Abstract
Background
Patients with idiopathic pulmonary fibrosis (IPF) have severely limited exercise capacity due to dyspnea, hypoxemia, and abnormal lung mechanics. This pilot study was designed to determine whether pulmonary rehabilitation were efficacious in improving the 6-min walk test (6-MWT) distance, exercise oxygen uptake, respiratory muscle strength [maximum inspiratory pressure (MIP)], and dyspnea in patients with IPF. Underlying physiological mechanisms and effects of the intervention were investigated.
Methods
Subjects were randomly assigned to a 3-month pulmonary rehabilitation program (n = 11) or to a control group (n = 10). All subjects initially underwent the 6-MWT and constant load exercise gas exchange studies.
Results
Subjects in the rehabilitation group increased treadmill exercise [metabolic equivalent of task-minutes] over the first 14 sessions. Beneficial effects on physical function resulted in those who completed rehabilitation. Subjects who completed the program increased cycle ergometer time and maintained exercise oxygen consumption (exercise VO2) at the baseline level over 3 months, while the control group suffered a significant decrease in exercise VO2. Rehabilitation subjects also increased their MIP. Plasma lactate doubled and brain natriuretic peptide levels increased significantly after exercise, as did the plasma amino acids glutamic acid, arginine, histidine, and methionine. These changes were associated with significant decreases in arterial oxygen saturation and increases in 15-F2t-isoprostanes after exercise.
Conclusions
Pulmonary rehabilitation effectively maintained exercise oxygen uptake over 3 months and lengthened constant load exercise time in patients with moderately severe IPF. Exercise endurance on cycle ergometry testing was limited by dyspnea and severe hypoxemia associated with systemic oxidant stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic pulmonary fibrosis (IPF) is an often fatal process characterized by onset in middle age, progressive scarring of the lungs in a usual interstitial pneumonia (UIP) pattern, and the absence of systemic disease that would explain lung scarring [1]. No therapies, save lung transplantation, are effective in prolonging lives of IPF patients [2].
Exercise limitation, accompanied by dyspnea, is the cardinal manifestation of IPF [3]. Abnormal lung mechanics limit ventilatory adaptation to exercise and often lead to a less efficient, rapid, and shallow breathing pattern [4]. Pulmonary hypertension is also present in nearly one half of transplant-candidate IPF patients who undergo cardiac catheterization [5]. Increased pulmonary vascular resistance in IPF appears to be poorly amenable to therapy [6].
Both chronic and intermittent hypoxia impair skeletal muscle function through a number of mechanisms, including oxidative enzyme inhibition, amino acid efflux, and increased production of reactive nitrogen and oxygen species (ROS) [7]. Systemic oxidant stress occurs during low-level exercise in IPF patients, as we have shown by increased urine 15-F2t-isoprostanes (isoprostanes) and decreased plasma total antioxidant capacity [8].
Pulmonary rehabilitation, defined as a variable combination of aerobic and strengthening exercises, quite clearly improves 6-min walk test (6-MWT) distance and well-being in patients with chronic obstructive pulmonary diseases (COPD) [9]. High-quality data showing similar benefits in IPF patients are sparse [10–12]. A recent retrospective study of 402 patients with interstitial lung disease (50 % had IPF) showed that intense inpatient rehabilitation resulted in a 46 ± 3 (SEM)-m average increase in 6-MWT distance [13].
Our goals for this study were to test whether outpatient pulmonary rehabilitation for 12 weeks improved 6-MWT distance, exercise oxygen consumption (exercise VO2), treadmill exercise [metabolic equivalent of task (MET)-minutes], maximum inspiratory pressure (MIP), and dyspnea (Borg dyspnea index) in subjects who met all contemporary criteria for IPF [14].
Methods
Study Participants
This study was approved by the Miami Veterans Affairs Health System Institutional Review Board. This study is registered as clinicaltrials.gov Identifier: NCT01118221.
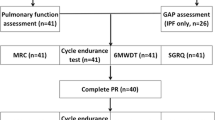
IPF cases were defined according to American Thoracic Society–European Respiratory Society (ATS-ERS) clinical diagnostic criteria [14]. Inclusion and exclusion criteria are presented in Table 1. Patients were screened by echocardiography at rest to estimate right ventricular systolic pressure (RVSP) [15]. High-resolution computed tomography (HRCT) scans of the chest were required to show a UIP pattern [16]. The distribution of subjects who were screened and randomized is shown in the CONSORT diagram presented in Fig. 1.
Selection and disposition of subjects. We screened 72 IPF patients for eligibility and enrolled 25. Fourteen were assigned to rehabilitation and 11 to the control (observation only) group. Two rehabilitation subjects and one control subject chose to leave the trial. One rehabilitation subject died of respiratory failure during the trial. Twenty-one subjects completed the trial and their data are presented here
Experimental Design
The study was designed as a randomized, controlled, nonblinded, pilot study of the effects of pulmonary rehabilitation. The prespecified primary outcome measure of the clinical trial was the 6-MWT distance.
Exercise Testing
We used an Oxycon™ Mobile portable unit (CareFusion, San Diego, CA, USA) to measure sustained exercise VO2 and other gas exchange variables, while subjects exercised to their volitional limit at a constant load on an exercise cycle (Life Cycle 65R, Life Fitness, Schiller Park, IL, USA) [17]. This approach has been used to assess the effects of nonpharmacological interventions in patients with respiratory disease [18–20]. V E/VCO2 slope values, acquired from the initiation to peak exercise, were calculated using least-squares linear regression [21]. Heart rate reserve (HRR) was calculated as maximum predicted heart rate (220 − age in years/min) minus the actual peak heart rate recorded during exercise [3, 4]. Before (resting) and immediately after (post-exercise) constant-load cycle ergometry at 50 W, plasma (15-F2t-isoprostanes, lactate, NT-proBNP, and AA) and urine (15-F2t-isoprostanes and creatinine) samples were collected, processed, and frozen at −80 °C.
Pulmonary Function Tests
The maximum voluntary ventilation (MVV) was calculated as 35× FEV1 [in L (liters)] [3, 4]. Maximum inspiratory (MIP) and expiratory (MEP) pressures were measured as previously described [22].
6-Min Walk Test Protocol
The 6-MWT was done and monitored as previously described [23]. Before and after the test, we recorded heart rate, oxygen saturation, and the Borg Dyspnea Index (BDI) [24].
Rehabilitation Program
Subjects in the rehabilitation group completed 24 twice-weekly 2-h rehabilitation sessions over 12 weeks. Control subjects did not participate in a rehabilitation program. Supplemental nasal oxygen was provided from a compressed gas source during exercise training to maintain SpO2 above 88 %. Treadmill and cycling exercises were initiated at 60–80 % of the predicted maximum heart rate based on age. MET-minutes for each session were estimated and recorded [25]. Details of the rehabilitation program are presented in Table 2. Perceived breathlessness on exertion was recorded using the modified BDI before and after each exercise modality [24].
Biochemical Analyses
We quantified 15-F2t-isoprostanes in plasma and urine using high-performance liquid chromatography (HPLC) tandem mass spectroscopy (MS–MS), as previously described [26, 27]. We assayed plasma free amino acids (AA) by liquid chromatography–mass spectroscopy (LC–MS) using the EZ:faast Assay (Phenomenex®, Torrance, CA, USA). The concentration of lactate in plasma samples obtained before and after exercise was measured using standard techniques [28]. Amino terminal pro-brain natriuretic peptide (NT-proBNP) was assayed in plasma using the procedure described by Elin and Winter [29].
Statistical Analyses
Paired t-tests or Wilcoxon signed-rank tests were used for within-group comparisons, whereas independent-sample t-tests or Mann–Whitney tests were used for between-group comparisons. A generalized linear model was used to analyze trends in treadmill MET-minutes [30]. Statistical significance was defined as P < 0.05.
Results
Characteristics and Disposition of the Subjects
The participants’ baseline characteristics are presented in Table 3. At the time of enrollment, subjects had mild to moderate restriction of lung volumes (mean ± SD FVC = 61 ± 12 % of predicted) and moderate to severe diffusion impairment (mean DLCO = 44 ± 10 % of predicted). Eight of 11 rehabilitation and 3 of 10 control subjects were taking empirical N-acetyl-l-cysteine (600 mg orally three times daily) at the time of enrollment [1].
Baseline Response to Cycle Ergometry Testing
During the initial cycle ergometry, the 21 subjects achieved on average 63 ± 3 (SEM) % of their predicted MVV. The average maximum heart rate during cycle ergometry testing at baseline evaluation reached 68 ± 3 (SEM) % of predicted, and the HRR at maximum achieved exercise averaged 49 ± 2/min.
Plasma and Urine Isoprostanes
The baseline mean plasma concentration of 15-F2t-isoprostanes was 16.5 ± 2.3 (SEM) pg/mL. Immediately after cycle ergometry to measure exercise VO2, the concentration of 15-F2t-isoprostanes increased significantly to 18.0 ± 12.2 pg/mL (P = 0.028). At baseline, the mean concentration of 15-F2t-isoprostanes in urine (normalized to creatinine) was 336 ± 43 (SEM) pg/mg creatinine. Urine isoprostane concentration did not change significantly after cycle ergometry from baseline (post exercise testing, 345 ± 46; P = 0.746).
Plasma Lactate
Plasma lactate increased significantly, more than doubling (+108 %), after ergometry from baseline (pre-exercise test, 1.3 ± 0.1 [SEM] mM; post-exercise test, 2.7 ± 0.2; P = 0.001).
Brain Natriuretic Peptide
NT-proBNP also increased significantly (+11 %) after the baseline cycle ergometry exercise test (pre-exercise test, 81 ± 19 [SEM] pg/mL; post-exercise test, 90 ± 20; P = 0.012).
Oxygenation
At baseline, mean SpO2 in the subjects was 95 ± 1 (SEM) %. SpO2 decreased uniformly and significantly to 86 ± 2 % (P < 0.001) at the conclusion of exercise testing while breathing room air. Plasma oxygen saturation, plasma lactate, 15-F2t-isoprostanes, and NT-proBNP data are summarized in Fig. 2 for subjects before and after the 3-month protocol.
Overall effects of cycle ergometry exercise testing (~50-W exercise) on arterial oxygen saturation, plasma lactate, 15-F2t-isoprostanes, and NT-proBNP at baseline. Data shown were obtained at baseline (i.e., before any intervention) from all subjects who completed the 3-month study. a SpO2. b Plasma lactate. c Plasma 15-F2t-isoprostanes. d NT-proBNP. Box-whisker plots display distribution of the data as the median (line in box), 25th and 75th percentiles (box), and 5th and 95th percentiles (error bars) for all subjects before (Pre 0) and after (Post 0) the baseline cycle ergometry test. *P < 0.05 for the pre-ergometry data compared to the post-ergometry data
Plasma Amino Acid Concentrations
Glutamic acid (GLU) concentration in the plasma more than doubled (+113 %). This increase was accompanied by significant but smaller increases in the concentrations of arginine (ARG) (+10 %), aspartic acid (ASP) (+47 %), histidine (HIS) (+32 %), and methionine (MET) (+24 %). These data are summarized in Table 4. Importantly, among those subjects who were not taking N-acetyl-l-cysteine, the [cysteine]/[cystine] ratio decreased by 72 % after exercise. These data are summarized in Table 5.
Effects of Rehabilitation on Cycle Ergometry Exercise Testing
After 3 months, VO2 during exercise, a prospectively chosen end point, remained stable in the rehabilitation group, whereas it decreased significantly (−13 %; P = 0.027) over that time in the control group. These data are shown in Fig. 3. Completion of the rehabilitation program significantly increased exercise time from 184 ± 28 (SEM) to 302 ± 62 s (P = 0.036) among those subjects who did not reach a steady state exceeding 10 min during cycle ergometry testing at 50 W. In contrast, exercise time did not change in controls over the 3-month observation period (baseline, 141 ± 29 s, 3-month, 137 ± 36 s; P = 0.762).
Subjects in rehabilitation program maintained exercise VO2 at baseline. We measured exercise oxygen uptake (exercise VO2) during cycle ergometry exercise testing at baseline (solid gray bars) and again after 3 months (cross hatched bars) of rehabilitation (Rehabilitation) or observation (Control). Data shown are the mean ± SEM exercise oxygen consumption (mL/min) measurements in the rehabilitation and control groups at baseline and at 3 months. Exercise VO2 did not change over 3 months in the rehabilitation group, while it decreased significantly in controls; *P < 0.05
Effects of Rehabilitation on Treadmill Walking and Exercise Cycling
Rehabilitation subjects (n = 11) achieved 65 ± 2 (SEM) % of their predicted maximum heart rate on the treadmill and 66 ± 2 % on the exercise cycle during the twice-weekly rehabilitation sessions. The intensity of treadmill exercise increased significantly during the initial 14 rehabilitation sessions. These data are summarized graphically in Fig. 4.
Treadmill exercise MET-minutes during the 24 rehabilitation sessions. We recorded MET-minutes of treadmill exercise (shown by the solid blue line) for each rehabilitation subject (n = 11) at each of the 24 sessions. Data shown are arithmetic means ± SEM (MET-minutes) for the subjects during each rehabilitation session. Sessions occurred twice weekly over 3 months. The subjects increased treadmill exercise as reflected by mean MET-minutes during the initial 14 sessions (linear trend P < 0.05), but they appeared to reach a plateau in the latter sessions (15–24) of rehabilitation
Effects of Rehabilitation or Observation on Maximum Inspiratory and Expiratory Respiratory Pressures
The MIP increased significantly after 3 months compared to that at 0-month baseline in subjects in the rehabilitation group. These data are summarized in Fig. 5.
Rehabilitation increases MIP. We measured MIP at baseline (solid gray bars) and again after 3 months (cross hatched bars) of rehabilitation (Rehabilitation) or observation (Control). Data shown are the mean ± SEM MIP (mmHg) measurements in the rehabilitation and control groups at baseline and at 3 months. MIP did not change after 3 months in the control group, while it increased significantly in the rehabilitation group; *P < 0.05. The maximum expiratory pressure (MEP) did not change significantly in either group
Effects of Rehabilitation on 6-Minute Walk Tests
The 6-MWT distance did not change significantly as a result of the 3-month rehabilitation program, nor did it change significantly in controls after the observation period. These data are summarized in Table 6.
Effects of Rehabilitation on BDI and Ventilatory Efficiency
Completion of the rehabilitation program did not decrease the level of dyspnea experienced after the 6-MWT, nor did it change after the observation period. These data are summarized in Table 7. Consistent with its lack of effect on dyspnea, rehabilitation had no effect on the subjects’ ventilatory efficiency, represented by VE/VCO2 slope [3, 4]. These data are given in Table 8.
Discussion
Mechanisms of Exercise Limitation on Cycle Ergometry
Moderate-intensity constant-load exercise testing has been used successfully to test the effects of selected interventions such as exercise training and pharmacologic therapies [18–20]. IPF subjects did not usually reach predicted maximum or heart rates or minute ventilation, because symptoms restricted their ability to exercise at predicted maximum levels [3, 4]. On average, subjects reached 63 ± 3 (SEM) % of the predicted MVV (group mean baseline MVV was 71.7 ± 4.6 L/min), indicating that subjects exercised submaximally because of other factors such as dyspnea, hypoxemia, and oxidant stress. Total ventilation remained quite inefficient compared to carbon dioxide production (V E/VCO2 slope) throughout the test [3, 4]. The V E/VCO2 slope was markedly elevated during exercise, demonstrating an inability to optimize respiratory function even at these mild workloads [4].
Despite the low level of work (50 W) and the often brief exercise testing time (<10 min), subjects had uniformly increased plasma lactate levels after exercise testing, indicating a physiologically important shift to anaerobic energy production [4]. Concomitant with severe hypoxemia and increased plasma lactate, we found that IPF subjects also had an increase in plasma 15-F2-isoprostanes after exercise, a highly reliable (when measured by mass spectroscopy) marker of systemic oxidant stress and lipid peroxidation [26, 27]. This is likely because both exercise and cellular hypoxia increase the production of ROS [7, 31]. The increased plasma isoprostane concentrations we found here reflect increased oxidation of arachidonic acid [8].
Activation of phospholipase A2 leads to further increased intracellular ROS and release of oxidized arachidonic acid products, which result in isoprostane production [32]. ROS produced during exercise impair calcium metabolism and myofilament function in skeletal muscle cells, resulting in the lack of endurance that we observed [7, 31].
NT-proBNP, a putative marker of pulmonary hypertension in interstitial lung diseases [33], increased significantly after cycle ergometry testing, suggesting increased pulmonary artery pressure. Patients with IPF are at risk of developing worsened pulmonary hypertension with exercise because of fixed vascular resistance [34]. Brain natriuretic peptide levels correlate well with pulmonary hypertension determined by right heart catheterization in interstitial lung diseases [33]. In addition, 15-F2t-isoprostanes are potent vasoconstrictors in pulmonary circulation [32]. The plasma concentration of thromboxane B2, which might also increase pulmonary resistance, increased during exercise in a previously studied group of IPF patients [34].
Blood glutamine increases with power output during exercise in normal men and the increase parallels the blood ammonia concentration [35]. Muscle glutamate concentration decreases after short-term exercise in COPD patients, and this has been attributed to oxygen deprivation [36]. We detected a large (twofold) increase in plasma GLU after exercise in patients with IPF, suggesting its release from muscle stores. Glutamate may enhance energy production in hypoxic tissue by conversion to succinate [37]. Increased ARG might modulate increases in pulmonary artery pressure otherwise occurring with exercise [38].
We found (in those subjects not taking N-acetyl-l-cysteine, a common empiric therapy for IPF) that the ratio of cysteine to cystine decreased significantly in plasma after exercise. This change in [cysteine]/[cystine] signals a shift in the reduction–oxidation state to a more oxidized milieu after exercise.
Effects of Pulmonary Rehabilitation on Exercise Capacity of IPF Patients
A clear and important training effect was evident in increased endurance time at 50-W exercise, maintenance of exercise VO2 during constant-load testing, increase in treadmill MET-minutes, and improvement in respiratory muscle strength (MIP) after rehabilitation [22].
Pulmonary rehabilitation as applied in our program (see Table 2) did not significantly change the 6-MWT distance in these strictly defined IPF patients. Rehabilitation and control groups both experienced significant increases in dyspnea after the 6-MWT, and 3 months of rehabilitation did not ameliorate the increase in the BDI. IPF patients likewise did not improve ventilatory work efficiency (V E/VCO2 slope) as a result of rehabilitation. Similarly, Nishiyama et al. [11] reported that a 10-week exercise program did not improve pulmonary function or dyspnea in IPF patients, but, in contrast, it did increase the 6-MWT distance by 46 m (95 % confidence interval = 8–84 m), which du Bois et al. [39] interpreted as clinically important. Salhi et al. [12] reported that patients with various restrictive lung diseases demonstrated improved 6-MWT distance and quadriceps strength after a 12-week rehabilitation program, although their study had no control group and the enrolled population differed greatly from ours. On the whole, the benefit of pulmonary rehabilitation on exercise capacity is not as clear in IPF as it is in COPD, although it may enhance quality of life [40, 41]. Mean 6-MWT distance decreased 6 m in the rehabilitation group, while it decreased by 15 m in controls. Neither mean change is considered clinically important (i.e., 24–45 m) for patients with IPF [39].
In patients with end-stage lung diseases awaiting transplantation, the 6-MWT distance correlated with maximum oxygen uptake [42]. We found no such correlation between exercise VO2 and 6-MWT distance in this trial. Exercise VO2 more precisely represents moderate to maximum exercise capacity, while 6-MWT distance reflects the ability to do sustained, low-level exercise [43].
Limitations of the Study
Because the effects of pulmonary rehabilitation on 6-MWT distance and perception of dyspnea are small, a larger number of subjects would be required to definitively demonstrate an effect on those variables. Subjects all had clinically diagnosed IPF according to ATS-ERS criteria [14]. Only 2 of 21 subjects had undergone surgical lung biopsy to definitively diagnose UIP, so it remains formally possible that some subjects may have been misclassified [1]. We did not do right heart catheterizations to measure pulmonary artery pressures, and it remains possible (since we used echocardiography) that some subjects with severe pulmonary hypertension, which would by itself limit exercise, may have been included [15].
Conclusions
We did not design this study to develop clinical guidelines, although its results suggest that clinical benefits and improvements in quality of life may accrue to patients with IPF as a result of pulmonary rehabilitation. We also found (Gaunaurd et al., unpublished observations) that subjects who completed the pulmonary rehabilitation program experienced improvements in the symptom domain of the St. George’s Respiratory Questionnaire for IPF [44]. The 12-week rehabilitation program tested here is comparable to that recently recommended [40], and it is practical for enrolled subjects in regard to time and effort commitment. Rehabilitation programs are not, however, standardized and vary widely based on local practice and reimbursement schemes [9]. We did not specifically test the premise that extended periods of rehabilitation might provide additional benefits by delaying declines in functional status of patients with IPF, which is often relentlessly progressive. Our program clearly increased endurance time (cycle ergometry) and maintained exercise capacity (oxygen uptake) and skeletal muscle strength (MIP) during rehabilitation. Pulmonary rehabilitation is clearly not harmful, and thus it may be a useful therapeutic modality in patients with IPF.
We conclude that although patients with IPF are limited by symptoms and have a relentlessly progressive disease, a pulmonary rehabilitation program like that we describe produces measurable benefits in maintaining exercise capacity and increasing endurance time and respiratory muscle strength. Mechanisms of exercise limitation, including oxidant stress related to hypoxemia, warrant further study so that more targeted exercise regimens can be designed.
References
King T, Pardo A, Selman M (2011) Idiopathic pulmonary fibrosis. Lancet 378:1949–1961
Christie J, Edwards L, Kucheryavaya A, Aurora P, Dobbels F, Kirk R, Rahmel A, Stehlik J, Hertz M (2010) The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult lung and heart–lung transplantation report-2010. J Heart Lung Transplant 29:1103–1118
O’Donnell D, Laveneziana D (2007) Patterns of cardiopulmonary response to exercise in lung disease. Eur Respir Monogr 12:69–92
Jones N, Killian K (2000) Exercise limitation in health and disease. N Engl J Med 343:632–641
Shorr A, Wainright J, Cors C, Lettieri C, Nathan S (2007) Pulmonary hypertension in patients with pulmonary fibrosis awaiting lung transplant. Eur Respir J 30:715–721
Jackson R, Ramos C, Glassberg M, Bejarano P, Gómez-Marin O (2010) Sildenafil therapy and exercise tolerance in idiopathic pulmonary fibrosis. Lung 188:115–123
Clanton T (2007) Hypoxia-induced reactive oxygen species formation in skeletal muscle. J Appl Physiol 102:2379–2388
Jackson R, Ramos C, Gupta C, Gómez-Marin O (2010) Exercise decreases plasma antioxidant capacity and increases urinary isoprostanes in IPF. Respir Med 104:1919–1928
Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, Carone M, Celli B, Engelen M, Fahy B, Garvey C, Goldstein R, Gosselink R, Lareau S, MacIntyre N, Maltais F, Morgan M, O’Donnell D, Prefault C, Reardon J, Rochester C, Schols A, Singh S, Troosters T, ATS, ERS Pulmonary Rehabilitation Writing Committee (2006) American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 173:1390–1413
Holland A, Hill C (2008) Physical training for interstitial lung disease. Cochrane Database Syst Rev (4):CD006322. doi:10.1002/14651858.CD006322.pub2
Nishiyama O, Kondoh Y, Kimura T, Kato K, Kataoke K, Ogawa T, Watanabe F, Arizono S, Nishimura K, Taniguchi H (2008) Effects of pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis. Respirology 13:354–399
Salhi B, Troosters T, Behaegel M, Joos G, Derom E (2010) Effects of pulmonary rehabilitation in patients with restrictive lung diseases. Chest 137:273–279
Huppman P, Sczepansk B, Boensch M, Winterkamp Schonheit-Kenn U, Neurohr C, Behr J, Kenn K (2013) Effects of inpatient pulmonary rehabilitation in patients with interstitial lung disease. Eur Respir J 42:444–453
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE Jr, Kondoh Y, Myers J, Müller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schünemann HJ, ATS, ERS, JRS, ALAT Committee on Idiopathic Pulmonary Fibrosis (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183:788–824
Arcasoy S, Christie J, Ferrari V, St. John Sutton M, Zisman D, Blumenthal N, Pochettino A, Kotloff R (2003) Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Respir Crit Care Med 167:735–740
Lynch D, Godwin D, Safrin S, Starko K, Hormel P, Brown K, Raghu G, King T, Bradford W, Schwartz D, Webb W (2005) High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med 172:488–493
Rosdahl H, Gullstrand L, Salier-Eriksson J, Johansson P, Schantz P (2010) Evaluation of the Oxycon mobile metabolic system against the Douglas bag method. Eur J Appl Physiol 109:159–171
Puente-Maestu L, Sanz M, Sanz P, Ruiz de Ona J, Rodriguez-Hermosa J, Whipp B (2000) Effects of two types of training on pulmonary and cardiac responses to moderate exercise in patients with COPD. Eur Respir J 15:1026–1032
Puente-Maestu L, Sanz M, Sanz P, Cubillo J, Mayol J, Casaburi R (2000) Comparison of effects of supervised versus self-monitored training programmes in patients with chronic obstructive pulmonary disease. Eur Respir J 15:517–525
Palange P, Galassetti P, Mannix E, Farber M, Manfredi F, Serra P, Carlone S (1995) Oxygen effect on O2 deficit and VO2 kinetics during exercise in obstructive pulmonary disease. J Appl Physiol 78:2228–2234
Solberg G, Robstad B, Skjonsberg O, Borchsenius F (2005) Respiratory gas exchange indices for estimating the anaerobic threshold. J Sports Sci Med 4:29–36
American Thoracic Society/European Respiratory Society (2002) ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med 166:518–624
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117
American Thoracic Society (1999) Dyspnea. Mechanisms, assessments and management: a consensus statement. Am J Resp Crit Care Med 159:321–340
Byrne N, Hills A, Hunter G, Weinsier R, Schutz Y (2005) Metabolic equivalent: one size does not fit all. J Appl Physiol 99:1112–1119
Haschke M, Zhang Y, Kahle C, Klawitter J, Korecka M, Shaw L, Christians U (2007) HPLC-atmospheric pressure chemical ionization MS/MS for quantification of 15-F2-isoprostane in human urine and plasma. Clin Chem 53:1–9
Klawitter J, Haschke M, Shokati T, Klawitter J, Christians U (2011) Quantification of 15-F2-isoprostane in human plasma and urine: Results from enzyme-linked immunoassay and liquid chromatography cannot be compared. Rapid Commun Mass Spectrom 25:463–468
Lundholm L, Mohme-Lundholm E, Vamos N (1963) Lactic acid assay with L(+) lactic acid dehydrogenase from rabbit muscle. Acta Physiol Scand 58:243–249
Elin R, Winter W (2004) Laboratory and clinical aspects of b-type natriuretic peptides. Arch Pathol Lab Med 128:669–697
Cnaan A, Laird N, Slasor P (1997) Using the general linear mixed model to analyze unbalanced repeated measures and longitudinal data. Stat Med 16:2349–2380
Powers S, Nelson W, Hudson M (2011) Exercise-induced oxidative stress in humans: causes and consequences. Free Radical Biol Med 51:942–950
Basu S (2008) F2-isoprostanes in human health and diseases: from molecular mechanisms to clinical implications. Antioxid Redox Signal 10:1405–1434
Leuchte H, Neurohr C, Baumgartner R, Holzapfel M, Giehrl W, Vogeser M, Behr J (2004) Brain natriuretic peptide and exercise capacity in lung fibrosis and pulmonary hypertension. Am J Respir Crit Care Med 170:360–365
Blanco I, Ribas J, Xaubet A, Gómez F, Roca J, Rodriguez-Roisin R, Barberà J (2011) Effects of inhaled nitric oxide at rest and during exercise in idiopathic pulmonary fibrosis. J Appl Physiol 110:138–145
Henriksson J (1991) Effect of exercise on amino acid concentrations in skeletal muscle and plasma. J Exp Biol 160:149–165
Engelen M, Wouters E, Does J, Schols A (2001) Effects of exercise on amino acid metabolism in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 161:859–864
Pisarenko O, Solomatina E, Ivanov V, Studneva I, Kapelko V, Smirnov V (1985) On the mechanism of enhanced ATP formation in hypoxic myocardium caused by glutamic acid. Basic Res Cardiol 80:126–134
Mitani Y, Maruyama K, Sakurai M (1997) Prolonged administration of l-arginine ameliorates chronic pulmonary hypertension and pulmonary vascular remodeling in rats. Circulation 96:689–697
du Bois R, Weycker D, Albera C, Bradford W, Costabel U, Karteshev A, Lancaster L, Noble P, Sahn S, Swarcberg J, Thomer M, Veleye D, King T (2011) Six-minute-walk tests in idiopathic pulmonary fibrosis. Test validation and minimal clinically important difference. Am J Respir Crit Care Med 183:1231–1237
Bolton C, Bevan-Smith E, Blakely J, Crowe P, Elkin S, Garrod R, Greening N, Heslop K, Hull J, Man W, Morgan M, Proud D, Roberts M, Sewell L, Singh S, Walker P, Walmsley S (2013) British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 68:ii1–ii30
Ferreira A, Garvey C, Connors G, Hilling L, Rigler J, Ferrell S, Cayou C, Shoriat C, Collard H (2009) Pulmonary rehabilitation in interstitial lung disease. Benefits and predictors of response. Chest 135:442–447
Cahalin L, Pappagianopoulus P, Prevost S, Wain J, Ginns L (1995) The relationship of the 6-minute walk test to maximal oxygen consumption in transplant candidates with end stage lung disease. Chest 108:452–459
Fell C, Liu L, Motika C, Kaserooni E, Gross B, Travis W, Colby T, Murray S, Toews G, Martinez F, Flaherty K (2009) The prognostic value of cardiopulmonary exercise testing in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 179:402–407
Yorke J, Jones P, Swigris J (2010) Development and validity testing of an IPF specific version of the St George’s respiratory questionnaire. Thorax 65:921–926
Acknowledgments
We thank Dr. Rafael Valenzuela and Mr. Roman Miguel for assaying lactate and NT-proBNP. We also thank Drs. Uwe Christians and Jelena Klawitter of Integrated Solutions in Clinical Research and Development, University of Colorado, Aurora, CO, for assaying 15-F2t-isoprostanes. This study was supported by a Merit Review Award from the VA Research Service.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jackson, R.M., Gómez-Marín, O.W., Ramos, C.F. et al. Exercise Limitation in IPF Patients: A Randomized Trial of Pulmonary Rehabilitation. Lung 192, 367–376 (2014). https://doi.org/10.1007/s00408-014-9566-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-014-9566-9