Abstract
Purpose
Fractional exhaled nitric oxide (FeNO) has emerged as an important biomarker in asthma. Increasing evidence points to atopy as a confounding factor in the interpretation of elevated FeNO. We conducted a longitudinal study to understand the clinical significance of FeNO as an inflammatory biomarker.
Methods
We identified 19 children aged 13–15 years at baseline with a significant elevation in FeNO ≥ 80 parts per billion (ppb) and randomly selected a group of children of similar age with a moderate elevation (40–79 ppb) and normal-to-low FeNO (<40 ppb). Between November 2010 and July 2011, three additional study visits were conducted.
Results
Ninety-three children participated in the study. There were 16, 24, and 53 participants in the high, mid, and low FeNO groups. During 1.5 years of follow-up, mean FeNO levels were 82.6 ppb (standard deviation [SD] = 65.9) for atopic asthmatics, 50.6 ppb (SD = 42.6) for nonasthmatic atopics, 17.0 ppb (SD = 10.8) for nonatopic asthmatics, and 17.8 ppb (SD = 13.9) for nonatopic nonasthmatics (p < 0.001). FeNO levels remained stable: 63 % of the high FeNO group had a FeNO ≥ 80 across all 4 measurements and 87 % of the normal-to-low FeNO group had a FeNO of <40 across all 4 measurements. The high FeNO group also was found to have an elevation in IL-5 (p = 0.04), IL-6 (p = 0.003), IL-10 (p = 0.002), and total serum IgE (p < 0.001), after adjustment by age, sex, height, body mass index, and atopy and asthma status.
Conclusions
An elevation of FeNO appears to indicate an atopic phenotype regardless of an asthma diagnosis, clinical symptoms, or corticosteroid use. An elevation of FeNO also is associated with a systemic elevation in inflammatory cytokines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a chronic inflammatory disorder of the airways with a current worldwide prevalence estimated at 300 million [1]. Given the worldwide burden of asthma, significant efforts have been made to identify noninvasive markers for lower airway inflammation, both to aid in asthma diagnosis and management. In the 1990s, individuals with asthma were found to have an elevated fractional exhaled nitric oxide (FeNO) [2–5]. FeNO originates from the bronchial epithelium and has been shown to reflect eosinophilic airway inflammation. Increased levels of FeNO have been found to correlate with sputum and bronchoalveolar lavage eosinophilia [6, 7].
FeNO has emerged as a promising inflammatory marker of asthma. Initial data found that an elevation in FeNO was correlated with an increase in asthma symptoms, and it was as predictive of asthma exacerbations as a decrease in spirometric values. Other studies have shown that FeNO predicts a patient response to corticosteroids [5, 8, 9]. However, despite these promising findings, there has been no proven advantage to FeNO-based treatment protocols [10]. A recent study questions the clinical utility of FeNO by finding no correlation between FeNO levels and symptoms of asthma and allergic rhinitis. Moreover, the study found no difference in FeNO levels among allergic rhinitis patients with or without asthma [11].
Increasing evidence points to the fact that the presence of atopy confounds the interpretation of elevated FeNO in asthma patients. Studies have shown that FeNO levels are raised in atopic subjects, regardless of whether or not they have significant lower respiratory tract symptoms [5, 12, 13]. Studies of multiple birth cohorts of asthmatic and atopic patients found that only atopic asthmatics had an elevation in FeNO and that nonatopic asthmatics had relatively normal levels [5, 13].
The definition of elevated FeNO levels have varied throughout the literature with the upper limit of normal in the general population having been defined from 20 to 50 ppb. However, a recent ATS consensus statement has now defined a low FeNO level as <25 ppb, a mid FeNO level as 25–50 ppb, and a high FeNO level as >50 ppb [14]. Our research group previously conducted a population-based, cross-sectional study that examined the effect of urbanization on asthma and atopy in children aged 13–15 years at enrollment while living in a peri-urban environment in Lima, Peru [15]. Of the approximately 600 participants evaluated in this previous study, 19 children were found to have a significant elevation in their FeNO level ≥80 ppb, whereas the mean FeNO level for the whole study population was 21.7 ppb.
Elevation of FeNO to levels ≥80 ppb has not been meaningfully discussed in the current literature. Thus, we performed a longitudinal assessment of FeNO levels in these participants with extreme elevations in FeNO to determine if these levels persisted over time. We also revisited children who were found to have mid and low levels of FeNO to gain a better understanding of the clinical significance of FeNO as an inflammatory biomarker and its relationship to both asthma and atopy. An additional goal of our study was to explore the relationship between FeNO levels and inflammatory cytokines associated with asthma since several cytokines, such as IL-4, IL-5, IL-6, IL-10, IL-13, IFN-γ, and TNF-α, have been found to play a key role in the Th1 and Th2 mediated airway inflammation of asthma [16–20].
Methods
Study Setting
Our study was conducted at Pampas de San Juan de Miraflores, a peri-urban shanty town outside of downtown Lima, Peru with approximately 60,000 inhabitants. Our target population was children who had participated in a previous study of asthma prevalence in Lima, Peru [15, 21]. Of 593 participants from this previous study, 19 children (3 %) had a FeNO level of ≥80 ppb (high FeNO group). The remaining participants (n = 574) were grouped into a mid FeNO group (40–79 ppb) and a normal-to-low FeNO group (<40 ppb). Our goal was to enroll all 19 participants with high FeNO levels, 40 participants for both the mid FeNO group and 40 in the normal-to-low FeNO group. To meet this goal, we used a simple random sample of participants from these mid and normal-to-low FeNO groups and asked them to participate in this follow-up study. This study was approved by the Institutional Review Boards of the Johns Hopkins Bloomberg School of Public Health in Baltimore, MD, and A.B. PRISMA in Lima, Peru.
Study Design
This is an ancillary study to a large population based study that was conducted in 2009 examining the effect of urbanization on asthma in Peru [15, 21]. We conducted a longitudinal follow-up study consisting of three visits, each performed 3 months apart between November 2010 and July 2011. Home visitations were conducted to enroll participants, administer questionnaires, and perform physical testing. Each visit included a questionnaire, spirometry testing, and measurement of exhaled nitric oxide. Questionnaires assessed asthma, allergy symptoms, use of asthma medications, asthma severity, allergic rhinitis, eczema symptoms, family history, and smoking history.
Spirometry was conducted in accordance with guidelines from the European Respiratory Society and the American Thoracic Society [22] using a handheld spirometer (Jaeger/ERT, Hoechberg, Germany). A maximum of eight forced expiratory maneuvers were allowed to achieve three maneuvers that met acceptability and reproducibility criteria [22]. Participants not meeting quality criteria were revisited up to two more times on a different day for repeat spirometry. Participants withheld any bronchodilators within 4–12 h of testing. Participants reporting a respiratory infection in the past 2 weeks were revisited on a later date. FeNO levels were measured in parts per billion (ppb) using a portable chemiluminescent analyzer (NIOXMINO, Aerocrina, Solna, Sweden) following standard guidelines [14]. FeNO was measured before spirometric testing.
We also collected blood samples from study participants once during the study period using a 7-ml tube without gel. All samples were centrifuged within 1 h of collection at 1,000 rpm for 10 min. The serum was then separated into five cryovials. One cryovial was used to measure total serum immunoglobulin E (IgE) and C-reactive protein (CRP). Two cryovials were analyzed for cytokines levels (IL-1β, IL-4, IL-5, IL-6, IL-10, IL-13, IFN-g, TNF-α), and the remaining two cryovials were stored in our repository as backup. All samples were stored at −20 °C until processing. Cytokines were analyzed using the Millipex HSCYTO-60SK-08 Human Cytokine High Sensitivity kits on a Luminex 100 device (Luminex 100, Luminex Corp, Austin, TX). Total serum IgE and CRP were processed using standard techniques.
Definitions
We defined asthma as a history of wheezing or use of asthma medications in the past 12 months, or a physician diagnosis of asthma. Atopy was identified with a positive puncture skin response (i.e., ≥3 mm than the negative control) to any of the following allergens: cockroach, dust mite mixture, cat hair, dog epithelium, mouse epithelium, and mold mixture (ALK-Abello, Round Rock, USA). We calculated % predicted lung function values using formula recommended by Hankinson et al. [23].
Biostatistical Methods
We compared continuous variables using an analysis of variance (ANOVA) test if the variables were normally distributed. If variables were not normally distributed, they were compared using a Kruskal–Wallis one-way analysis of variance. Dichotomous or categorical values were compared with Chi-square tests or Fisher exact tests, as appropriate. Log-transformation analysis was used to evaluate the relationship between total serum IgE, CRP, cytokines, and FeNO. We used multiple linear regressions to identify the relationship of spirometric values and total serum IgE with log-transformed FeNO in our study population. We used tobit regression to analyze the association of FeNO and log-transformed cytokines (IL-1β, IL4, IL-5, IL-6, IL-10, IL-13, IFN-γ, TNF-α) with undetectable lower bounds that were adjusted for age, sex, asthma-atopy condition, and body mass index. Longitudinal assessment of FeNO was assessed after stratifying by disease condition (asthma or atopy condition) and by group of FeNO (normal-to-low, mid and high). We conducted statistical analyses using STATA 11 (STATA Corp., College Station, TX) and R (www.r-project.org).
Results
Participant Characteristics
A total of 202 children were invited to participate in the study, and 108 (53 %) participants were enrolled. Reasons for nonenrollment included time constraints, refusal to comply with all study visits (26.2 %), and migration out of the study area (20.3 %). There were no significant differences related to sex (p = 0.42), age (p = 0.99), asthma status (p = 0.2), or atopy (p = 0.12) between enrolled and nonenrolled participants. Of the nonenrolled participants 2 % (2/94) were in the high FeNO group, 22 % (21/94) were in the mid FeNO group, and 76 % (71/94) were in the normal-to-low FeNO group. Throughout the three study visits, 15 participants were lost to follow-up and 93 had evaluation for all three visits. Lost to follow-up rates were 6 % (1/17) in the high FeNO group, 20 % (6/30) in the mid FeNO group, and 13 % (8/61) in the normal-to-low FeNO group.
Baseline characteristics of the study participants are described in Table 1. At the end of study, there were 16, 24, and 53 participants in the high, mid, and normal-to-low FeNO groups, respectively. Each group was further divided into the following disease categories: atopic asthmatics, nonatopic asthmatics, nonasthmatic atopics, and nonasthmatic nonatopics. We present diagnosis and treatment characteristics of asthmatic children in Table 2. Specifically, 80 % (20/25) of asthmatics were diagnosed by a physician, 96 % (24/25) experienced wheezing in the 12 months before study initiation, and 100 % (25/25) met at least two of the three criteria. Forty-eight percent (12/25) of asthmatics used any asthma medication in the previous 12 months. Asthmatics in the high FeNO group were more likely to be on treatment with 100 % (8/8) either using oral prednisone, inhaled corticosteroids, or short-acting beta agonists at some point during the 12 months before study initiation. This trend of a higher percentage of asthmatics in the high FeNO group being on treatment remained throughout the study period.
Longitudinal Assessment of FeNO
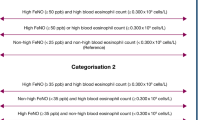
A total of 100, 88, and 43.5 % of the high, mid, and normal-to-low FeNO adolescents, respectively, were found to have atopy. During 1.5 years of follow-up, mean FeNO levels by disease category as displayed in Fig. 1 were: 82.6 ppb (standard deviation [SD] = 65.9) for atopic asthmatics; 50.6 ppb (SD = 42.6) for nonasthmatic atopics; 17.0 ppb (SD = 10.8) for nonatopic asthmatics, and 17.8 ppb (SD = 13.9) nonatopic nonasthmatics (p < 0.05). In general, participants stayed within their FeNO groups throughout follow-up: 63 % of participants in the high FeNO group were found to have a FeNO ≥ 80 across all 4 measurements and 87 % of participants low FeNO group was found to have a FeNO of ≤40 across all 4 measurements (Fig. 2).
Mean fractional exhaled nitric oxide (FeNO) levels stratified by disease category and measurement period (in months). B represents baseline measurement. Each dot represents an individual FeNO measurement at a specific measurement team, and the red horizontal line represents the mean value of FeNO for a specific time period within each disease category
Association of FeNO with Spirometry
We did not find a significant association between FeNO and spirometry values. There were no significant differences in prebronchodilator FEV1, FVC, FEV1/FVC over time among the high, mid, and normal-to-low FeNO groups (Table 1) or in % predicted FEV1 among the high, mid, and normal-to-low FeNO groups at 0 months (p = 0.15), 3 months (p = 0.17), or 6 months (p = 0.2). Also, there were no significant differences in the spirometry values when compared by disease category: atopic asthmatics, nonasthmatic atopics, nonatopic asthmatics, and nonatopic nonasthmatics.
Association of FeNO with Total Serum IgE and CRP
Children in the high FeNO group had higher levels of both total serum IgE and CRP (Fig. 3). The geometric mean of total serum IgE was 1,688 kU/L (geometric SD = 2.1), 1,349 kU/L (geometric SD = 2.0), and 288 kU/L (geometric SD = 4.5) for the high, mid, and normal-to-low FeNO groups respectively (p = 0.001). Mean CRP was 2.3 mg/L (SD = 4.5), 1.8 mg/L (SD = 5.3), 0.7 mg/L (SD = 1.1) for the high, mid, and low FeNO groups respectively (p = 0.21).
Association Between FeNO and Inflammatory Cytokines
Of the cytokines that we measured, IL-1β, IL-4, IL-13, and IFN-γ were undetectable in >20 % of sera tested. Bivariate analysis by FeNO group showed that the high FeNO group had significantly higher levels of IL-5 and IL-10 (Table 3). Multivariable tobit regression analysis showed that the high FeNO group had significantly higher levels of IL-5, IL-6, and IL-10, after adjusting by age, sex, body mass index, height, asthma, and atopic condition. Also we assessed the correlation between exhaled nitric oxide and other inflammatory biomarkers. We observed a significant association using a pairwise Spearman analysis between total serum IgE and IL-5 (r = 0.39, p < 0.001), IL-5 and FeNO (r = 0.35, p < 0.001), and total serum IgE levels and FeNO (r = 0.54, p < 0.001; Fig. 4).
Correlation matrix plot of fractional exhaled nitric oxide (FeNO) values, total serum IgE, C-reactive protein (CRP), IL-5, IL-6, and IL-10. The heat map represents the direction of the correlation (ranging from red for negative values to blue for positive values), and the shape of the ellipse represents the magnitude of the correlation
Discussion
We performed a longitudinal assessment of FeNO in participants with varying baseline measurements to gain a better understanding of its clinical significance as an inflammatory biomarker and its relationship with asthma and atopy. Our data indicate that atopic status, regardless of an asthma diagnosis, was linked with elevated FeNO levels. In contrast, nonatopic asthmatics had FeNO levels that were similar to controls. We also found a synergistic increase of FeNO in patients with both atopy and asthma with atopic asthmatics having the highest FeNO levels.
Individual participants in our study were also found to have relatively stable FeNO levels during the 1.5-year study period, regardless of whether their baseline measurement was high or low. The lack of variation in FeNO levels that we found may help explain the failure of FeNO based asthma treatment protocols. A previous study found a distinctly heterogeneous response of FeNO to high doses of inhaled corticosteroids in asthmatic patients [10]. Specifically, these investigators found that a subgroup of clinically well-controlled asthmatics with high allergic indices had persistently elevated levels of FeNO that did not respond to high doses of ICS [10].
We found that only 2 % of asthmatic participants used ICS prior to study initiation as well as throughout the study period. These patients were in the high and mid FeNO groups with 13 and 9 %, respectively, of asthmatics using ICS. Despite the use of ICS, these participants had relatively high FeNO levels throughout the study. This finding also was true for subjects who had used oral corticosteroids in the last 12 months, with 100 % of patients in the high FeNO group and 36 % of the mid FeNO group. Despite the use of systemic corticosteroids, these participants had relatively high FeNO levels throughout the study, falling into the high (≥80 ppb) and mid (40–79 ppb) groups. We found no correlation between FeNO and spirometry, regardless of FeNO level or disease category.
The relationship between FeNO and atopy has been shown in previous studies [5, 13, 24–27], and it has been confirmed by our data. In our study, we found that high FeNO levels also correlated with a high total serum IgE. This strengthens the relationship between FeNO and atopy. Atopic asthma has been found to be a predominately Th2-mediated response to allergen exposure [18, 19]. Th2 mediated cytokines include IL-4, IL-5, IL-9, IL-10, IL-13, IL-33, and GM-CSF [16, 18, 28]. Release of these cytokines results in eosinophilic activation and inflammation, which ultimately leads to airway damage and bronchial hyperresponsiveness. IL-5 plays a central role in eosinophilic differentiation [16]. In cytokine analysis, we found that patients with high FeNO levels had significantly higher levels of IL-5, IL-6, and IL-10. Given that half of the children in the high FeNO group were atopic asthmatics, results from cytokine analysis in this study supports the theory of a Th2-mediated response in allergic asthma and further strengthens our finding that elevated levels of FeNO reflect an atopic phenotype. IL-6, a proinflammatory cytokine, is known to be important in the pathogenesis of many inflammatory disorders, including allergic asthma. Recent studies suggest that atopy may influence the IL-6 pathways to induce a more severe Th1 response [29]. IL-10 is an anti-inflammatory cytokine that has been found to be increased in atopic asthmatics [19] and decreased in nonatopic asthma [20]. This finding is supported by our study as we found that the high FeNO group, which consisted of atopic asthmatics and nonasthmatic atopics, had elevated levels of IL-10. This finding likely reflects a baseline level of low grade inflammation among atopic individuals, which leads to the secretion of IL-10. Studies have shown that an increase in IL-10 in areas of allergic inflammation is thought to be a physiologic response to counteract the inflammatory process [30].
Our study has some potential shortcomings. First, our sample size is relatively small and specifically we were only able to recruit a limited number of nonatopic asthmatics, which may have skewed our results. Second, although we did follow asthma symptoms longitudinally, we did not use a validated questionnaire, such as the asthma control test. Third, although we do have information on prednisone use throughout the study, we do not have details regarding dosing and duration of use. Fourth, skin testing was used to determine the atopic status of subjects rather than a more sensitive panel of serum-specific IgE antibodies. Lastly, the Luminex may have too high a lower limit of detection for IL-1β, IL-4, IL-13, and IFN-γ (>20 % of undetectable values) in relatively healthy children, which may affect the interpretation of our results.
Despite these limitations, our study shows that FeNO is a significant marker of airway inflammation only in atopic asthmatics. We found that an elevation in FeNO likely represents an underlying atopic phenotype, and it may be more a relevant biomarker of atopy rather than of asthma. Thus, the clinical utility of an elevated FeNO among asthmatics may simply lie in the ability to identify atopic asthmatics rather than as a tool for asthma diagnosis and disease management.
References
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. http://www.ginasthma.org/local/uploads/files/GINA_Report_2012Feb13.pdf
Alving K, Weitzberg E, Lundberg J (1993) Increased amount of nitric oxide in exhaled air of asthmatics. Eur Respir J 6:1368–1370
Kharitonov S, Yates D, Barnes P (1996) Inhaled glucocorticoids decrease nitric oxide in exhaled air of asthmatic patients. Am J Respir Crit Care Med 153:454–457
Kharitonov S, Chung K, Evans D, O’Connor BJ, Barnes PJ (1996) Increased exhaled nitric oxide in asthma is mainly derived from the lower respiratory tract. Am J Respir Crit Care Med 153:1773–1780
Scott M, Raza A, Karmaus W (2010) Influence of atopy and asthma on exhaled nitric oxide in an unselected birth cohort study. Thorax 65:258–262
Lex C, Ferreira F, Zacharasiewicz A, Nicholson AG, Haslam PL, Wilson NM, Hansel TT, Payne DN, Bush A (2006) Airway eosinophilia in children with severe asthma: predictive values of noninvasive tests. Am J Respir Crit Care Med 174:1286–1291
Warke TJ, Fitch PS, Brown V, Taylor R, Lyons JD, Ennis M, Shields MD (2002) Exhaled nitric oxide correlates with airway eosinophils in childhood asthma. Thorax 57:383–387
Sippel JM, Holden WE, Tilles SA et al (2000) Exhaled nitric oxide levels correlate with measures of disease control in asthma. J Allergy Clin Immunol 106:645–650
Gelb AF, Flynn TC, Shinar CM et al (2006) Role of spirometry and exhaled nitric oxide to predict exacerbations in treated asthmatics. Chest 129:1492–1499
Buchvald F, Eiberg H, Bisgaard H (2003) Heterogeneity of FeNO response to inhaled steroid in asthmatic children. Clin Exp Allergy 33:1735–1740
de Bot CM, Moed H, Bindels PJ, van Wijk RG, Berger MY, de Groot H, de Jongste JC, van der Wouden JC (2013) Exhaled nitric oxide measures allergy not symptoms in children with allergic rhinitis in primary care: a prospective cross-sectional and longitudinal cohort study. Prim Care Respir J 22:44–50
Dupont LJ, Demedts MG, Verleden GM (2003) Prospective evaluation of the validity of exhaled nitric oxide for diagnosis of asthma. Chest 123:751–756
Crane J, Lampshire P, Wickens K, Epton M (2012) Asthma, atopy and exhaled nitric oxide in a cohort of 6-yr-old New Zealand children. Pediatr Allergy Immunol 23:59–64
Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, Olin AC, Plummer AL, Taylor DR (2011) An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FeNO) for clinical applications. Am J Respir Crit Care Med 184:602–615
Robinson CL, Baumann LM, Romero K, Combe JM, Gomez A, Gilman RH, Cabrera L, Gonzalvez G, Hansel NN, Wise RA, Barnes KC, Breysse PN, Checkley W (2011) Effect of urbanisation on asthma, allergy and airways inflammation in a developing country setting. Thorax 66:1051–1057
Poon AH, Eidelman DH, Martin JG, Laprise C, Hamid Q (2012) Pathogenesis of severe asthma. Clin Exp Allergy 42:625–637
Lykouras D, Sampsonas F, Karparianos A, Karkoulias K, Spiropoulos K (2008) Role and pharmacogenomics of TNF-alpha in asthma. Mini Rev Med Chem 8:934–942
Desai D, Brightling C (2009) Cytokine and anti-cytokine therapy in asthma: ready for the clinic? Clin Exp Immunol 158:10–19
Wong CK, Ho CY, Ko FW, Chan CH, Ho AS, Hui DS, Lam CW (2001) Proinflammatory cytokines (IL-17, IL-6, IL-18 and IL-12) and Th cytokines (IFN-gamma, IL-4, IL-10 and IL-13) in patients with allergic asthma. Clin Exp Immunol 125:177–183
John M, Lim S, Seybold J, Jose P, Robichaud A, O’Connor B, Barnes PJ, Chung KF (1998) Inhaled corticosteroids increase interleukin-10 but reduce macrophage inflammatory protein-1alpha, granulocyte-macrophage colony-stimulating factor, and interferon-gamma release from alveolar macrophages in asthma. Am J Respir Crit Care Med 157:256–262
Robinson CL, Baumann LM, Gilman RH, Romero K, Combe JM, Cabrera L, Hansel NN, Barnes K, Gonzalvez G, Wise RA, Breysse PN, Checkley W (2012) The Peru Urban versus Rural Asthma (PURA) Study: methods and baseline quality control data from a cross-sectional investigation into the prevalence, severity, genetics, immunology and environmental factors affecting asthma in adolescence in Peru. BMJ Open 2(1):e000421
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J (2005) ATS/ERS Task Force: standardization of spirometry. Eur Respir J 26:319–338
Hankinson JL, Odencrantz JR, Fedan KB (1999) Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 159:179–187
Linhares D, Jacinto T, Pereira AM (2011) Effects of atopy and rhinitis on exhaled nitric oxide values—a systematic review. Clin Transl Allergy 1:8
Dweik RA, Sorkness RL, Wenzel S (2010) Use of exhaled nitric oxide measurement to identify a reactive, at-risk phenotype among patients with asthma. Am J Respir Crit Care Med 181:1033–1041
Choi BS, Kim KW, Lee YI, Park HB, Kim YH, Sohn MH, Kim KE (2011) Exhaled nitric oxide is associated with allergic inflammation in children. J Korean Med Sci 26:1265–1269
Sutherland TJ, Taylor DR, Sears MR (2007) Association between exhaled nitric oxide and systemic inflammatory markers. Ann Allergy Asthma Immunol 99:334–339
Ingram JL, Kraft M (2012) IL-13 in asthma and allergic disease: asthma phenotypes and targeted therapies. J Allergy Clin Immunol 130:829–842
Wang XQ, Hu GH, Kang HY, Shen Y, Hong SL (2013) Significance of the IL-6 pathway in nasal polyposis in Chinese patients. Asian Pac J Allergy Immunol 31:11–19
Grimbaldeston MA, Nakae S, Kalesnikoff J, Tsai M, Galli SJ (2007) Mast cell-derived interleukin 10 limits skin pathology in contact dermatitis and chronic irradiation with ultraviolet B. Nat Immunol 8:1095–1104
Acknowledgments
This study was supported in part by the Johns Hopkins Center for Global Health. Mary Elmasri and Karina Romero were Fogarty International Center Research Fellows during the conduct of this work (R25TW009340). Colin Robinson was a Fogarty International Clinical Research Scholar during the time of this work and was further supported by Tufts University School of Medicine. Lauren Baumann was supported by a pre-doctoral NIH T35 Training Grant (T35AI065385). Nadia Hansel and William Checkley were supported by a R01 grant from the National Institutes of Environmental Health Sciences (R01ES018845). William Checkley was further supported by a Pathway to Independence Award (R00HL096955) from the National Heart, Lung and Blood Institute, National Institutes of Health and by a contract (HHSN268200900033C) with the National Heart, Lung and Blood Institute, National Institutes of Health. Study sponsors played no role in the study design, data collection, data analysis, data interpretation or the decision to submit the article for publication.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Other PURA Study Investigators Include
Juan Combe (A.B. PRISMA, Lima, Peru), Alfonso Gomez (A.B. PRISMA, Lima, Peru), Guillermo Gonzalvez (PAHO Lima, Peru), Lilia Cabrera (A.B. PRISMA, Lima, Peru), Kathleen Barnes (Johns Hopkins University, Baltimore, MD), Robert Wise (Johns Hopkins University, Baltimore, MD), Patrick Breysse (Johns Hopkins University, Baltimore, MD), D’Ann Williams (Johns Hopkins University, Baltimore, MD).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elmasri, M., Romero, K.M., Gilman, R.H. et al. Longitudinal Assessment of High Versus Low Levels of Fractional Exhaled Nitric Oxide Among Children with Asthma and Atopy. Lung 192, 305–312 (2014). https://doi.org/10.1007/s00408-013-9551-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-013-9551-8