Abstract
The role of airway inflammation in mediating airflow obstruction in persons with chronic traumatic tetraplegia is unknown. Measurement of the fraction of exhaled nitric oxide (FeNO) affords a validated noninvasive technique for gauging the airway inflammatory response in asthma, although it has never been assessed in persons with tetraplegia. This study was designed to determine the FeNO in individuals with chronic tetraplegia compared with that in patients with mild asthma and healthy able-bodied individuals. Nine subjects with chronic tetraplegia, seven subjects with mild asthma, and seven matched healthy able-bodied controls were included in this prospective, observational, pilot study. All subjects were nonsmokers and clinically stable at the time of study. Spirometry was performed on all participants at baseline. FENO was determined online by a commercially available closed circuit, chemiluminescence method, using a single-breath technique. Subjects with tetraplegia had significantly higher values of FeNO than controls (17.72 ± 3.9 ppb vs. 10.37 ± 4.9 ppb; P ≤ 0.01), as did subjects with asthma (20.23 ± 4.64 ppb vs. 10.37 ± 4.9 ppb, P ≤ 0.001). There was no significant difference in FeNO between subjects with tetraplegia and those with asthma (17.72 ± 3.9 ppb vs. 20.23 ± 4.64 ppb, P ≤ 0.27). Individuals with chronic tetraplegia have FeNO levels that are comparable to that seen in mild asthmatics and higher than that in healthy able-bodied controls. The clinical relevance of this observation has yet to be determined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The role of airway inflammation in individuals with chronic cervical spinal cord injury (SCI) is unknown. Our research group has postulated that aspects of airway physiology characteristically seen in chronic tetraplegia are the consequence of overriding cholinergic airway tone mediated by intact vagal (parasympathetic) nerve fibers arising from the brainstem [1–4], whereas sympathetic innervation is interrupted at the level of the upper thoracic spinal cord. These physiologic responses include decrease in baseline airway caliber [4], significant bronchodilator responsiveness after inhalation of beta-2-adrenergic agonists or anticholinergic agents [4, 5], and airway hyperreactivity (AHR) [1–3]. These same aspects of airway physiology in tetraplegia also are encountered in asthma, and in asthma are closely linked to airway inflammation.
To examine the potential role of airway inflammation in persons with tetraplegia, measurement of the FeNO now offers a noninvasive methodology to assess indirectly the airway inflammatory response [6]. FeNO is markedly elevated in poorly controlled asthma due to excess NO produced by inflammatory cells within the airways [7–9], but exhaled levels in tetraplegia have heretofore never been investigated.
The purpose of this pilot investigation was to analyze FeNO levels in individuals with chronic cervical SCI compared with mild asthmatics and healthy able-bodied controls. We hypothesized that measurement of FeNO in individuals with chronic cervical SCI would give us insight into the role that airway inflammation plays and help to explain the obstructive physiology observed in this population.
Materials and Methods
This work was performed at the James J. Peters Veterans Affairs Medical Center, Bronx, NY. The study was approved by the local Institutional Review Board and Research and Development Committee. Written, informed consent was obtained from all participants prior to enrollment in the study.
Subjects
Twenty-two subjects were studied: eight with a diagnosis of chronic tetraplegia (>1 year in duration), seven with mild asthma (baseline forced expiratory volume in the first second (FEV1) >70% predicted), and seven healthy able-bodied controls. Participants were matched for age, height, weight, and body mass index (BMI). Subjects were nonsmokers (e.g., lifelong or more than 5 years since stopping). Individuals with tetraplegia and controls did not report a history of asthma or recent respiratory infection (i.e., within 3 months), and they were not taking medications that are known to alter airway caliber. Measurements of FeNO were performed at least 7 days after the last administration of inhaled or oral corticosteroid medication, 48 h after the last administration of long-acting inhaled bronchodilator medication, 24 h after the last administration of leukotriene modifiers, and/or at least 12 h after the last administration of short-acting inhaled bronchodilator medication.
The following measurements were performed in all participants:
Spirometry
Spirometric measurements were performed using the VMax Encore integrated pulmonary function lab (Viasys, Yorba Linda, CA). Forced vital capacity (FVC), FEV1, and FEV1/FVC ratio are reported. All recordings were made in the seated position. At least three tests were performed in accordance to American Thoracic Society (ATS) guidelines for testing and reproducibility [10]. The highest values for FVC and FEV1 are reported.
FeNO Measurement
Exhaled NO measurements were performed in accordance to ATS recommendations for the standardization of this procedure [11]. Sievers Nitric Oxide Analyzer NOA 280 system for online measurements (Sievers Instruments, Boulder, CO) was used. Online measurement provided real-time display of exhaled NO and allowed the technician to adjust and to provide proper collection technique. Before obtaining measurements, the analyzer was calibrated according to the manufacturer’s specification. The subjects were seated comfortably with the mouth piece at the proper position and height. To avoid nasal NO accumulation and leakage contaminating the sample, nose clips were not used [11]. Subjects were instructed to breathe through their mouth and to avoid nasal breathing. Subjects were then asked to inhale to total lung capacity (TLC) and to expire against a constant expiratory resistance of 5 cm H2O to ensure velopharyngeal aperture closure and to prevent nasal NO contamination. Study subjects were provided biofeedback by displaying the flow rate on the monitor. The duration of the exhalation was sufficient to obtain a plateau in the NO concentration. Repeat exhalation measurements were performed to assure reproducibility. Testing was completed when three NO plateaus were obtained within 10% of each other. At least 30 seconds of relaxed tidal breathing subsequent to testing was provided between measurements to allow the subject to rest. Exhaled NO was reported as the mean of three values within 10% of each other.
Statistics
All data were analyzed using Statview 5.0 (SAS Institute, Inc.). Continuous data are reported as mean ± SD. A priori level of significance was set at P ≤ 0.05. Unpaired t tests were performed to identify group (control, asthma, tetraplegia) differences for demographic characteristics (age, height, weight, and BMI). Univariate analysis of variance was performed to identify group differences for the dependent variable (FeNO levels). Significant group effects were further evaluated using a Fisher PLSD post hoc test.
Results
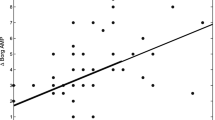
Subjects in the three groups were matched for age, height, weight and BMI; consistent with a mild restrictive ventilator defect subjects with tetraplegia had significantly lower FVC values than asthmatic or control subjects, and significantly lower FEV1 than control subjects (Table 1). FeNO levels in individuals with tetraplegia were comparable to those observed in asthmatic subjects (17.72 ± 3.9 ppb vs. 20.23 ± 4.64 ppb, P ≤ 0.27), and significantly higher than that observed in the control group (17.72 ± 3.9 ppb vs. 10.37 ± 4.9 ppb, P ≤ 0.004). Individuals with asthma had significantly higher levels of FeNO than that of the control group (20.23 ± 4.64 ppb vs. 10.37 ± 4.9 ppb, P ≤ 0.0005; Fig. 1).
Discussion
Respiratory complications are the leading cause of death during the first year after SCI, and the third leading cause of death thereafter [12]. Complete or partial loss of respiratory muscle innervation in individuals with cervical and high thoracic injuries leads to inadequate ventilation and inability to effectively clear secretions, often prompting supportive ventilation after initial injury. Development of atelectasis, pneumonia, and respiratory failure are the most common respiratory complications seen in the acute phase of injury [13]. It is well known that a restrictive ventilatory defect, dependent upon the level and completeness of injury, is apparent in individuals with chronic cervical SCI and was noted in our subjects. Respiratory functional impairment might be further compromised in these individuals, the majority of whom share many aspects of obstructive airway physiology commonly associated with asthma.
The etiology underlying obstructive physiology observed in individuals with tetraplegia has been assumed to be different from that associated with asthma. The asthma-like features that individuals with chronic cervical SCI demonstrate have been hypothesized to be due to overriding cholinergic airway tone carried by intact vagal (parasympathetic) nerve fibers arising from the brainstem [1–3], whereas sympathetic innervation is interrupted at the level of the upper thoracic spinal cord. In persons with asthma, similar pulmonary physiological responses are attributed to allergic airway inflammation. Whether airway narrowing and AHR in chronic cervical SCI also is related to chronic airway inflammation is unknown, although it is conceivable that repeated respiratory infections and/or, possibly, a neurogenic component, could contribute to an inflammatory response.
The role of NO in the respiratory tract has been the focus of extensive studies during the past decade. In the respiratory system, NO is formed and released by an array of different cells, including inflammatory, nerve, epithelial, endothelial, and airway smooth muscle cells. Nitric oxide is synthesized from the amino acid L-arginine by the enzyme NO synthase (NOS). Studies have identified the presence of three NOS isoforms in the human lung: neuronal NOS (nNOS), which is felt to be involved in the modulation of airway tone and is the principal inhibitory (bronchodilating) neurotransmitter of the non-adrenergic non-cholinergic nervous system (NANC) within the airways [14, 15]; endothelial NOS (eNOS), which is responsible for vasodilation; and inducible NOS (iNOS), which is predominantly found in macrophages and epithelial cells [15, 16]. The enzymes nNOS and eNOS are known as constitutive NOS (cNOS), and they are thought to be involved in the regulation of airway and vascular tone by local production of small amounts of NO in response to neurogenic and non-neurogenic stimuli [16]. The iNOS is stimulated by proinflammatory cytokines during airway inflammation and regulates the production of large amounts of NO in the airways and vasculature. It is apparent that iNOS produces 1,000-fold higher levels of NO than does cNOS [17], and most of exhaled NO measured in patients with asthma is thought to be iNOS-derived. In patients with asthma, high levels of NO detected in exhaled air are thought to be closely related to the degree of airway inflammation, and due to increased production of NO by the inflammatory cells. This may suggest a role of NO in the generation and maintenance of airway inflammation. On the other hand, when generated in the small amounts, NO also has a direct bronchodilatory effect on airway smooth muscle and acts as a principal neurotransmitter of the NANC system (the only known neural relaxant pathway in human airways).
Although implicated in conflicting biological mechanisms, it is now widely believed that in the airways of patients with asthma the release of NO represents a physiological mechanism to counteract the bronchoconstriction caused by various stimuli [18]. Whether the elevated levels of FeNO that we observed in individuals with chronic tetraplegia are reflective of airway inflammation due to iNOS-derived production of NO vs. altered regulation of NOS pathways (i.e., upregulation of the NANC system) is not known. Further studies are needed to define the source of elevated NO in the exhaled air of persons with tetraplegia (iNOS vs. cNOS pathway), the relationships among FeNO, the presence of underlying airway inflammation and its effects on bronchial tone, airway hyperreactivity, and overall pulmonary function in individuals with chronic tetraplegia. Confirmation of chronic underlying airway inflammation in those with tetraplegia would raise consideration for use of anti-inflammatory agents, such as inhaled steroids, as a potential therapeutic option.
References
Dicpinigaitis PV et al (1994) Bronchial hyperresponsiveness after cervical spinal cord injury. Chest 105(4):1073–1076
Singas E et al (1996) Airway hyperresponsiveness to methacholine in subjects with spinal cord injury. Chest 110(4):911–915
Grimm DR et al (1999) Airway hyperresponsiveness to ultrasonically nebulized distilled water in subjects with tetraplegia. J Appl Physiol 86(4):1165–1169
Schilero GJ, Grimm DR, Bauman WA, Lenner R, Lesser M (2005) Assessment of airway caliber and bronchodilator responsiveness in subjects with spinal cord injury. Chest 127(1):149–155
Almenoff PL, Alexander LR, Spungen AM, Lesser MD, Bauman WA (1995) Bronchodilatory effect of ipratropium bromide in patients with tetraplegia. Paraplegia 33(5):274–277
Zitt M (2005) Clinical applications of exhaled nitric oxide for the diagnosis and management of asthma: a consensus report. Clin Ther 27(8):1238–1250
Barnes PJ, Belvisi MG (1993) Nitric oxide and lung disease. Thorax 48(10):1034–1043
Barnes PJ, Liew FY (1995) Nitric oxide and asthmatic inflammation. Immunol Today 16(3):128–130
Kharitonov SA et al (1994) Increased nitric oxide in exhaled air of asthmatic patients. Lancet 343(8890):133–135
Miller MR et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338
The official statement of the American Thoracic Society (1999) Recommendations for standardized procedures for the on-line and off-line measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide in adults and children. Am J Respir Crit Care Med 160:2104–2117
DeVivo MJ, Black KJ, Stover SL (1993) Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 74(3):248–254
Jackson AB, Groomes TE (1994) Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil 75(3):270–275
Fischer A et al (1993) Nitric oxide synthase in guinea pig lower airway innervation. Neurosci Lett 149(2):157–160
Asano K, Chee CBE, Gaston B, Lilly CM, Gerard C, Drazen JM, Stamler JS (1994) Constitutive and inducible nitric oxide synthase gene expression, regulation and activity in human epithelial cells. Proc Natl Acad Sci USA 91:10089–10093
Barnes PJ, Belvisi MG (1993) Nitric oxide and lung disease. Thorax 48:1034–1043
Dweik RA, Laskowski D, Abu-Soud HM, Kaneko FT, Hutte R, Stuehr DJ, Erzurum SC (1998) Nitric oxide synthesis in the lung: regulation by oxygen through a kinetic mechanism. J Clin Invest 101:660–666
Di Maria GU, Spicuzza L, Mistretta A (2000) Role of endogenous nitric oxide in asthma. Allergy 55(Suppl 61):31–35
Acknowledgments
This work was funded by a Rehabilitation Research and Development (RR&D) Service Career Development award (B4335 V) & RR&D Center of Excellence for the Medical Consequences of Spinal Cord Injury (B4162C). The authors thank The James J. Peters Medical Center, Bronx, NY, and Department of Veterans Affairs Rehabilitation Research and Development service for their support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radulovic, M., Schilero, G.J., Wecht, J.M. et al. Exhaled Nitric Oxide Levels Are Elevated in Persons with Tetraplegia and Comparable to that in Mild Asthmatics. Lung 188, 259–262 (2010). https://doi.org/10.1007/s00408-009-9207-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-009-9207-x