Abstract
An excess of neutrophils in the alveoli and lung interstitium has been described in idiopathic pulmonary fibrosis (IPF). Engagement of neutrophil Fcγ receptors with IgG complexes may contribute to the pathogenesis of IPF. The neutrophil FcγRIIIb receptor occurs in two codominantly expressed allelic variants, NA1 and NA2, which exhibit different binding affinities for IgG1 and IgG3 subclasses. The aim of this study was to investigate whether FcγRIIIb genotype is associated with IPF susceptibility or disease progression. In a case-control study we compared the distribution of FcγRIIIb NA1/2 polymorphisms in 142 patients with IPF and in 218 controls using allele-specific PCR amplification. Significant skewing in the distribution of FcγRIIIb genotypes was observed between patients with IPF and control subjects. In the IPF cohort, there was higher frequency of the NA1/NA1 genotype (0.19 vs. 0.07), and lower NA2/NA2 frequency (0.31 vs. 0.50; χ2 = 17.71, df = 2, P < 0.001). The overall frequency of the NA1 allele was increased in IPF patients compared to controls (0.44 vs. 0.29; P < 0.0001, odds ratio [OR] = 1.93, 95% confidence interval [CI] = 1.42–2.64). Heterozygotes and homozygotes of the NA1 allele were at higher risk of developing IPF (OR = 2.19, 95% CI = 1.40–3.41, P = 0.0005), whereas the NA2 allele was protective against IPF (OR = 0.34, 95% CI = 0.17–0.65, P = 0.0014). There was no association of FcγRIIIb genotype with disease progression as assessed by serial lung function measurements. FcγRIIIb NA1/2 polymorphisms are associated with IPF disease susceptibility. These results support a role for immunological mechanisms contributing to IPF pathogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic pulmonary fibrosis (IPF) is a devastating lung disease of unknown etiology that carries a poor prognosis and for which there is no effective treatment. Histologically, IPF is characterized by areas of fibrosis of various ages interspersed with normal lung [1]. This pattern of disease could be explained by repeated episodes of lung injury separated in time and place followed by an abnormal wound-healing response characterized by excessive fibrosis.
Although in IPF the nature of the initiating lung injury is unknown, several lines of evidence support a role for immune complex-mediated lung injury: (1) lung fibrosis indistinguishable from IPF occurs in patients with autoimmune rheumatic diseases such as rheumatoid arthritis; (2) end-stage lung fibrosis may ensue in chronic hypersensitivity pneumonitis, the archetypal immune complex-mediated lung disease; (3) pulmonary fibrosis can be stimulated by immune complex-mediated lung injury in animal models [2, 3]; and (4) immune complexes have been detected in the serum and the lung of patients with IPF [4–12].
Neutrophil infiltration to the alveolar spaces is a characteristic feature of early IPF [13, 14] and there is an excess of neutrophils in the bronchoalveolar (BAL) fluid from IPF patients [15, 16]. Neutrophils bind immune complexes via the low-affinity IgG receptors FcγRIIa and FcγRIIIb [17], engagement of which triggers proinflammatory cascades, cell activation, and the production and release of histotoxic compounds [18, 19]. Since neutrophils and immune complexes have been linked to the development of IPF and FcγRIIIb is exclusively expressed by neutrophils [20], we hypothesized that genetic variation within the FCGR3B gene would be a genetic determinant for disease susceptibility. FcγRIIIb occurs in two codominantly expressed allelic variants with differential affinity for certain IgG subclasses [21]. In particular, FcγRIIIb is characterized by the presence of the NA1/NA2 polymorphic variants that comprise one synonymous and four nonsynonymous mutations, which affect N-linked glycosylation of the receptor and consequently the binding affinity for certain IgG subclasses (IgG1 and IgG3). The NA1 allele exhibits higher affinity for IgG1 and IgG3, and neutrophils from NA1 homozygous donors have been demonstrated to have increased capacity for phagocytosis of IgG1- and IgG3-opsonized particles [22, 23]. We have therefore investigated whether FcγRIIIb polymorphisms are associated with the pathogenesis and progression of IPF.
Materials and Methods
Subjects
IPF (n = 142) was diagnosed in patients attending a clinic specializing in interstitial lung disease according to the ATS/ERS International Multidisciplinary Consensus Classification [16]. Surgical lung biopsy and/or BAL were performed in cases for which a confident diagnosis based on clinical, functional, and radiological grounds was not possible. A consensus diagnosis was made in each case following joint review by two respiratory clinicians and a radiologist (and a pathologist for cases in which biopsy was performed). The control group (n = 218) comprised healthy blood donors and age-matched patients with lung pathologies other than an interstitial lung disease. All the study subjects were ethnically matched (British) Caucasians and provided informed consent. Ethical approval was obtained from Lothian Research Ethics Committee (LREC/2002/4/65).
Pulmonary function tests at baseline and at 6 and 12 months (±1 month) following diagnosis were recorded to assess disease progression in 121 patients with IPF. The remaining 21 patients were lost to follow-up or were unfit to perform further testing.
Allele-specific PCR Amplification
Genomic DNA was extracted from peripheral venous blood using a QIAamp DNA Blood Midi Kit (Qiagen, Crawley, West Sussex, UK). FcγRIIIb NA1/2 polymorphisms were determined in 50-μl PCR reactions using allele-specific PCR primer pairs as previously described [24]. The efficiency and specificity of the allele-specific PCR genotyping was validated by direct sequencing using Applied Biosystems (Birchwood, Warrington, UK) Big-Dye 3.1 chemistry on an Applied Biosystems model 3730 automated capillary DNA sequencer (College of Life Sciences, University of Dundee, UK).
Flow Cytometry
Neutrophil granulocytes were isolated by dextran sedimentation and discontinuous Percoll gradient centrifugation [17] from citrated peripheral venous blood drawn from subjects previously typed as NA1/NA1, NA1/NA2, and NA2/NA2. Neutrophils were immunolabelled, as previously described [25], using either allotype-specific mouse monoclonal antibodies (10 μg ml−1) against human FcγRIIIb (NA1: CLB-gran/11, mouse IgG2a; NA2: GRM-1, mouse IgG2a) [21, 26] or isotype negative control monoclonal antibody (UPC-10, mouse IgG2a; Sigma, Poole, Dorset, UK), followed by Alexa Fluor 488-conjugated goat anti-mouse F(ab′)2 (Invitrogen, Renfrew, Paisley, UK). Surface expression of FcγRIIIb (NA1 or NA2) was assessed by flow cytometry using a BD FACScan flow cytometer (BD Biosciences, Oxford, UK) and data were analyzed using BD CellQuest (BD Biosciences) or FlowJo software (Tree Star, Inc., Ashland, OR).
Statistical Analysis
Hardy–Weinberg equilibrium was assessed by a χ2 test with one degree of freedom. Differences in the genotype and allele frequencies between control and IPF patients were analyzed by the χ2 test or Fisher’s exact test. One-way analysis of variance (ANOVA) was used to test for differences in the mean values of quantitative variables. Unless otherwise stated, quantitative data are presented as mean ± SD and P < 0.05 was considered to be statistically significant. Data were analyzed using GraphPad Prism software (GraphPad Software, Inc., La Jolla, CA).
Results
IPF is Associated with Increased Frequency of the NA1 Allele of FcγRIIIb
A total of 142 IPF patients were diagnosed. The baseline characteristics of the IPF cohort are summarized in Table 1. Significant skewing in the distribution of the three FcγRIIIb genotypes (NA1/1, NA1/2, NA2/2) was observed between IPF patients and control subjects (Table 2). In the IPF cohort there was higher frequency of the NA1/NA1 genotype (0.19 vs. 0.07) and lower NA2/NA2 genotype frequency (0.31 vs. 0.50; χ2 = 17.71, df = 2, P < 0.001). Similarly, the overall frequency of the NA1 allele was increased in IPF patients compared to controls (0.44 vs. 0.29; odds ratio [OR] = 1.93; 95% confidence interval [CI] = 1.42–2.64, P < 0.0001). Heterozygotes and homozygotes of the NA1 allele (NA1/NA1 + NA1/NA2) were associated with higher risk of IPF (OR = 2.19; 95% CI = 1.40–3.41, P = 0.0005), while the presence of the NA2 allele had a protective effect against IPF (OR = 0.34; 95% CI = 0.17–0.65, P = 0.0014). Risk analysis of the NA1 allele revealed an additive association of this allele with disease susceptibility, with NA1 homozygotes being at higher risk than NA1/2 heterozygous ones (NA1/1 vs. NA2/2 OR = 4.14; 95% CI = 2.03–8.43, P = 0.0001; NA1/2 vs. NA2/2 OR = 2.23; 95% CI = 1.12–4.45, P = 0.0257).
There was agreement between genotypes observed and those predicted by the Hardy–Weinberg equilibrium in the control population (χ2 = 0.53, P = 0.47) and in the IPF group (χ2 = 0.03, P = 0.86). The specificity of PCR-based genotyping was validated by direct sequencing and by immunolabelling of isolated neutrophil granulocytes using monoclonal antibodies that specifically recognize the epitopes of the NA1 and NA2 alleles (Fig. 1) [21, 26].
Determination of FcγRIIIb NA1/2 genotypes. Genomic DNA was extracted from peripheral blood obtained from the participating subjects and the FcγRIIIb NA1/2 genotypes were determined by PCR amplification using allele-specific primer pairs, as previously described [24]. a Representative PCR amplification products from NA1/NA1, NA1/NA2, and NA2/NA2 donors, using NA1 [1]- or NA2 [2]-specific primers [24]. The efficiency and specificity of the PCR genotyping were validated using direct sequencing on an Applied Biosystems 3730 automated capillary DNA sequencer (College of Life Sciences, University of Dundee, UK). b As an additional control, neutrophil granulocytes were isolated by dextran sedimentation and discontinuous Percoll gradient centrifugation (described in [17]) from peripheral venous blood drawn from subjects previously typed as NA1/NA1, NA1/NA2, and NA2/NA2. Genotypes were confirmed using allotype-specific antibodies [21, 26]. Representative flow cytometry histogram overlays of neutrophils that were immunolabelled with allotype-specific monoclonal antibodies [for NA1: CLB-gran/11 (thick line); for NA2: GRM-1(gray-filled)]
NA1/2 Polymorphisms have No Effect on IPF Disease Progression
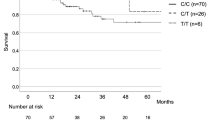
We next determined whether FcγRIIIb NA1/2 polymorphisms are also associated with IPF progression. Serial pulmonary function measurements were collected during a follow-up period of 12 months in order to assess disease progression in 121 patients with IPF. In IPF, a drop of 10% or more in forced vital capacity (FVC) or 15% or more in diffusing capacity for carbon monoxide (Dl CO, marker for gas exchange capacity of the lung) from baseline in the first 12 months is generally associated with poor prognosis and a more progressive disease phenotype. Therefore, patients were categorized as either rapid progressors (n = 49) or slow progressors (n = 72) based on whether they displayed a fall from baseline of 10% or more in FVC or 15% or more in Dl CO in 12 months [15, 27–29]. Baseline measurements were similar between rapid and slow progressors (data not shown). Both rapid and slow progressor groups displayed similar genotype frequencies and no significant skewing in the genotype distribution was noted between the groups (χ2 = 0.32, df = 2, P = 0.85) (rapid progressors: NA1/1: 0.18, NA1/2: 0.49, NA2/2: 0.33; slow progressors: NA1/1: 0.17, NA1/2: 0.54, NA2/2: 0.29). Similarly, the percentage change in FVC and Dl CO in 12 months was similar for the three FcγRIIIb genotypes (Fig. 2), thereby excluding a role of FcγRIIIb NA1/2 polymorphisms in disease progression and aggressiveness.
NA1/2 polymorphisms are not associated with IPF progression. In IPF, a drop of 10% or more in FVC or 15% or more in Dl CO from baseline in the first 12 months is generally associated with poor prognosis [15]. Serial measurements of FVC and Dl CO were recorded at 12 months following baseline (date of first radiologic evidence for IPF) to determine whether FcγRIIIb NA1/2 polymorphisms are associated with deterioration in lung function, indicative of disease progression. No significant association between the FcγRIIIb genotypes and the percent change in FVC (a) and Dl CO (b) at 12 months following baseline was evident [for FVC: P = 0.28, nonsignificant (NS); for Dl CO: P = 0.41, NS). Results are presented as mean ± 95% confidence interval (CI)
Discussion
In this study we aimed to determine the association of FcγRIIIb NA1/2 polymorphisms with IPF disease susceptibility and progression. Given the substantial evidence that supports a clear role for immunological mechanisms, and more precisely for immune complexes, in IPF pathogenesis, we focused particularly on the low-affinity IgG receptor FcγRIIIb. Although a number of single-nucleotide polymorphisms (SNPs) have been described for Fcγ receptor genes, only a small number have a clear, well-established functional significance [20]. Among them, the FcγRIIIb NA1/2 polymorphisms exhibit differential affinity for human IgG subclasses and have been associated with a number of chronic inflammatory and autoimmune disorders (reviewed in [20]). In the present study, increased frequency of NA1 homozygotes along with overrepresentation of the NA1 allele was observed among patients with IPF.
In contrast, no significant association of the FcγRIIIb NA1/NA2 polymorphism with IPF disease progression was evident. Furthermore, since the baseline pulmonary function was similar irrespective of the NA1/NA2 genotype, disease severity at presentation might also not be linked with this polymorphism. Therefore, it could be suggested that FcγRIIIb-mediated interactions play a key role only during the initial stages of the disease pathogenesis, thereby altering disease susceptibility but not severity or progression.
FcγRIIIb is expressed exclusively by neutrophils, so our findings support the pathogenic potential of this leukocyte subset in IPF. Uncontrolled recruitment or activation of neutrophils has been shown to be an important pathogenic mechanism in a variety of inflammatory diseases [30]. Interactions of immune complexes, which have been reported to be present in blood and lung tissue in IPF, with neutrophils through Fcγ-mediated binding can trigger a range of effector and immunoregulatory functions, including degranulation, phagocytosis, and cell activation [31]. Such processes consequently lead to the production of histotoxic compounds, including proteolytic enzymes and reactive oxygen and nitrogen intermediates [19]. Ensuing damage to the alveolar walls and pulmonary interstitium could lead to fibroblast activation and aberrant deposition of fibrotic tissue, which characterize IPF.
In addition to the present study, association of the NA1 allele has also been reported for a number of diseases, including vasculitis and periodontitis, which are characterized by extensive tissue damage as a result of chronic and persistent inflammation [20]. The presence of the NA1 allotype on the neutrophil surface is likely to lower the threshold for neutrophil activation by immune complexes containing IgG1 and IgG3, the two most abundant IgG subclasses in serum. Increased neutrophil activation would enhance tissue damage and act as a key determinant for the establishment and progression of the disease.
Over the last decade, studies on the pathogenesis of IPF have suggested a strong genetic component for disease susceptibility and progression. Several reports describe associations of IPF with genes involved in proinflammatory pathways, including cytokines, chemokines, their corresponding receptors, as well as with genes having a role in tissue repair and fibrogenesis, such as TGF-β [32–43]. All these studies, along with the findings presented here, suggest that a number of different genes, mainly with a strong proinflammatory potential, are involved independently in disease pathogenesis. One of the main future challenges will be the identification of the precise mechanisms and pathways that confer disease susceptibility, as their therapeutic modulation could potentially influence disease pathogenesis and progression.
References
Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, Jain A, Strawderman RL, Flint A, Lynch JP, Martinez FJ (2001) Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med 164:1722–1727
Bellon B, Bernaudin JF, Mandet C, Chamak B, Kuhn J, Druet P (1982) Immune complex-mediated lung injury produced by horseradish peroxidase (HRP) and anti-HRP antibodies in rats. Am J Pathol 107:16–24
Ward PA (1979) Immune complex injury of the lung. Am J Pathol 97:85–92
Wallace WA, Roberts SN, Caldwell H, Thornton E, Greening AP, Lamb D, Howie SE (1994) Circulating antibodies to lung protein(s) in patients with cryptogenic fibrosing alveolitis. Thorax 49:218–224
Dall’Aglio PP, Pesci A, Bertorelli G, Brianti E, Scarpa S (1988) Study of immune complexes in bronchoalveolar lavage fluids. Respiration 54(Suppl 1):36–41
Dreisin RB, Schwarz MI, Theofilopoulos AN, Stanford RE (1978) Circulating immune complexes in the idiopathic interstitial pneumonias. N Engl J Med 298:353–357
Gelb AF, Dreisen RB, Epstein JD, Silverthorne JD, Bickel Y, Fields M, Border WA, Taylor CR (1983) Immune complexes, gallium lung scans, and bronchoalveolar lavage in idiopathic interstitial pneumonitis-fibrosis. Chest 84:148–153
Haslam PL, Thompson B, Mohammed I, Townsend PJ, Hodson ME, Holborow EJ, Turner-Warwick M (1979) Circulating immune complexes in patients with cryptogenic fibrosing alveolitis. Clin Exp Immunol 37:381–390
Martinet Y, Haslam PL, Turner-Warwick M (1984) Clinical significance of circulating immune complexes in ‘lone’ cryptogenic fibrosing alveolitis and those with associated connective tissue disorders. Clin Allergy 14:491–497
Dobashi N, Fujita J, Murota M, Ohtsuki Y, Yamadori I, Yoshinouchi T, Ueda R, Bandoh S, Kamei T, Nishioka M, Ishida T, Takahara J (2000) Elevation of anti-cytokeratin 18 antibody and circulating cytokeratin 18: anti-cytokeratin 18 antibody immune complexes in sera of patients with idiopathic pulmonary fibrosis. Lung 178:171–179
Dobashi N, Fujita J, Ohtsuki Y, Yamadori I, Yoshinouchi T, Kamei T, Tokuda M, Hojo S, Bandou S, Ueda Y, Takahara J (2000) Circulating cytokeratin 8:anti-cytokeratin 8 antibody immune complexes in sera of patients with pulmonary fibrosis. Respiration 67:397–401
Takahashi T, Wada I, Ohtsuka Y, Munakata M, Homma Y, Kuroki Y (2007) Autoantibody to alanyl-tRNA synthetase in patients with idiopathic pulmonary fibrosis. Respirology 12:642–653
Gadek J, Hunninghake G, Zimmerman R, Kelman J, Fulmer J, Crystal RG (1979) Pathogenetic studies in idiopathic pulmonary fibrosis. Control of neutrophil migration by immune complexes. Chest 75:264–265
Hunninghake GW, Gadek JE, Lawley TJ, Crystal RG (1981) Mechanisms of neutrophil accumulation in the lungs of patients with idiopathic pulmonary fibrosis. J Clin Invest 68:259–269
Bradley B, Branley HM, Egan JJ, Greaves MS, Hansell DM, Harrison NK, Hirani N, Hubbard R, Lake F, Millar AB, Wallace WAH, Wells AU, Whyte MK, Wilsher ML (2008) Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax 63(Suppl 5):v1–v58
American Thoracic Society, European Respiratory Society (2002) American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med 165:277–304
Bournazos S, Hart SP, Chamberlain LH, Glennie MJ, Dransfield I (2009) Association of FcγRIIa (CD32a) with lipid rafts regulates ligand binding activity. J Immunol 182:8026–8036
Green JM, Schreiber AD, Brown EJ (1997) Role for a glycan phosphoinositol anchor in Fcγ receptor synergy. J Cell Biol 139:1209–1217
Nathan C (2006) Neutrophils and immunity: challenges and opportunities. Nat Rev Immunol 6:173–182
Bournazos S, Woof JM, Hart SP, Dransfield I (2009) Functional and clinical consequences of Fc receptor polymorphic and copy number variants. Clin Exp Immunol 157:244–254
Salmon JE, Edberg JC, Kimberly RP (1990) Fcγ receptor III on human neutrophils. Allelic variants have functionally distinct capacities. J Clin Invest 85:1287–1295
Ory PA, Clark MR, Kwoh EE, Clarkson SB, Goldstein IM (1989) Sequences of complementary DNAs that encode the NA1 and NA2 forms of Fc receptor III on human neutrophils. J Clin Invest 84:1688–1691
Ory PA, Clark MR, Talhouk AS, Goldstein IM (1991) Transfected NA1 and NA2 forms of human neutrophil Fc receptor III exhibit antigenic and structural heterogeneity. Blood 77:2682–2687
De Haas M, Kleijer M, van Zwieten R, Roos D, von dem Borne AE (1995) Neutrophil FcγRIIIb deficiency, nature, and clinical consequences: a study of 21 individuals from 14 families. Blood 86:2403–2413
Bournazos S, Rennie J, Hart S, Fox KAA, Dransfield I (2008) Monocyte functional responsiveness after PSGL-1-mediated platelet adhesion is dependent on platelet activation status. Arterioscler Thromb Vasc Biol 28:1491–1498
Trounstine ML, Peltz GA, Yssel H, Huizinga TW, Von dem Borne AE, Spits H, Moore KW (1990) Reactivity of cloned, expressed human FcγRIII isoforms with monoclonal antibodies which distinguish cell-type-specific and allelic forms of FcγRIII. Int Immunol 2:303–310
Hanson D, Winterbauer RH, Kirtland SH, Wu R (1995) Changes in pulmonary function test results after 1 year of therapy as predictors of survival in patients with idiopathic pulmonary fibrosis. Chest 108:305–310
Latsi PI, du Bois RM, Nicholson AG, Colby TV, Bisirtzoglou D, Nikolakopoulou A, Veeraraghavan S, Hansell DM, Wells AU (2003) Fibrotic idiopathic interstitial pneumonia: the prognostic value of longitudinal functional trends. Am J Respir Crit Care Med 168:531–537
Flaherty KR, Mumford JA, Murray S, Kazerooni EA, Gross BH, Colby TV, Travis WD, Flint A, Toews GB, Lynch JP, Martinez FJ (2003) Prognostic implications of physiologic and radiographic changes in idiopathic interstitial pneumonia. Am J Respir Crit Care Med 168:543–548
Weiss SJ (1989) Tissue destruction by neutrophils. N Engl J Med 320:365–376
Ravetch JV, Bolland S (2001) IgG Fc receptors. Annu Rev Immunol 19:275–290
Whyte M, Hubbard R, Meliconi R, Whidborne M, Eaton V, Bingle C, Timms J, Duff G, Facchini A, Pacilli A, Fabbri M, Hall I, Britton J, Johnston I, Di Giovine F (2000) Increased risk of fibrosing alveolitis associated with interleukin-1 receptor antagonist and tumor necrosis factor-α gene polymorphisms. Am J Respir Crit Care Med 162:755–758
Checa M, Ruiz V, Montaño M, Velázquez-Cruz R, Selman M, Pardo A (2008) MMP-1 polymorphisms and the risk of idiopathic pulmonary fibrosis. Hum Genet 124:465–472
Molina-Molina M, Xaubet A, Li X, Abdul-Hafez A, Friderici K, Jernigan K, Fu W, Ding Q, Pereda J, Serrano-Mollar A, Casanova A, Rodríguez-Becerra E, Morell F, Ancochea J, Picado C, Uhal BD (2008) Angiotensinogen gene G-6A polymorphism influences idiopathic pulmonary fibrosis disease progression. Eur Respir J 32:1004–1008
Mushiroda T, Wattanapokayakit S, Takahashi A, Nukiwa T, Kudoh S, Ogura T, Taniguchi H, Kubo M, Kamatani N, Nakamura Y, Group PCS (2008) A genome-wide association study identifies an association of a common variant in TERT with susceptibility to idiopathic pulmonary fibrosis. J Med Genet 45:654–656
Pantelidis P, Fanning GC, Wells AU, Welsh KI, Du Bois RM (2001) Analysis of tumor necrosis factor-α, lymphotoxin-α, tumor necrosis factor receptor II, and interleukin-6 polymorphisms in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 163:1432–1436
Riha RL, Yang IA, Rabnott GC, Tunnicliffe AM, Fong KM, Zimmerman PV (2004) Cytokine gene polymorphisms in idiopathic pulmonary fibrosis. Intern Med J 34:126–129
Selman M, Lin HM, Montaño M, Jenkins AL, Estrada A, Lin Z, Wang G, DiAngelo SL, Guo X, Umstead TM, Lang CM, Pardo A, Phelps DS, Floros J (2003) Surfactant protein A and B genetic variants predispose to idiopathic pulmonary fibrosis. Hum Genet 113:542–550
Vasakova M, Striz I, Dutka J, Slavcev A, Jandova S, Kolesar L, Sulc J (2007) Cytokine gene polymorphisms and high-resolution-computed tomography score in idiopathic pulmonary fibrosis. Respir Med 101:944–950
Vasakova M, Striz I, Slavcev A, Jandova S, Kolesar L, Sulc J (2006) Th1/Th2 cytokine gene polymorphisms in patients with idiopathic pulmonary fibrosis. Tissue Antigens 67:229–232
Whittington HA, Freeburn RW, Godinho SIH, Egan J, Haider Y, Millar AB (2003) Analysis of an IL-10 polymorphism in idiopathic pulmonary fibrosis. Genes Immun 4:258–264
Xaubet A, Marin-Arguedas A, Lario S, Ancochea J, Morell F, Ruiz-Manzano J, Rodriguez-Becerra E, Rodriguez-Arias JM, Inigo P, Sanz S, Campistol JM, Mullol J, Picado C (2003) Transforming growth factor-β1 gene polymorphisms are associated with disease progression in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 168:431–435
Zorzetto M, Ferrarotti I, Trisolini R, Agli LL, Scabini R, Novo M, De Silvestri A, Patelli M, Martinetti M, Cuccia M, Poletti V, Pozzi E, Luisetti M (2003) Complement receptor 1 gene polymorphisms are associated with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 168:330–334
Acknowledgments
We are grateful to Dr. Andrew Robson for his help in obtaining lung function measurements and Dr. Zhe Hui Hoo for his help and comments. We also thank all the past members from our group (Centre for Inflammation Research, UK) and all the subjects who participated in this study. This work was supported by grants from the British Heart Foundation (FS/05/119/19568) and the Medical Research Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bournazos, S., Bournazou, I., Murchison, J.T. et al. Fcγ Receptor IIIb (CD16b) Polymorphisms are Associated with Susceptibility to Idiopathic Pulmonary Fibrosis. Lung 188, 475–481 (2010). https://doi.org/10.1007/s00408-010-9262-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-010-9262-3