Abstract
Idiopathic pulmonary fibrosis (IPF) is a chronic and usually fatal lung disease of unknown etiology. The aim of this study was to describe clinical and polysomnographic features of sleep-related breathing disorders (SRBD) and to identify predictors of obstructive sleep apnea (OSA) in IPF patients. Eight hundred fifty-seven patients with IPF were admitted to the Cleveland Clinic from 2001 to 2005. An all-night polysomnogram (PSG) was performed in 18 of them to investigate complaints suggestive of sleep-disordered breathing. OSA was confirmed in 11 of the 18 IPF patients with complaints suggestive of sleep apnea, while the remain 7 patients had a diagnosis of primary snoring or upper airway resistance syndrome (UARS). All patients showed a reduction in sleep efficiency, REM sleep, and slow wave sleep. The apnea-hypopnea index (AHI) was positively correlated with body mass index (p < 0.0001, r = 0.80). The REM AHI and overall AHI were negatively correlated with FEV1 (p = 0.008, r = −0.59 and p = 0.04, r = −0.49, respectively) and FVC percentages (p = 0.03, r = −0.50 and p = 0.08, r = −0.42, respectively). Our study is the first describing SRBD in IPF patients. An increased BMI and a significant impairment in pulmonary function testing may be predictors of OSA in this population. In the absence of effective treatments for IPF, the diagnosis and treatment of comorbid SRBD may lead to improvements in quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic pulmonary fibrosis (IPF) is the most common of the idiopathic interstitial pneumonias. It is thought to affect about 30 per 100,000 people in the general population and perhaps as many as 175 per 100,000 people in the age group 75 years and older. The outlook for patients with IPF is poor; the symptoms of breathlessness and cough are usually progressive and about 50% of patients die within 3 years of diagnosis [1–3]. The response to currently recommended treatments in terms of survival is disappointing [1].
Because of a paucity of studies in IPF patients, significant gaps remain in our understanding of how IPF affects the quality of sleep. To the best of our knowledge there are no previous studies describing obstructive sleep apnea (OSA) in IPF patients. Two studies in the mid-1980s have shown nocturnal hypoxemia, sleep fragmentation, increase in stage 1, and reduction in REM sleep in the presence of severe lung fibrosis [4, 5].The incidence of apneas and hypopneas was found to be in the normal range despite the severe oxygen desaturation during sleep. A recent study showed that nocturnal hypoxemia is common in patients with IPF and may be associated with a reduction in energy levels and impairment of physical and social functioning [6].
As a result of the rapidly progressive nature of IPF, SRBD may be markedly underdiagnosed in these patients. The aim of this retrospective study was to describe the clinical and polysomnographic features of SRBD and to identify predictors of OSA in IPF patients. Such data may facilitate early recognition of clinically significant SRBD, while treatment may reduce morbidity and improve quality of life.
Material and Methods
Subjects
Using a computer-assisted search, 857 patients with IPF evaluated at Cleveland Clinic during the period of January 1, 2001, to December 31, 2005, were identified. The diagnosis of IPF was based on strict criteria (clinical history, physical examination, roentgenographic findings, laboratory tests, pulmonary function tests, histologic findings, and the exclusion of other known causes of interstitial lung disease), according to the latest American Thoracic Society/European Respiratory Society criteria [1]. The study was approved by the Cleveland Clinic Institutional Review Board (IRB).
An overnight polysomnogram (PSG) was performed in 18 IPF patients (12 male and 6 female, median age = 68.1 years, range = 51–78 years) to investigate complaints compatible with sleep-disordered breathing. The patients completed the Cleveland Clinic Sleep Disorders Questionnaire and the Epworth Sleepiness Scale, a validated, commonly used eight-item questionnaire used to measure subjective excessive daytime sleepiness. Ten of these patients had a lung-biopsy that confirmed the diagnosis of IPF (feature of usual interstitial pneumonia in lung tissue specimen), while in the rest of these patients the diagnosis of IPF was made on the basis of the latest American Thoracic Society/European Respiratory Society criteria [1, 2]. At the time of the PSG eight patients were being treated (corticosteroids or azathioprine and corticosteroids combination). Demographic and pulmonary function testing data are summarized in Table 1.
Methods
An attended all-night PSG was performed according to established standards [7]. Multichannel recordings of the electroencephalogram (central and occipital), electro-oculogram (EOG), electromyogram (EMG), oronasal flow (by thermistor and nasal transducer), respiratory effort (by abdominal and thoracic strain gauges),oxygen saturation (pulse oximetry), snoring, and body position were recorded on a computerized workstation (Vangard, Cleveland, OH) [8].Tracheal sounds were monitored using an acoustic microphone. Studies were scored in 30–s epochs following Rechtschaffen and Kales criteria for sleep staging [9]. Apneas and hypopneas were defined by standard criteria [10]. An obstructive apnea was defined as a reduction in airflow greater than 90% lasting at least 10 s in which there was evidence of persistent respiratory effort. A central apnea was defined as a reduction in airflow of more than 90% lasting at least 10 s in which there was no evidence of respiratory effort. A hypopnea was defined as a reduction in airflow by 50% with a duration of at least 10 s or a reduction of airflow or respiratory effort by 30% for more than 10 s, accompanied by an EEG arousal and/or a 3% or greater oxygen desaturation. Arousals were defined as a change in EEG activity to a faster frequency for at least 3 s [11]. OSA was considered mild if the AHI was ≥5 per hour but < 15 per hour, moderate if ≥15 per hour but < 30 per hour, and severe if ≥30 per hour [10].
Spirometry (FEV1, FVC, FEV1/FVC ratio), measurement of static lung volumes (total lung capacity [TLC], residual volume [RV] by body box plethysmography), and measurement of diffusing capacity (diffusing capacity of the lung for carbon monoxide [DLCO] by the single-breath technique) were performed (Jaeger Compactlabs, Millbery, OH) with the patient in the seated position according to approved standards [12].
Statistical Analysis
All data are given as mean ± SD. Data were examined for normal distribution using the Kolmogorov-Smirnov test. The Pearson correlation coefficient was employed to examine the relationship between overall AHI, REM AHI, and BMI or pulmonary function testing values (normally distributed data). A p value of less than 0.05 was considered statistically significant.
Results
The PSG data are shown in Table 2. Patients had complaints of excessive daytime sleepiness (77.7%), snoring (88.8%), witnessed apneas (44.4%), and daytime fatigue (61.1%). The mean BMI was 33.2 ± 6.9 (range = 23–43.3) and the mean ESS was 9.9 ± 3.1. On PSG we noted a decrease in sleep efficiency (62.9% ± 17.8%), slow wave sleep (5.5% ± 6.7%), and REM sleep (8.6% ± 7.9%). The overall AHI was in the moderate range (25.2 ± 25.8 apneas/hypopneas per hour of sleep), while the mean arousal index was increased (29.7 ± 22.8/ hour of sleep). The diagnosis of OSA was made in 11 patients (5 had severe, 5 moderate, and 1 mild OSA) while 4 patients had the diagnosis of primary snoring. The remaining 3 patients had PSG features compatible with upper airway resistance syndrome. A PSG with esophageal pressure monitoring was recommended but not completed due to the clinical status of these patients. PLM index was elevated in seven patients (mean PLM index = 13.3 ± 24.5), while two of them were diagnosed with restless legs syndrome (RLS) and the PSG findings were compatible with the diagnosis [13, 14]. Oxygen saturation below 90% was observed during 17.7% ± 22.6% of the total sleep time.
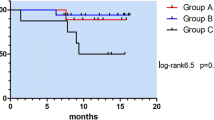
The AHI was positively correlated with body mass index (BMI) values (p < 0.0001, r = 0.80) (Fig 1). OSA was observed only in moderately to severely obese IPF patients (11 patients, BMI = 38.4 ± 3.1, range = 35.3–44.3), while UARS and primary snoring were observed in those with BMI values in the normal or overweight range (7 patients, mean BMI = 25.5 ± 3.0, range = 23–30). No statistically significant differences were found related to BMI values and severity of OSA (based on the apnea-hypopnea index) when IPF patients under treatment with corticosteroids were compared to those not receiving such treatment.
The overall AHI was negatively correlated with FEV1 values (p = 0.04, r = −0.49) and FVC percentages (p = 0.08, r = −0.42, statistically significant trend). REM AHI was negatively correlated with FEV1 and FVC percentages (p = 0.008, r = −0.59 and p = 0.03, r = −0.50, respectively) (Figs. 2a,b and 3a,b).
Discussion
This is the first study that describes SRBD in patients with IPF, a chronic and usually fatal lung disease of unknown etiology. Perez-Padilla et al. [4], in a study in the mid-1980s, observed that patients with interstitial lung disease (11 ILD patients, 7 patients with IPF) had poor sleep quality with less time in REM sleep and marked sleep fragmentation. The apnea-hypopnea index was found to be low (1.3 ± 0.45) even though hypoxemia and obesity were noted in several of these patients. Bye et al. [5], in a study from the same period that investigated patients with ILD (13 ILD patients, 3 with IPF), showed that patients with ILD had significant oxygen desaturation during REM sleep. In a more recent study, Clark et al. [6] noted that patients with IPF and pulmonary fibrosis secondary to connective tissue disorders had hypoxemia during sleep. This was associated with decreased energy levels and impaired daytime functioning and these effects were independent of FVC. Another recent study by Prado et al..[15], investigating patients with pulmonary fibrosis secondary to systemic sclerosis, showed that these patients had a very disrupted sleep, increased amount of PLMS, and increased frequency of RLS. An apparently discrepant finding contrary to their initial hypothesis was that the AHI was in the normal range suggesting the absence of OSA in this patient group. On the other hand, Turner et al. [16] found an increased incidence of OSA in patients with sarcoidosis.
The IPF terminology and the criteria for the diagnosis of IPF has been changed during the last few years and now there are strict criteria to diagnose this condition according to the latest American Thoracic Society/European Respiratory statements [1, 2]. Our study was designed to investigate sleep-disordered breathing only in patients with a confirmed diagnosis of IPF, a disease affecting only the lungs, in contrast to pulmonary fibrosis due to connective tissue disease or sarcoidosis, which affects multiple organ systems.
According to our data a very disrupted sleep was observed in all IPF patients who had a PSG to investigate complaints that were suggestive of sleep-disordered breathing. The sleep architecture in these patients showed a reduction in sleep efficiency and REM sleep, slow wave sleep, and a marked sleep fragmentation due to an increased arousal index.
Prior polysomnographic studies in this population have demonstrated alterations in sleep architecture and oxygen desaturation, especially during REM sleep, but not OSA, even in morbidly obese IPF patients. The increased respiratory drive associated with increased minute ventilation and hypocapnia has been proposed as a protective mechanism against OSA in IPF [4, 17]. Our data suggest that OSA does in fact exist at least in some IPF patients. Prior studies dating back 10–20 years underestimated respiratory events by using thermal sensors exclusively. Our data identify two factors, increased BMI and a significant impairment in pulmonary function testing (based on FVC and FEV1), as potential predictors of OSA in IPF.
Obesity is known to be an important risk factor for OSA [18–21] and our data suggest that IPF patients are not an exception to this rule.The AHI was positively correlated with BMI, while unambiguous OSA was observed only in moderately to severely obese IPF patients and lesser degrees of SRBD (UARS and primary snoring) were observed in those with BMI values in the normal or overweight range.
The second factor found to be a predictor of SRBD is the magnitude of the pulmonary function test impairment. Restrictive pulmonary diseases are characterized by decreased lung volumes that can reduce the upper airway stability and increase resistance due to a decreased traction on the upper airway. These changes can facilitate the upper airway collapse, especially during REM sleep when functional residual capacity (FRC) is further reduced due to the inactivity of the intercostal muscles [22–24]. We found a trend for a negative correlation between FVC and overall AHI but a statistically significant negative correlation between FVC and REM AHI. Therefore, obese IPF patients with significantly decreased pulmonary function parameters may be at increased risk for OSA, particularly during REM sleep.
UARS and primary snoring were diagnosed in 7 of 18 IPF patients with complaints suggestive of sleep-disordered breathing. There is evidence that nonapneic snoring is associated with daytime dysfunction and probably represents an intermediate point on the continuum of sleep-disordered breathing [25, 26]. The increased resistance to breathing during snoring may have more adverse effects in patients with IPF who have altered lung mechanics and reduced respiratory muscle power. Furthermore, UARS has been recognized as a significant cause of sleep disruption [27–31] but the gold standard test remains monitoring of esophageal pressure. This procedure is not performed routinely during PSG studies, especially in patients with severe pulmonary disease like IPF.
Another symptom especially common during the progressive course of IPF is daytime fatigue or, more precisely, exhaustion of which patients complain frequently and which negatively impacts their quality of life. Sixty-one percent of the studied patients had this complaint. Multiple factors can explain daytime fatigue in patients with severe pulmonary diseases like IPF, including sleep fragmentation and SRBD.
Our study is the first to report on SRBD in a pure IPF population; however, we suspect that our group represents a minority of actual cases at our institution. Despite growing OSA awareness among healthcare providers, we suspect that treating physicians may defer sleep testing because IPF is characterized by such a rapidly progressive course leading them to focus on more acute problems such as dyspnea and limitations in daily activities. Eleven of 18 IPF patients who were deemed sleep apnea suspects and referred for polysomnography were found to have OSA, while 3 had UARS. In the absence of an effective treatment for IPF, optimization of quality of life remains a primary therapeutic goal. We believe these findings will help to raise awareness of the potential for comorbid sleep disorders, the treatment of which may improve quality of life. Further studies are needed to identify the prevalence of SRBD in IPF and determine treatment effects.
References
American Thoracic Society/European Respiratory Society (2002) International multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 165:277–304
American Thoracic Society/European Respiratory Society (2000) Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. Am J Respir Crit Care Med 161:646–664
Coultas DB, Zumwalt RE, Black WC, Sobonya RE (1994) The epidemiology of interstitial lung disease. Am J Respir Crit Care Med 150:967–972
Perez-Padilla R, West P, Lertzman M, Kryger M (1985) Breathing during sleep in patients with interstitial lung disease. Am Rev Respir Dis 132:224–229
Bye P, Issa F, Berthon-Jones M, Sullivan C (1984) Studies of oxygenation during sleep in patients with interstitial lung disease. Am Rev Respir Dis 129:27–32
Clark M, Cooper B, Singh S, et al. (2001) A survey of nocturnal hypoxaemia and health related quality of life in patients with cryptogenic fibrosing alveolitis. Thorax 56:482–486
American Sleep Disorders Association (1997) Practice parameters for the indication for polysomnography and related procedures: Polysomnography Taske Force, American Sleep Disorders Association Standards of Practice Committee. Sleep 20:406–422
Bartolo A, Clymer B, Golish J, Burgess R (2000) The Polysomnogram Assay: A method to represent the overnight polysomnogram in a condensed format. Comput Biomed Res 33:110–125
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles, CA: Brain Information Service/Brain Research Institute, University of California at Los Angeles
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research; the report of the American Academy of Sleep Medicine task force. Sleep 22:667–689
American Sleep Disorders Association (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:174–184
American Thoracic Society (1995) Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 152:1107–1136
Walters AS (1995) The International Restless Legs Syndrome Study Group. Toward a better definition of the restless legs syndrome. Mov Disord 10:634–642
American Sleep Disorders Association (1993) Recording and scoring leg movements. The Atlas Task Force. Sleep 16(8):748–759
Prado G, Allen R, Trevisani V, Toscano V, Earley C (2002) Sleep disruption in systemic sclerosis (scleroderma) patients: clinical and polysomnographic findings. Sleep Med 2:341–345
Turner GA, Lower EE, Corser BE, Gunther KL, Baughman RP (1997) Sleep apnea in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 14:61–64
McNicholas W, Coffey M, Fitzgerald M (1986) Ventilation and gas exchange during sleep in patients with interstitial lung disease. Thorax 41:777–782
Resta O, Foschino-Barbaro MP, Legari G, et al. (2001) Sleep-related breathing disorders, loud snoring and excessive daytime sleepiness in obese subjects. Int J Obes Relat Metab Disord 25:669–675
Kripke DF, Ancoli-Israel S, Klauber MR, et al. (1997) Prevalence of sleep-disordered breathing in ages 40–64 years: A population-based survey. Sleep 20:65–76
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep disordered breathing. JAMA 284:3015–3021
Dixon JB, Schachter LM, O’Brien PE (2001) Sleep disturbance and obesity: changes following surgically induced weight loss. Arch Intern Med 161:102–106
Ballard RD, Irvin CG, Martin RJ, et al. (1990) Influence of sleep on lung volume in asthmatic patients and normal subjects. J Appl Physiol 68:2034–2041
Hudgel DW, Devadatta P (1984) Decrease in functional residual capacity during sleep in normal humans. J Appl Physiol 57:1319–1322
Aronson RM, Carley DW, Onal E, Wilborn J, Lopata M (1991) Upper airway muscle activity and the thoracic volume dependence of upper airway resistance. J Appl Physiol 70:430–438
Gottlieb DJ, Yao Q, Redline S, Ali T, Mahowald MW (2000) Does snoring predict sleepiness independently of apnea and hypopnea frequency? Am J Respir Crit Care Med 162:1512–1517
Lindberg E, Carter N, Gislason T, Janson T (2001) Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med 164:2031–2035
Guilleminault C, Stoohs R, Clerk A, Cetel M, Maistros P (2005) A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest 127:1–4
Guilleminault C, Chowdhuri S (2000) Upper airway resistance syndrome is a distinct syndrome. Am J Respir Crit Care Med 161:1413–1415
Gold AR, Marcus CL, Dipalo F, Gold MS (2002) Upper airway collapsibility during sleep in upper airway resistance syndrome. Chest 121:1531–1540
American Academy of Sleep Medicine (2005) International classification of sleep disorders: diagnostic and coding manual, 2nd ed. Westchesler, IL: American Academy of Sleep Medicine
Rees K, Kingshott R, Wraith P, Douglas N (2000) Frequency and significance of increased upper airway resistance during sleep. Am J Respir Crit Care Med 162:1210–1214
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mermigkis, C., Chapman, J., Golish, J. et al. Sleep-Related Breathing Disorders in Patients with Idiopathic Pulmonary Fibrosis. Lung 185, 173–178 (2007). https://doi.org/10.1007/s00408-007-9004-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-007-9004-3