Abstract
Purpose
Previous studies with small sample sizes have shown a wide range of complication rates and no study has investigated the yield of computed tomography-guided transthoracic core needle biopsies (CTTCB) for coccidioidomycosis. To better assess the safety, accuracy, and risk factors for complications of CTTCB of pulmonary nodules, we conducted a retrospective study at a high-volume academic center in an endemic coccidioidomycosis area.
Methods
We conducted a retrospective study of 203 patients who underwent CTTCB of pulmonary nodules between December 2010 and May 2013. We collected demographics, clinical, and radiographic data. Each case was reviewed for complications. Diagnostic accuracy was assessed by comparing CTTCB with final diagnoses.
Results
The overall complication rate was 25 %. Pneumothorax accounted for 24 % of complications with 7 % of pneumothoraces requiring chest tube. 1.5 % were complicated by hemoptysis but none required blood transfusions. There was an association between complications and age, presence of emphysema on CT, traversed lung length, and lesion depth. The overall sensitivity of the CTTCB for all types of lung cancer was 93 %, and specificity of 100 %. The positive predictive value of CTTCB for lung cancer was 100 %. The sensitivity and specificity of CTTCB for a coccidiomycosis lung nodule was 83 % with a specificity of 100 % with a PPV of 100 %.
Conclusion
Our study demonstrates that CTTCB is a relatively safe method for evaluating lung nodules and highly accurate in evaluating lung nodules due to coccidioidomycosis in an endemic area. The primary risk factors for complications from CTTCB are the presence of emphysema on CT scan, lesion depth, and traversed lung length.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With the advent of low-dose chest computerized tomographic (CT) screening, the number of solitary pulmonary nodules (SPN) is likely to increase. Because of the underlying risk for lung cancer, histological evaluation of SPN is often required. While positron emission tomography (PET)/CT is recommended for initially evaluating moderate risk SPN [1], PET/CT may not be appropriate in some endemic fungal areas because of high false positive rates [2, 3]. Transthoracic needle biopsy of SPN has a diagnostic yield of up to 97 % for malignancy [4]. Originally, transthoracic needle biopsies were performed using single plane fluoroscopy and fine needle aspiration [5, 6]. In the last decade, more centers have been performing computed tomography-guided transthoracic core needle biopsies (CTTCB) [1, 7]. CTTCB is currently recommended for peripheral SPN when clinical and imaging findings are discordant or when a benign diagnosis that requires specific medical treatment is suspected [1].
CTTCB is generally a safe procedure with limited morbidity and rare mortality [1, 7]. Pneumothorax (15–34 % incidence) and hemoptysis (4–25 % incidence) are the most common complications of CTTCBs [4, 8–19]. A recent, retrospective cross-sectional analysis reported a pneumothorax rate of 24 % and hemorrhage rate of 1 %. However, this study did not distinguish between core needle biopsies and fine needle aspiration and was based on discharge records and medical coding of complications rather than review of individual patient records [8]. Diagnostic yield and complications may vary based on both the patient population and the volume of procedures being performed. Prior published series of CTTCB were limited in that more than half of the studies included fewer than 200 procedures, many did not report risk factors for complications, and none were performed in an endemic area for coccidioidomycosis [4, 8–19].
Our study was designed to evaluate complications and diagnostic yield of CTTCB in a high-volume center in a coccidioidomycosis endemic region. Because of the false positive rates in PET/CT for granulomatous infections and coccidioidomycosis specifically, we commonly perform CCTTB in our patients with peripheral SPN. Our center is among the top 10 % of institutions in the state of California and top 26 % in the United States of America in annual number of CTTCBs performed [8]. This is the first study to specifically address complication rates and diagnostic yield for CCTTB in an area endemic for coccidioidomycosis.
Methods
We conducted a retrospective study of transthoracic needle biopsies for lung nodules performed at Community Medical Centers (CMC) in Fresno, CA. The study was reviewed and approved by the CMC Institutional Review Board (Approval #: 2011075).
Patients
We reviewed medical records of all patients seen in a multidisciplinary lung nodule program who underwent CTTCBs between December 2010 and May 2013. The decision to perform a CTTCB was made by consensus of a multidisciplinary team consisting of radiologist, pulmonologist, oncologist, and thoracic surgery based on clinical and radiographic characteristics. We identified 203 patients with biopsy proven malignancy or proven or probable coccidioidomycosis. A final diagnosis for cancer was made on histological grounds. Proven coccidioidomycosis was defined as positive cultures for Coccidioides or by morphologic identification of Coccidioides from pulmonary samples. Probable coccidioidomycosis was diagnosed based on finding granulomatous inflammation on the biopsy and a clinical course compatible with coccidioidomycosis including radiographic stability, improvement, or resolution over a two-year period.
Procedure
All biopsies were performed by board-certified radiologists using a commercially available helical multidetector-row CT scanner.
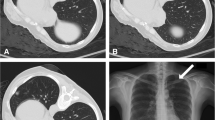
The biopsies were performed using a coaxial technique with an outer 17–19-gage thin-wall coaxial introducer needle 10–20 cm long. Core biopsies were performed with an 18–20-gage automated cutting needle biopsy gun (Temno systems; Cardinal Health; Dublin, OH) through the introducer needle. Needle positioning was confirmed using CT fluoroscopy. Patients were monitored for 2 h after the biopsy, and pneumothorax was documented on an immediate post-biopsy CT and on an upright postero-anterior expiratory chest radiograph obtained 1 h after biopsy. Symptomatic or expanding pneumothoraces were treated with nasal oxygen and thoracostomy tube insertion and some were admitted for observation. In addition, any hemorrhages resulting in hemoptysis and/or requiring blood transfusions were recorded.
Definitions and Selection of Study Variables
Data were abstracted by trained staff using a standardized approach. Data abstracted included age, gender, history of chronic lung disease (CLD), tobacco use, nodule size, nodule location, body mass index (BMI), and emphysema seen on CT scan, length of lung parenchyma traversed, and lesion depth of each patient. Pneumothoraces were categorized as either requiring treatment with thoracostomy tube or not requiring treatment. Hemorrhage was categorized as patients who developed hemoptysis or required blood transfusions. History of CLD was defined as asthma or chronic obstructive pulmonary disease (COPD) based on patient history. Tobacco use was categorized as current smoker, ex-smoker, or never smoker. Emphysema was defined as emphysematous on CT and nodule size and location were abstracted from radiologist’s report. The length of lung parenchyma traversed was defined as the distance from the pleural puncture site to the nearest edge of the lesion. The lesion depth was defined as the distance from the skin puncture site to the nearest edge of the lesion on CT images. These measurements were made from the biopsy images captured at the time of the procedure.
Statistical Analysis
Frequency distributions were prepared and examined on all variables and data were carefully reviewed for statistical outliers. Cross tabulations were completed to assess the correlation between CLD, gender, nodule location, tobacco history, and the occurrence of complications. To assess associations among categorical variables, Pearson’s χ 2 test was used and Student’s t test was used to compare means of different groups. Logistic regression analysis was performed to evaluate associations between traversed lung length or depth of lesion and the occurrence of complications. A receiver operating characteristic (ROC) analysis was conducted to determine that point of traversed distance which produced the highest sensitivity for avoiding complications. All statistical analyses were performed using IBM/SPSS software, version 21.0 (SSPS, Chicago, IL, USA). Two-sided tests were used, and a p value ≤ 0.05 was considered statistically significant.
Results
We evaluated a total of 203 CTTCBs of which 164 (81 %) nodules were malignant and 39 (19 %) were due to coccidioidomycosis. The demographics of these patients are shown in Table 1.
The overall complication rate was 25 % (51/203). The most common complication was pneumothorax. Hemorrhage was uncommon and no patient required transfusion (Table 2). Neither gender, BMI, tobacco history, history of chronic lung disease, nodule size, nor nodule location was associated with complications (Table 3).
Age was significantly associated with complications. The average age for those with complications was 66 years as compared to 60 years for those without complications (p = 0.007), (Table 3).
While a history of chronic lung disease was not associated with complications, the presence of emphysema on CT was significantly associated with complications. While 17 % of all patients (35/203) had emphysema on CT scan, 33 % of patients with complications had emphysema on CT scan (p value < 0.01). The odds ratio (OR) for complications with emphysema was 2.97 (95 % CI 1.40–6.29).
The mean traversed lung length and lesion depth were independently associated with pneumothorax and hemorrhage (Table 3). For patients with pneumothorax, the mean lesion depth was 92.9 ± 28.2 mm as compared to 57.6 ± 29.2 mm for those without a pneumothorax (p < 0.001), and the mean traversed lung length was 28.9 ± 18.6 mm for those with pneumothorax compared with 21.1 ± 19.2 mm for those without pneumothorax (p = 0.002). The OR for a pneumothorax with increasing lesion depth (in mm) was 1.03 per mm (95 % CI 1.021–1.044) and was 1.02 (95 % CI 1.004–1.036) for traversed lung length. For patients with hemorrhage, the mean lesion depth was 95.5 ± 27.1 mm as compared to 64.5 ± 32.6 mm for those without hemorrhage (p < 0.001), and the traversed lung length was 30.0 ± 20.6 mm as compared with 19.5 ± 18.8 mm for those with and without hemorrhage (p = 0.003). The OR for hemorrhage with increasing lesion depth (in mm) was 1.025 per mm (95 % CI 1.007–1.042) and was 1.02 (95 % CI 0.988–1.045) for traversed lung length. The OR for any complication with increasing lesion depth (in mm) was 1.04 per mm (95 % CI 1.028–1.052) and was 1.024 (95 % CI 1.008–1.041) for traversed lung length.
To evaluate this relationship further, we developed an ROC curve for lesion depth and traversed lung length and obtained inflection points from these curves. For lesion depth, the area under the curve (AUC) was 0.69 (p < 0.0001) and the inflection point was 68 mm (Fig. 1). Patientts with lesion depth of ≥68 mm had an overall complication rate of 61 % and those with <68 mm had a complication rate 8 % (p < 0.001). For the traversed lung length ROC, the AUC was 0.86 (p < 0.0001) and the inflection point was 20.5 mm (Fig. 2). The overall complication rate for traversed lung length ≥20.5 mm was 48 % compared to 18 % for traversed lung length <20.5 mm (p < 0.001).
The overall sensitivity of the CT-guided biopsy for all types of lung cancer was 93 %, with a specificity of 100 %. The positive predictive value of a CTTCB for lung cancer was to be 100 %. The sensitivity and specificity of CTTCB for proven and probable coccidioidomycosis infectious lung nodule was 83 % with a specificity of 100 % and a PPV of 100 %. These results are based only on biopsies with a histological diagnosis.
Discussion
With the increased use of chest CT and the advent of lung cancer screening, the finding of pulmonary nodules is likely to increase. Screening studies of smokers who are at high risk of malignancy find that most nodules identified on CT are benign, however, management of indeterminate pulmonary nodules is a diagnostic challenge [20]. Patients and clinicians must decide on the risk benefit for nodule biopsy.
In the National Lung Screening Trial, 96 % of nodules were false positive but 11 % of the positive results led to an invasive study [20]. Current guidelines propose FDG-PET for intermediate probability solitary pulmonary nodules >8 mm. FDG-PET has been shown to differentiate benign from malignant lesions; however, infectious, inflammatory, or granulomatous nodules can yield a false positive [21]. In fact, in an endemic coccidioidomycosis area, FDG-PET was positive in 86 % of coccidioidomycosis nodules with a standardized uptake value (SUV) >2.5 in almost half [22]. These observations highlight the need to adapt guidelines to local conditions and have led us to often use CTTCB.
Until the mid 1960s, most of the limited diagnostic procedures for pulmonary nodules had such a low-specific diagnostic yield that the clinician had essentially two choices: recommend diagnostic thoracotomy, or observe with repeated X-ray examinations [23]. In 1973, Zelch et al. showed that needle aspiration biopsies for pulmonary nodules with the use of fluoroscopy had a significantly better diagnostic yield and was easier to perform than the older bronchial brushing approach [24]. With the advent of CT, fine needle aspiration became the most commonly used method because it not only had a better diagnostic yield, but also made it possible to biopsy smaller and previously less accessible lesions with low complication rates [25]. Needle core biopsy techniques are now preferred to fine needle aspiration for both benign and malignant diagnoses. Core biopsies provide histologic architecture improving our ability to identify benign diagnoses. In addition, larger biopsy samples provide for additional immunohistochemical and mutational analysis in malignancy. Larger core biopsy samples also reduce the number of punctures required and have a higher diagnostic yield. The difference in complication rates between core needle biopsy and fine needle aspiration varies by studies [26].
Prior studies of transthoracic needle biopsies done in the American Southwest were done with fluoroscopic guidance and fine needle aspiration [6]. To our knowledge, our study is the first study of CT-guided core biopsies in patients at high risk for coccidioidomycosis. Our overall complication rate was 25 %, similar to other large studies. Twenty-four per cent of our patients had a pneumothorax but only 7 % required chest tube, and 1 % had hemorrhage but none required transfusion. This complication rate is similar to other large studies, but significantly lower than small case studies. [5, 11, 17, 18].
We evaluated predictors for complications from CTTCB. Many clinical risks including gender, smoking history, presence of chronic lung disease by history, nodule size, and patient BMI were not associated with complications. However, age was an identified risk factor in our population in contrast to prior studies [10, 11, 16, 17], and may reflect the younger patients in our cohort with coccidioidomycosis. While a history of chronic lung disease was not associated with complications, we did find an association between the presence of emphysema on CT scan and complications with a 2–3-fold increase in complications in patients with emphysema.
Unlike some earlier studies, we did not find an association between nodule size or nodule location with complications [4, 10–14, 16–18]. However, one novel finding in our study was the non-linear relationship between lesion depth from skin or from the pleura. Lesion depth is the sum of two elements; depth of soft tissue to the pleura and distance from the pleura to the lesion. Prior studies have shown both to be associated with complications and our study confirms that the increased lesion depth and lung parenchyma traversed increases the risk of pneumothorax and hemorrhage in patients undergoing CTTCB. In a linear analysis of our data, we did find that a 4 % increase in complications with each mm lesion depth and a 2.4 % increase in complications for each mm increase in traversed lung length. However, we felt it would be unlikely that complications will be linear in their relationship to lesion depth and traversed lung depth. To address this, we analyzed the data using an ROC curve. This type of analysis allows us to improve our ability to identify the threshold beyond which complication risk increases. We found that a lesion depth ≥68 mm and traversed lung length ≥20.5 mm defined points with a significant difference in complications. To our knowledge, this is the first time that complications from CTTCB have been analyzed in this way, and we feel is a more realistic method for determining risk. Interestingly, using BMI as a surrogate for soft tissue depth revealed no significant association with complications.
Our study was performed in an endemic coccidioidomycosis area and it is the first study to investigate the accuracy of CTTCB in diagnosing pulmonary nodules due to coccidioidomycosis. Prior studies employed the use of needle aspiration biopsies and plain X-rays for guidance [6, 27]. By comparing the histologic specimen from CTTCB with the clinic diagnosis, we found sensitivity to be 83 % with a specificity of 100 % and PPV of 100 %. We calculated the overall accuracy of CTTCB for coccidioidomycosis by careful definition using pathology and microbiology. We found that CTTCB is highly sensitive and specific for malignancy, consistent with most studies [9, 10, 28]. The sensitivity and specificity were calculated using only biopsies with a histological diagnosis.
There were some limitations of our study. One is that this is a retrospective study that depended on collection of clinical data from the patient record. However, we have standardized the collection of clinical risk factors for lung cancer in our clinic, and we reviewed all of the CT scans to confirm radiographic measurements. In addition, our diagnostic accuracy for coccidioidomycosis was made by positive cultures, identification of the organism on pathology, or presence of granulomatous inflammation with a consistent clinical course.
Our study demonstrates that CTTCB is a relatively safe method for evaluating lung nodules in our endemic region. The primary risk factors for complications from CTTCB are the presence of emphysema on CT scan, lesion depth, and traversed lung length. In addition, we demonstrate CTTCB is a relatively safe and highly accurate method of evaluating lung nodules due to coccidioidomycosis in an endemic area.
References
Gould MK, Donington J, Lynch WR et al (2013) Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143(5Suppl):e93S–e120S
Croft DR, Trapp J, Kernstine K et al (2002) FDG-PET imaging and the diagnosis of non-small cell lung cancer in a region of high histoplasmosis prevalence. Lung Cancer 36(3):297–301
Reyes N, Onadeko OO, Luraschi-Monjagatta MD et al (2014) Positron emission tomography in the evaluation of pulmonary nodules among patients living in a coccidioidal endemic region. Lung 192(4):589–593
Khan MF, Straub R, Moghaddam SR et al (2008) Variables affecting the risk of pneumothorax and intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur Radiol 18(7):1356–1363
Wiener RS, Wiener DC, Gould MK (2013) Risks of transthoracic needle biopsy: how high? Clin Pulm Med 20(1):29–35
Forseth J, Rohwedder JJ, Levine BE et al (1986) Experience with needle biopsy for coccidioidal lung nodules. Arch Intern Med 146(2):319–320
Loubeyre P, Copercini M, Dietrich PY (2005) Percutaneous CT-guided multisampling core needle biopsy of thoracic lesions. Am J Roentgenol 185(5):1294–1298
Wiener RS, Schwartz LM, Woloshin S et al (2011) Population-based risk for complications after transthoracic needle lung biopsy of a pulmonary nodule: an analysis of discharge records. Ann Intern Med 155(3):137–144
Montaudon M, Latrabe V, Pariente A et al (2004) Factors influencing accuracy of CT-guided percutaneous biopsies of pulmonary lesions. Eur Radiol 14(7):1234–1240 Epub 2004 Feb 13
Heyer CM, Reichelt S, Peters SA et al (2008) Computed tomography-navigated transthoracic core biopsy of pulmonary lesions: which factors affect diagnostic yield and complication rates? Acad Radiol. 15(8):1017–1026
Yeow KM, Su IH, Pan KT et al (2004) Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest 126(3):748–754
Li Y, Du Y, Yang HF et al (2013) CT-guided percutaneous core needle biopsy for small (≤20 mm) pulmonary lesions. Clin Radiol 68(1):e43–e48
Covey AM, Gandhi R, Brody LA et al (2004) Factors associated with pneumothorax and pneumothorax requiring treatment after percutaneous lung biopsy in 443 consecutive patients. J Vasc Interv Radiol 15(5):479–483
Chakrabarti B, Earis JE, Pandey R et al (2009) Risk assessment of pneumothorax and pulmonary haemorrhage complicating percutaneous co axial cutting needle lung biopsy. Respir Med 103(3):449–455
Yildirim E, Kirbas I, Harman A et al (2009) CT-guided cutting needle lung biopsy using modified coaxial technique: factors effecting risk of complications. Eur J Radiol 70(1):57–60
Saji H, Nakamura H, Tsuchida T et al (2002) The incidence and the risk of pneumothorax and chest tube placement after percutaneous CT-guided lung biopsy: the angle of the needle trajectory is a novel predictor. Chest 121(5):1521–1526
Yamagami T, Nakamura T, Iida S et al (2002) Management of pneumothorax after percutaneous CT-guided lung biopsy. Chest 121(4):1159–1164
Kothary N, Lock L, Sze DY et al (2009) Computed tomography-guided percutaneous needle biopsy of pulmonary nodules: impact of nodule size on diagnostic accuracy. Clin Lung Cancer. 10(5):360–363
Hiraki T, Mimura H, Gobara H et al (2009) CT fluoroscopy-guided biopsy of 1,000 pulmonary lesions performed with 20-gauge coaxial cutting needles: diagnostic yield and risk factors for diagnostic failure. Chest 136(6):1612–1617
Williams A, Tammemagi MC et al (2013) Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med 369(10):910–919
Vansteenkiste JF, Stroobants SS (2006) PET scan in lung cancer: current recommendations and innovation. J Thorac Oncol 1(1):71–73
Reyes N, Onadeko OO et al (2014) Positron emission tomography in the evaluation of pulmonary nodules among patients living in a coccidioidal endemic region. Lung 192(4):589–593
Neff TA (1973) To needle, brush, cut or watch? Chest 63(2):134
Zelch JV, Lalli AF, McCormack LJ et al (1973) Aspiration biopsy in diagnosis of pulmonary nodule. Chest 63(2):149–152
VanSonnenberg E, Casola G, Ho M et al (1988) Difficult thoracic lesions: CT-guided biopsy experience in 150 cases. Radiology 167(2):457–461
Choi SH, Chae EJ et al (2013) Percutaneous CT-guided aspiration and core biopsy of pulmonary nodules smaller than 1 cm: analysis of outcomes of 305 procedures from a tertiary referral center. Am J Roentgenol 201(5):964–970
Chitkara YK (1997) Evaluation of cultures of percutaneous core needle biopsy specimens in the diagnosis of pulmonary nodules. Am J Clin Pathol 107(2):224–228
Anderson JM, Murchison J, Patel D (2003) CT-guided lung biopsy: factors influencing diagnostic yield and complication rate. Clin Radiol 58(10):791–797
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors wish to declare that there is no conflict of financial or personal interest related to this manuscript.
Rights and permissions
About this article
Cite this article
Sachdeva, M., Ronaghi, R., Mills, P.K. et al. Complications and Yield of Computed Tomography-Guided Transthoracic Core Needle Biopsy of Lung Nodules at a High-Volume Academic Center in an Endemic Coccidioidomycosis Area. Lung 194, 379–385 (2016). https://doi.org/10.1007/s00408-016-9866-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-016-9866-3