Abstract
Background
Blood lactate levels and central venous oxygen saturation (ScvO2) are known to be useful indicators of global tissue hypoxia. However, it is unclear whether ScvO2 correlates with lactate levels when measured simultaneously and whether changes in ScvO2 or lactate levels in serial measurements have prognostic value. We investigated the correlation between ScvO2 and lactate levels measured simultaneously and their association with clinical outcomes.
Methods
We performed a prospective observational study of patients with severe systemic inflammatory response syndrome (SIRS) and severe sepsis who were admitted to the medical intensive care unit. ScvO2 and lactate levels were measured simultaneously at the time of study enrollment, every 6 h for 24 h, and then every 24 h until the goal was reached.
Results
Twenty-five patients were enrolled in the study; 13 have died and 12 have survived. There was no correlation between lactate levels and ScvO2. Neither lactate levels nor ScvO2 at the time of admission differed between nonsurvivors and survivors. Normalization of lactate levels within 48 h was significantly associated with survival.
Conclusions
In patients with severe SIRS and severe sepsis, simultaneously measured ScvO2 and lactate levels showed no correlation, and normalization of lactate levels within 48 h was a predictive factor for survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The systemic inflammatory response can progress to severe sepsis, septic shock, and multiorgan failure [1]. This progression of systemic inflammatory injury and sepsis leads to circulatory abnormalities and increases metabolic requirements [2]. Consequently, a systemic imbalance is created between systemic oxygen delivery and demand, resulting in global tissue hypoxia [3]. Global tissue hypoxia contributes to the development of multisystem organ dysfunction syndrome and increased mortality [4]. The most well-known biomarkers of global tissue hypoxia are low central venous oxygen saturation (ScvO2) and hyperlactatemia [5]. ScvO2 has been shown to be a surrogate for the cardiac index as a target for hemodynamic therapy. A decreased ScvO2 results from an imbalance between oxygen delivery and oxygen consumption [6]. When systemic oxygen delivery decreases, the systemic oxygen extraction ratio increases as a compensatory mechanism to match systemic oxygen demand. This results in a decrease in ScvO2, which reflects global tissue hypoxia. In contrast, high ScvO2 values do not always indicate adequate tissue oxygen delivery. When oxygen extraction is pathologically impaired because of microcirculatory dysfunction or the inability of cells to use the oxygen, ScvO2 remains high in the presence of hypoxia at the tissue level [7, 8].
Lactate is also a useful and clinically measurable surrogate marker of tissue hypoxia and disease severity [9]. When the limit of this compensatory increase in oxygen extraction (anaerobic threshold) is reached, anaerobic metabolism ensues, leading to lactate production [7]. Thus, hyperlactatemia in critically ill patients has usually been interpreted as a marker of secondary anaerobic metabolism due to an inadequate oxygen supply that induces cellular distress. However, this is not always the case and should not be rigorously interpreted as an indicator of hypoxia [5]. In skeletal muscle and other tissues, aerobic glycolysis is linked to Na+–K+ ATPase activity and stimulates epinephrine [8, 10]. The presence of hyperlactatemia under well-oxygenated conditions can be explained by these findings [11]. In addition, lactate concentrations reflect the balance between lactate production and clearance. Liver and kidney functions and their blood flow influence lactate clearance because blood lactate is metabolized mainly by the liver and kidneys [12]. Thus, as opposed to ScvO2, which is a rudimentary indicator of only the balance between oxygen supply and demand, blood lactate levels reflect the general homeostasis of the host.
Both ScvO2 and blood lactate levels were used as a goal of early sepsis resuscitation in many studies; however, there remains significant debate regarding the relative value of ScvO2 versus blood lactate levels [13, 14]. To our knowledge, no prospective study has directly compared ScvO2 and blood lactate levels measured simultaneously in the same patients with systemic inflammatory response syndrome (SIRS) or sepsis. In this study, we investigated the correlation between ScvO2 and blood lactate levels measured simultaneously in the same patients and compared their prognostic values.
Materials and Methods
Study Design and Patients
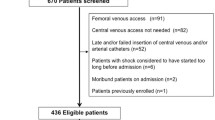
A prospective observational study of patients with severe SIRS and severe sepsis was conducted in Seoul National University Hospital, Seoul, Korea, from June to September 2012. This study was approved by the local institutional review board for human research and performed in accordance with Good Clinical Practice guidelines (IRB No. H-1204-121-408). SIRS was defined according to the presence of two or more of four criteria for SIRS: (1) temperature of >38 or <36 °C; (2) heart rate of >90 beats per minute; (3) respiratory rate of >20 breaths per minute or PaCO2 of <32 mmHg; and (4) white blood cell count of >12,000, <4,000 cu/mm3, or >10 % immature (band) forms [1]. Severe sepsis was defined as sepsis associated with organ dysfunction, hypoperfusion, or hypotension. Hypoperfusion and perfusion abnormalities could include but were not limited to lactic acidosis, oliguria, or an acute alteration in mental status. Hypotension was defined as a systolic blood pressure of <90 mmHg or a reduction of ≥40 mmHg from baseline [1]. Patients with a noninfective insult but pathophysiologic changes equivalent to the definitions of severe sepsis were classified as having severe SIRS [6]. The following were exclusion criteria: age <20 years, pregnancy, an absolute contraindication to chest or neck central venous catheterization, a do-not-resuscitate status, or advance directives restriction implementation of the protocol. All patients were evaluated by an intensive care specialist and were admitted to the intensive care unit (ICU). All patients underwent central venous catheterization and were managed according to the Surviving Sepsis Campaign guideline [15]. Volume resuscitation using crystalloids or colloids was initiated to achieve a central venous pressure of 8–12 mmHg. Vasoactive agents were used to maintain a mean arterial pressure of >65 mmHg. Urine output of >0.5 mL/kg/h also served as a target goal. Patients were intubated and mechanically ventilated as required.
Measurements and Data Collection
Blood lactate levels and ScvO2 were measured simultaneously every 6 h during the first 24 h after enrollment and then every 24 h until the goals were reached or the patient died. The ScvO2 and lactate goals were defined as ≥70 % and a lactate plasma or serum level of ≤4 mmol/L, respectively. All patients underwent placement of a chest or neck central venous catheter capable of measuring ScvO2. ScvO2 was measured by intermittent sampling, and lactate levels were measured in arterial blood using the hospital’s central laboratory.
Data on patient demographics, hemodynamic variables, laboratory values, comorbidities, and admission diagnosis were collected at baseline. Biochemical and clinical variables required for calculation of the Acute Physiology and Chronic Health Evaluation II (APACHE II) and sequential organ failure assessment (SOFA) scores were collected at 0, 6, 12, 18, 24, 48, and 72 h after the start of the study. Therapeutic interventions such as antibiotics, fluids, packed red cell transfusions, vasoactive agents, and mechanical ventilation given in the ICU and for up to 72 h were recorded.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) version 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. For the purpose of this study, blood lactate levels, ScvO2, and organ dysfunction scores (SOFA) were analyzed for all patients enrolled in the study. Descriptive statistics were used to summarize patient characteristics. To investigate the correlation between simultaneously measured blood lactate levels, ScvO2, and SOFA scores, we estimated the correlation coefficient between two variables with repeated observations using a mixed-effects model [16]. A correlation analysis was employed between blood lactate levels and ScvO2, which were measured simultaneously in each patient. Mixed models were used to estimate the differences in lactate levels and ScvO2 between survivors and nonsurvivors. We evaluated the concordance rate of reaching the ScvO2 and lactate goals using Cohen’s kappa. Logistic regression using generalized estimation equations was performed to evaluate the association of clinical outcomes according to the achievement of goals. Data are presented as percentage or mean ± standard deviation.
Results
Baseline Characteristics of Patients
Twenty-five patients were included in the study. Their mean age was 68.12 ± 13.6 years, and 18 patients (72 %) were male. About 50 % of the patients had comorbidities, specifically hypertension or malignancy. Patients had a mean baseline APACHE II score of 33.72 ± 8.0 and SOFA score of 12.32 ± 4.6 at the time of admission to the ICU. Ninety-six percent of the patients required mechanical ventilation, and continuous renal replacement therapy was applied in 68 % of the patients (Table 1).
Among the 25 patients, 4 had nonspecific insult, 10 had a documented infection, and 11 were presumed to have an infectious process. As sepsis is defined as SIRS with a presumed or a confirmed infectious process, 21 patients had severe sepsis. Among the ten patients with documented infection, blood cultures revealed bacteria in five patients and fungi in two patients. Bacteria were isolated from sputum, ascites, and wounds in three patients.
Correlation Between ScvO2 and Blood Lactate Level and Their Relationship with SOFA Score
A statistically significant correlation was not observed between ScvO2 and blood lactate levels (correlation coefficient = 0.0504). ScvO2 showed no correlation with SOFA scores (correlation coefficient = 0.0218). In contrast, blood lactate levels revealed a positive correlation with SOFA scores (correlation coefficient = 0.571).
Concordance Rate of Reaching ScvO2 and Lactate Goals Within 24 h
Ten patients met the ScvO2 goal and 15 met the lactate goal. Of the ten patients who met the ScvO2 goal, seven met the lactate goal and three did not. Of the 14 patients who did not meet the ScvO2 goal, 8 met the lactate goal and 6 did not. There was no statistically significant agreement between the ScvO2 and lactate goal achievements (κ = 0.12, 95 % CI 0.668–0.686).
Association of Reaching ScvO2 and Blood Lactate Goals with Clinical Outcomes
Among the 25 patients, 13 had died and 12 had survived at the end of the measurements. We evaluated whether there was a difference in the clinical characteristics between survivors and nonsurvivors. There was no significant difference between the groups in any of the baseline characteristics, with the exception of the disease severity score (Table 1). Next, the ScvO2 and blood lactate levels at the time of ICU admission were compared between survivors and nonsurvivors. There was a borderline significant difference between survivors and nonsurvivors in blood lactate levels (3.01 vs. 5.45 mmol/L, respectively; p = 0.062) and ScvO2 (65.9 vs. 66.3 %, respectively; p = 0.951) at the time of enrollment. Interestingly, the serial blood lactate measurements, but not ScvO2 (p = 0.4566), showed a significant difference between survivors and nonsurvivors (p = 0.0043). The blood lactate levels of nonsurvivors at 6, 12, 24, and 48 h after admission to the ICU were higher than those of survivors at 6, 12, 24, and 48 h (p < 0.05) (Table 2). We next evaluated the association between clinical outcomes and the achievement of goals by logistic regression analysis. Normalization of blood lactate levels (≤4 mmol/L) within 24 or 48 h was significantly associated with survival (Table 3). In contrast, normalization of ScvO2 (>70 %) was not significantly correlated with survival. The multivariate model included relevant variables with p < 0.2 in univariate analysis. Multivariate logistic regression analysis showed that lactate normalization within 48 h was statistically significantly associated with survival [odds ratio (OR) = 22; p = 0.0107].
Discussion
Severe SIRS or sepsis evolves as a series of hemodynamic phases in which ScvO2 and lactate can serve as surrogates for monitoring the balance between systemic oxygen delivery and demands and for quantifying the severity of global tissue hypoxia [5, 17]. In a state of global tissue hypoxia, a decreased ScvO2 is likely to precede the appearance of lactate. However, which parameter reflects the tissue hypoxia more accurately is unclear. Both ScvO2 and blood lactate levels were used as a goal of early sepsis resuscitation in many studies. Although the optimal goal of resuscitation from sepsis remains unclear, protocols using ScvO2 as an early quantitative resuscitation goal have been demonstrated to improve outcomes in patients with severe sepsis and septic shock [18]. In addition, lactate clearance has been shown to be noninferior to ScvO2 as the final goal during resuscitation from sepsis [19]. Considering the underlying physiology and results of studies on resuscitation goals, ScvO2 and blood lactate levels are likely to correlate with each other. However, the specific correlation between them is unclear. In many previous studies, the ScvO2 and blood lactate levels were not measured simultaneously in the same patient, which is necessary to assess their correlation. In this study, we measured the ScvO2 and blood lactate levels simultaneously in each patient to evaluate the correlation between them. Unexpectedly, there was no correlation between the ScvO2 and blood lactate levels in the same patient. This suggests that each of these physiological processes is complex and influenced by multiple factors. ScvO2 has a half-life of only seconds and provides immediate feedback regarding the relationship between oxygen delivery and consumption, which depends on the phase of sepsis [20]. A low ScvO2 does not always reflect tissue hypoxia. In addition, a normal ScvO2 cannot exclude the possibility of tissue hypoxia. In sepsis, the ScvO2 may be elevated despite tissue hypoxia, perhaps secondary to poor distribution of flow. This leads to concerns that the ScvO2 may not always be a reliable target for quantitative resuscitation because it can sometimes be normal to elevated despite evidence of significant tissue hypoxia [7, 21]. Compared with ScvO2, lactate is a delayed indicator of tissue perfusion and has complex kinetics [22]. Elevated blood lactate has long been regarded as a marker of anaerobic metabolism. However, aerobic mechanisms, such as cytokine-mediated glucose uptake and catecholamine-stimulated Na–K pump hyperactivity, can lead to lactate production in patients with sepsis. Although the blood lactate level usually increases when tissue hypoxia is present, a normal blood lactate level does not exclude the presence of tissue hypoxia. An elevated blood lactate level was not observed in 20–50 % of patients with septic shock at presentation or during the clinical course. All of these findings suggest that neither ScvO2 nor hyperlactatemia always reflects tissue hypoxia because both are affected by many confounding factors. Different confounding factors could give rise to a lack of correlation between ScvO2 and blood lactate levels. This is supported by the absence of significant concordance in achieving ScvO2 and lactic acid goals in this study. It is also in accordance with previous reports [23].
In this study, only lactate levels showed statistically significant differences between survivors and nonsurvivors. In a previous prospective observational study, oxygen-derived variables showed no significant differences, while blood lactate levels had a strong relationship with survival [24]. Many studies have shown that lactate clearance, as a target of resuscitation, predicts better survival [25, 26]. There were no significant differences in ScvO2 between survivors and nonsurvivors at any measurement point in this study; in contrast, many studies have suggested that low ScvO2 is a good predictor of a poor prognosis [18, 27].
What is the reason for this difference in findings? The major difference between this study and previous studies is the method of ScvO2 measurement. While we measured ScvO2 intermittently by sampling at designated times, ScvO2 was measured by continuous monitoring in previous studies. Continuous ScvO2 monitoring, which provides a real-time assessment, has been suggested to be superior to intermittent monitoring [21]. However, it requires special equipment, such as a continuous central venous oxygen spectrophotometer and an appropriate central venous catheter. This is a major barrier that limits its generalizability. Thus, the intermittent monitoring of ScvO2 used in this study might reflect the real practice in the majority of ICUs. The lack of real-time assessment of ScvO2 might be the reason for the failure of ScvO2 to show prognostic significance in this study. In a recent prospective observational pilot study, intermittent ScvO2 monitoring was not inferior to continuous ScvO2 monitoring when done within the first 6 h of intervention [28]. However, another study comparing ScvO2 measurements showed that the achievement of goals and survival were improved to a greater degree with continuous observation of ScvO2 [29]. To validate intermittent monitoring of ScvO2, a large randomized multicenter study is needed.
All of our measurements and comparisons of ScvO2 and lactate levels were obtained after ICU admission, while patients in previous studies were enrolled and monitored in the emergency department. Guidelines for management of severe sepsis and septic shock recommend that the initial resuscitation goal be achieved during the first 6 h of resuscitation [30]. This is based on early goal-directed therapy and emphasizes initial resuscitation. The present study’s enrollment time may be a limitation to the interpretation of our results in that it may not reflect the critical time of early sepsis resuscitation in some patients. In addition, our study is limited in its clinical application in that it was designed as an observational study without intervention and involved a small sample size. The failure to demonstrate prognostic significance of initial lactate or ScvO2 in this study could be due to either missing earlier data or the small sample size. These limitations should be noted when interpreting the study results and warrants further studies in this area.
Conclusion
In patients with severe sepsis and severe SIRS, simultaneously measured blood lactate and ScvO2 show no correlation, and blood lactate levels, but not ScvO2, are associated with patient prognosis.
References
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101(6):1644–1655
Astiz ME, Rackow EC, Falk J, Kaufman BS, Weil M (1987) Oxygen delivery and consumption in patients with hyperdynamic septic shock. Crit Care Med 15(1):26–28
Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson KJ, Trzeciak S, Sherwin R, Holthaus CV, Osborn T (2006) Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest 130(5):1579–1595
Parrillo JE, Parker MM, Natanson C, Suffredini AF, Danner RL, Cunnion RE, Ognibene FP (1990) Septic shock in humans. Advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med 113(3):227–242
Astiz ME, Rackow EC, Kaufman B, Falk J, Weil M (1988) Relationship of oxygen delivery and mixed venous oxygenation to lactic acidosis in patients with sepsis and acute myocardial infarction. Crit Care Med 16(7):655–658
Muckart DJ, Bhagwanjee S (1997) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med 25(11):1789–1795
Bellomo R, Reade MC, Warrillow SJ (2008) The pursuit of a high central venous oxygen saturation in sepsis: growing concerns. Crit Care 12(2):130
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert P-E (2005) Relation between muscle Na+–K+ ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 365(9462):871–875. doi:10.1016/s0140-6736(05)71045-x
De Backer D (2003) Lactic acidosis. Intensive Care Med 29(5):699–702. doi:10.1007/s00134-003-1746-7
McCarter FD, Nierman SR, James JH, Wang L, King JK, Friend LA, Fischer JE (2002) Role of skeletal muscle Na+–K+ ATPase activity in increased lactate production in sub-acute sepsis. Life Sci 70(16):1875–1888
James JH, Luchette FA, McCarter FD, Fischer JE (1999) Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet 354(9177):505–508. doi:10.1016/s0140-6736(98)91132-1
Levy B (2006) Lactate and shock state: the metabolic view. Curr Opin Crit Care 12(4):315–321
Jones AE, Puskarich MA (2009) Sepsis-induced tissue hypoperfusion. Crit Care Clin 25(4):769–779
Sevransky JE, Nour S, Susla GM, Needham DM, Hollenberg S, Pronovost P (2007) Hemodynamic goals in randomized clinical trials in patients with sepsis: a systematic review of the literature. Crit Care 11(3):R67
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL, International Surviving Sepsis Campaign Guidelines Committee; American Association of Critical-Care Nurses; American College of Chest Physicians; American College of Emergency Physicians; Canadian Critical Care Society; European Society of Clinical Microbiology and Infectious Diseases; European Society of Intensive Care Medicine; European Respiratory Society; International Sepsis Forum; Japanese Association for Acute Medicine; Japanese Society of Intensive Care Medicine; Society of Critical Care Medicine; Society of Hospital Medicine; Surgical Infection Society; World Federation of Societies of Intensive and Critical Care Medicine (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36(1):296–327. doi:10.1097/01.CCM.0000298158.12101.41
Roy A (2006) Estimating correlation coefficient between two variables with repeated observations using mixed effects model. Biom J 48(2):286–301
Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson KJ, Trzeciak S, Sherwin R, Holthaus CV, Osborn T, Rivers EP (2006) Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest 130(5):1579–1595. doi:10.1378/chest.130.5.1579
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19):1368–1377. doi:10.1056/NEJMoa010307
Sauneuf B, Charbonneau P (2010) Lactate clearance and central venous oxygen saturation in early sepsis. JAMA 303(20):2031. doi:10.1001/jama.2010.658
Rivers EP, Elkin R, Cannon CM (2011) Rebuttal from Dr. Rivers et al. Chest 140(6):1415–1419
Perel A (2008) Bench-to-bedside review: the initial hemodynamic resuscitation of the septic patient according to Surviving Sepsis Campaign guidelines—does one size fit all? Crit Care 12(5):223
Rivers EP, Elkin R, Cannon CM (2011) Counterpoint: should lactate clearance be substituted for central venous oxygen saturation as goals of early severe sepsis and septic shock therapy? No. Chest 140(6):1408–1413. doi:10.1378/chest.11-2563
Puskarich MA, Trzeciak S, Shapiro NI, Arnold RC, Heffner AC, Kline JA, Jones AE, Emergency Medicine Shock Research Network (EMSHOCKNET) (2012) Prognostic value and agreement of achieving lactate clearance or central venous oxygen saturation goals during early sepsis resuscitation. Acad Emerg Med 19(3):252–258. doi:10.1111/j.1553-2712.2012.01292.x
Bakker J, Coffernils M, Leon M, Gris P, Vincent JL (1991) Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99(4):956–962
Jones AE (2011) Point: should lactate clearance be substituted for central venous oxygen saturation as goals of early severe sepsis and septic shock therapy? Yes. Chest 140(6):1406–1408. doi:10.1378/chest.11-2560
Jansen TC, van Bommel J, Schoonderbeek FJ, Visser SJS, van der Klooster JM, Lima AP, Willemsen SP, Bakker J (2010) Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med 182(6):752–761
Di Filippo A, Gonnelli C, Perretta L, Zagli G, Spina R, Chiostri M, Gensini GF, Peris A (2009) Low central venous saturation predicts poor outcome in patients with brain injury after major trauma: a prospective observational study. Scand J Trauma Resusc Emerg Med 17:23
Huh JW, Oh BJ, Lim CM, Hong SB, Koh Y (2012) Comparison of clinical outcomes between intermittent and continuous monitoring of central venous oxygen saturation (ScvO2) in patients with severe sepsis and septic shock: a pilot study. Emerg Med J 30(11):906–909
Ising P, Smith TW, Simpson SQ (2009) Effect of intermittent vs continuous ScvO2 monitoring on sepsis bundle compliance and mortality. Chest 136(4):21
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R, Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39(2):165–228
Acknowledgments
The authors are grateful for the enthusiastic support of the ICU nurses, assistant nurses, residents, and physicians at Seoul National University Hospital. They thank the Medical Research Collaborating Center in Seoul National University Biomedical Research Institute for help with the statistical analysis of the clinical data.
Conflict of interest
None of the authors has any conflicts of interest with regard to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, JH., Lee, J., Park, Y.S. et al. Prognostic Value of Central Venous Oxygen Saturation and Blood Lactate Levels Measured Simultaneously in the Same Patients with Severe Systemic Inflammatory Response Syndrome and Severe Sepsis. Lung 192, 435–440 (2014). https://doi.org/10.1007/s00408-014-9564-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-014-9564-y