for both PFS and OS (p < 0.001, p < 0.001, respectively). Although OS (10 vs 13 months, p: 0.028) was shorter in patients with high SII when compared to low SII, there was no difference for PFS. Patients with low PNI and low BMI had shorter PFS (6 vs 10 months, p < 0.001, 5 vs 9 months, p < 0.001, respectively) and OS times (9 vs 15 months, p < 0.001, 8 vs 12 months, p < 0.001, respectively) than those with high PNI and high BMI. There was no significant difference in PFS and OS times for other parameters.
As seen in Table 4, in univariate Cox regression analysis, the stage (HR: 0.483, p < 0.001), PCI (HR: 1.521, p: 0.038), extrapulmonary lesion (HR: 0.505, p < 0.001), PNI (HR: 1.659, p: 0.001), BMI (HR: 1.806, p < 0.001), and CONUT score (HR: 0.497, p < 0.001) were significant prognostic parameters of PFS. In univariate analysis, the stage (HR: 0.424, p < 0.001), PCI (HR: 1.692, p: 0.012), extrapulmonary lesion (HR: 0.437, p < 0.001), SII (HR: 0.714, p: 0.035), PNI (HR: 1.814, p < 0.001), BMI (HR: 1.903, p < 0.001), and CONUT score (HR: 0.476, p < 0.001) were all significant prognostic indicators for OS (Table 5). Among these immune-nutritional indicators, the HR of PNI and BMI was above 1, whereas the HR of SII and CONUT score was below 1. In the multivariate analysis, only the CONUT score (HR: 0.612, p: 0.018; HR: 0.650, p: 0.038, respectively) and the stage (HR: 0.121, p: 0.046; HR: 0.111, p: 0.006, respectively) were found independent prognostic factors for PFS and OS.
Discussion
SCLC occupies an important part of all lung cancers and is characterized by poor prognosis [1]. This study showed that the CONUT score, which is an immuno-nutritional indicator, is an independent prognostic factor for SCLC in both PFS and OS, and the high CONUT score at the time of diagnosis is associated with shorter PFS and OS times. To the best of our knowledge, this was the first study to demonstrate the prognostic significance of the CONUT score in SCLC. Additionally, although there was a significant relationship between CONUT score groups and some other inflammatory and nutritional markers such as NLR, SII, and PNI, none of these markers were found to be independent prognostic factors for survival.
The prognostic effect of inflammation and immuno-nutritional status in cancer patients has been the basis of many studies. In light of these studies, it has been shown that impaired nutritional status and increased inflammatory response have important relationship with poor prognosis in cancer patients [25]. NLR, which is one of the systemic inflammatory indicators, has prognostic significance in many cancers such as breast, bladder, and lung cancer [26,27,28]. In a study in SCLC patients, Lohinai et al. showed that low NLR (cutoff: 2.2) was associated with longer survival time in stage I-II patients [29]. Bernhardt et al. showed that NLR is not an independent prognostic factor in their study involving 350 SCLC patients [25]. In our study, we showed that patients in the high CONUT score group had significantly higher NLR results than the low CONUT group. However, we could not find NLR alone as a prognostic factor for either PFS or OS.
Another inflammatory-based index is SII obtained from a combination of platelets, neutrophils, and lymphocytes. In a meta-analysis involving 2786 lung cancer patients, Zang et al. identified the threshold value for SII as 640 and showed that high SII was associated with a reduced survival [30]. One of the few studies investigating the importance of SII in SCLC patients included 919 patients and SII, stage, LDH, and response to therapy were found to be independent prognostic factors for OS [31]. In our study, the cutoff value for SII was determined as 626, and it was shown that the patients in the high CONUT score group also had significantly higher SII values. Besides, SII was found significant only for OS in univariate analysis, but not significant in multivariate analysis. As few studies are investigating the prognostic significance of SII in SCLC patients, we think it would be beneficial to confirm the results with the studies to be conducted.
PNI, which has been used in recent years and reflects the immuno-nutritional status, is calculated from serum albumin concentration and peripheral lymphocyte count. PNI is prognostic in many solid organ malignancies, such as lung cancer, CRC, GC, and ovarian cancer [15, 32,33,34]. In a meta-analysis included 17 studies involving patients with NSCLC and four studies involving patients with SCLC. This meta-analysis showed that low pre-treatment PNI was associated with shorter OS, DFS, PFS, and relapse-free survival (RFS) in patients with NSCLC, and was associated with shorter OS time in patients with SCLC [35]. Jin et al. found the stage, PNI, and age as independent prognostic factors for OS in patients with SCLC [4]. Although we showed that PNI was significant for PFS and OS in accordance with previous studies, we could not detect it as an independent prognostic factor. Moreover, we showed that the PNI value was significantly lower, and the survival times were shorter in the high CONUT score group.
CONUT score is an immuno-nutritional scoring system obtained from the combined evaluation of serum albumin concentration, TLC, and TC. Serum albumin is a good indicator reflecting nutritional status due to the negative correlation between its concentration and ND [36]. Hypoalbuminemia is not only an indicator of ND but also of decreased liver reserve and increased inflammatory cytokine response in the tumoral microenvironment [36, 37]. Lymphocytes, another component of the CONUT score, play an essential role in host immunity, both by stimulating cytotoxic cell death and apoptosis and by inhibiting cell proliferation, and therefore lymphocytes are another critical indicator of inflammatory status [38]. The last variable of the CONUT score is TC. In cancer patients, due to increased low-density lipoproteins receptor (LDLR) expression and increased intracellular low-density lipoproteins (LDL) intake, mandatory oxidative phosphorylation increases, leading to hypocholesterolemia. In addition to the change in lipid metabolism in patients with SCLC, another cause of hypocholesterolemia may be cachexia [39, 40]. Important causes of cachexia are cytokines-induced anorexia (TNFα, IL-1, IL-6, etc.), insufficient calorie intake and increased catabolism as a result of systemic changes in metabolism [7,8,9,10].
The CONUT score is prognostic in some solid organ cancers such as GC and NSCLC [41, 42]. In a study with HCC patients, the preoperative CONUT score was an independent prognostic factor for OS [20]. However, few studies are investigating the importance of the CONUT score in patients with lung cancer. In one of these, Toyokawa et al. showed that high CONUT score was associated with short DFS and OS in 108 patients with squamous cell lung carcinoma [21]. Another study showed that in patients with NSCLC treated with pembrolizumab, the CONUT score was a predictor that both showed therapeutic effect and predicted prognosis [42]. In a study in which 109 patients with lung adenocarcinoma and obstructive pulmonary disease were included, the cutoff value was determined as 1 (AUC: 0.596; sensitivity 67%, specificity 43%), for the CONUT score, and the high (≥ 1) CONUT score was found to be associated with short DFS and OS [12]. In our study, the cutoff value was determined as 2 for the CONUT score (sensitivity 63%, specificity 85%), and it was found that the high (≥ 2) CONUT score at diagnosis in SCLC patients was associated with shortened PFS and OS time. Also, the CONUT score at the time of diagnosis was an independent prognostic factor for both PFS and OS. In addition to all these, the highest AUC was 0.73 for CONUT score, indicating the superiority of this factor relative to other markers.
Finally, for the first time in this study, we showed that the CONUT score at the time of diagnosis is a prognostic parameter for patients with SCLC. These new results show that the high CONUT score is an important scoring system that predicts shortened survival in SCLC patients. The CONUT score, which contains all three of the albumin, TLC, and TC, is a good indicator of the increased inflammatory response and impaired nutritional status in SCLC, known for its aggressive structure. The CONUT score is a useful parameter that can be easily applied in daily practice and it can help decision-making process for the clinician.
There were two important limiting points in our study. First of all, our study was retrospective and included relatively few patients. Another was that inflammatory and immuno-nutritional indicators such as C-reactive protein, weight loss, and skin thickness were not included in the study. Therefore, we think that studies with prospective and multicenter cohorts, in which more variables are involved, will be beneficial.
References
Wang D, Guo D, Shi F et al (2019) The predictive effect of the systemic immune-inflammation index for patients with small-cell lung cancer. Future Oncol 15(29):3367–3379
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Horn L, Mansfield AS, Szczęsna A et al (2018) First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med 6 379(23):2220–2229
Jin S, Cao S, Xu S et al (2018) Clinical impact of pretreatment prognostic nutritional index (PNI) in small cell lung cancer patients treated with platinum-based chemotherapy. Clin Respir J 12(9):2433–2440. https://doi.org/10.1111/crj.12925
Go SI, Jeon H, Park SW et al (2018) Low pre-treatment nutritional index is significantly related to poor outcomes in small cell lung cancer. Thorac Cancer 9(11):1483–1491
Alwarawrah Y, Kiernan K, MacIver NJ (2018) Changes in nutritional status impact immune cell metabolism and function. Front Immunol 16(9):1055
Banks WA (2001) Anorectic effects of circulating cytokines: role of the vascular blood-brain barrier. Nutrition 17:434–437
Zhu R, Liu Z, Jiao R et al (2019) Updates on the pathogenesis of advanced lung cancer-induced cachexia. Thorac Cancer 10(1):8–16
Kamp CM, Langen RC, Snepvangers FJ et al (2013) Nuclear transcription factor kB activation and protein turnover adaptations in skeletal muscle of patients with progressive stages of lung cancer cachexia. Am J Clin Nutr 98:738–748
Fearon KC, Barber MD, Falconer JS et al (1999) Pancreatic cancer as a model: Inflammatory mediators, acute-phase response, and cancer cachexia. World J Surg 23:584–588
Sørensen J (2018) Lung cancer cachexia: can molecular understanding guide clinical management? Integr Cancer Ther 17(3):1000–1008
Akamine T, Toyokawa G, Matsubara T et al (2017) Significance of the preoperative CONUT score in predicting postoperative disease-free and overall survival in patients with lung adenocarcinoma with obstructive lung disease. Anticancer Res 37(5):2735–2742
Sakin A, Sahin S, Yasar N et al (2019) The relation between hemogram parameters and survival in extensive-stage small cell lung cancer. Oncol Res Treat 42(10):506–515
Yang R, Chang Q, Meng X et al (2018) Prognostic value of systemic immune-inflammation index in cancer: a meta-analysis. J Cancer 7 9(18):3295–3302
Li D, Yuan X, Liu J et al (2018) Prognostic value of prognostic nutritional index in lung cancer: a meta-analysis. J Thorac Dis 10(9):5298–5307
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG et al (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20(1):38–45
Okamoto S, Ureshino H, Kidoguchi K et al (2020) Clinical impact of the CONUT score in patients with multiple myeloma. Ann Hematol 99(1):113–119
Takagi K, Domagala P, Polak WG et al (2019) Prognostic significance of the controlling nutritional status (CONUT) score in patients undergoing gastrectomy for gastric cancer: a systematic review and meta-analysis. BMC Surg 5 19(1):129
Elghiaty A, Kim J, Jang WS et al (2019) Preoperative controlling nutritional status (CONUT) score as a novel immune-nutritional predictor of survival in non-metastatic clear cell renal cell carcinoma of ≤ 7 cm on preoperative imaging. J Cancer Res Clin Oncol 145(4):957–965
Lin ZX, Ruan DY, Jia CC et al (2019) Controlling nutritional status (CONUT) score-based nomogram to predict overall survival of patients with HBV-associated hepatocellular carcinoma after curative hepatectomy. Clin Transl Oncol. https://doi.org/10.1007/s12094-019-02137-4
Toyokawa G, Kozuma Y, Matsubara T et al (2017) Prognostic impact of controlling nutritional status score in resected lung squamous cell carcinoma. J Thorac Dis 9(9):2942–2951
Shoji F, Haratake N, Akamine T et al (2017) The preoperative controlling nutritional status score predicts survival after curative surgery in patients with pathological Stage I non-small cell lung cancer. Anticancer Res 37(2):741–747
Amin MB, Greene FL, Byrd DR et al (2016) AJCC cancer staging manuel, 8th edn. Springer International Publishing, Berlin, pp 1–1024
World Health Organization (2020) https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 5 Jan 2020
Bernhardt D, Aufderstrasse S, König L et al (2018) Impact of inflammatory markers on survival in patients with limited disease small-cell lung cancer undergoing chemoradiotherapy. Cancer Manag Res 30(10):6563–6569
Duan J, Pan L, Yang M (2018) Preoperative elevated neutrophil-to-lymphocyte ratio (NLR) and derived NLR are associated with poor prognosis in patients with breast cancer: a meta-analysis. Medicine (Baltimore) 97(49):e13340. https://doi.org/10.1097/MD.0000000000013340
Vartolomei MD, Porav-Hodade D, Ferro M et al (2018) Prognostic role of pretreatment neutrophil-to-lymphocyte ratio (NLR) in patients with non-muscle-invasive bladder cancer (NMIBC): a systematic review and meta-analysis. Urol Oncol 36(9):389–399
Yu Y, Qian L, Cui J (2017) Value of neutrophil-to-lymphocyte ratio for predicting lung cancer prognosis: a meta-analysis of 7,219 patients. Mol Clin Oncol 7(3):498–506
Lohinai Z, Bonanno L, Aksarin A et al (2019) Neutrophil-lymphocyte ratio is prognostic in early stage resected small-cell lung cancer. PeerJ 29(7):e7232. https://doi.org/10.7717/peerj.7232
Zhang Y, Chen B, Wang L et al (2019) Systemic immune-inflammation index is a promising noninvasive marker to predict survival of lung cancer: a meta-analysis. Medicine (Baltimore) 98(3):e13788. https://doi.org/10.1097/MD.0000000000013788
Hong X, Cui B, Wang M et al (2015) Systemic ımmune-inflammation ındex, based on platelet counts and neutrophil-lymphocyte ratio, ıs useful for predicting prognosis in small cell lung cancer. Tohoku J Exp Med 236(4):297–304
Nazha B, Moussaly E, Zaarour M et al (2015) Hypoalbuminemia in colorectal cancer prognosis: nutritional marker or inflammatory surrogate? World J Gastrointest Surg 27 7(12):370–377
Saito H, Kono Y, Murakami Y et al (2017) Influence of prognostic nutritional index and tumor markers on survival in gastric cancer surgery patients. Langenbecks Arch Surg 402(3):501–507
Zhang W, Ye B, Liang W et al (2017) Preoperative prognostic nutritional index is a powerful predictor of prognosis in patients with stage III ovarian cancer. Sci Rep 25 7(1):9548
Wang Z, Wang Y, Zhang X et al (2018) Pretreatment prognostic nutritional index as a prognostic factor in lung cancer: review and meta-analysis. Clin Chim Acta 486:303–310
Lipschitz DA (1988) Protein-energy malnutrition. Hosp Pract (Off Ed) 15 23(11):87–99
Harimoto N, Yoshizumi T, Sakata K et al (2017) Prognostic significance of preoperative controlling nutritional status (CONUT) score in patients undergoing hepatic resection for hepatocellular carcinoma. World J Surg 41(11):2805–2812
Lin ZX, Ruan DY, Li Y et al (2015) Lymphocyte-to-monocyte ratio predicts survival of patients with hepatocellular carcinoma after curative resection. World J Gastroenterol 21(38):10898–10906
Khan AUH, Allende-Vega N, Gitenay D et al (2017) The PDK1 ınhibitor dichloroacetate controls cholesterol homeostasis through the ERK5/MEF2 pathway. Sci Rep 6 7(1):10654
Toyokawa T, Kubo N, Tamura T et al (2016) The pretreatment controlling nutritional status (CONUT) score is an independent prognostic factor in patients with resectable thoracic esophageal squamous cell carcinoma: results from a retrospective study. BMC Cancer 6(16):722
Kuroda D, Sawayama H, Kurashige J et al (2018) Controlling nutritional status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer 21(2):204–212
Ohba T, Takamori S, Toyozawa R et al (2019) Prognostic impact of the controlling nutritional status score in patients with non-small cell lung cancer treated with pembrolizumab. J Thorac Dis 11(9):3757–3768
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The local ethics committee approved the study protocol.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yılmaz, A., Tekin, S.B., Bilici, M. et al. The Significance of Controlling Nutritional Status (CONUT) Score as a Novel Prognostic Parameter in Small Cell Lung Cancer. Lung 198, 695–704 (2020). https://doi.org/10.1007/s00408-020-00361-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-020-00361-2