Abstract
Attention-deficit/hyperactivity disorder (ADHD) affects approximately 5 % of school-aged children and 2.5 % of adults. Genetic studies in ADHD have pointed to genes in different neurobiological systems, with relatively small individual effects. The mineralocorticoid receptor is the main receptor involved in the initial triggering of stress response. Therefore, its encoding gene (NR3C2) is a candidate for psychiatric disorder studies, including ADHD, and behavioral phenotypes. There is evidence that the Val allele of the MRI180V polymorphism (rs5522) increases the risk of depression, attention and cognitive deficits. We investigated the possible role of the mineralocorticoid receptor gene in the symptom dimensions and susceptibility to persistent ADHD. We compared genotype and allele frequencies in 478 adult patients with ADHD and 597 controls and symptom dimensions in 449 patients and 132 controls. Diagnoses were based on the DSM-IV criteria. ADHD symptom dimensions were investigated with SNAP-IV for ADHD severity and Barkley scales for severity and impairment. Carriers of the Val allele presented higher inattention, hyperactivity/impulsivity and impairment scores, while genotype and allele frequencies did not differ between patients and controls. These results are consistent with a possible link between genetic variations in the HPA axis and inattention and hyperactivity measures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main symptoms of attention-deficit hyperactivity disorder (ADHD) are inattention, impulsivity and hyperactivity. Its prevalence was estimated at approximately 5 % of school-aged children [1–3], persisting in 2.5 % of adults [4]. Meta-analyses of candidate gene investigations have suggested that a few frequently studied genes, mainly from neurotransmitter systems, present small but significant effects [5]. On the other hand, genome-wide association studies (GWAS) in ADHD have suggested the potential involvement of other genes related to basic cellular processes like cell division, adhesion, neuronal migration and neuronal plasticity [6].
There is evidence that neurotrophins, in concert to hypothalamic–pituitary–adrenal (HPA) axis, play a key role in modulating brain plasticity and behavioral coping, especially during ontogenetic critical periods, when the developing brain is particularly sensitive to external stimulations [7]. Stress-induced alterations in the fetal environment can modify brain development, predisposing individuals to develop psychopathologies in childhood, adolescence or even at adulthood, such as attentional and cognitive deficits, anxiety, disturbed social behavior, vulnerability to alcohol and drug consumption, sleep disturbance, schizophrenia and depressive symptoms [8–12].
The relationships between ADHD, cortisol levels and cortisol reactivity are far from clear. Some studies have reported reduced cortisol reactivity in patients with ADHD [13, 14]. Others, however, have found this effect only in ADHD patients with high rates of aggression [15] or did not detect any change in cortisol response [16]. Additionally, it was suggested that ADHD patients may differ in cortisol reactivity according to the ADHD subtype [17]. There is some evidence that the relationship between cortisol levels and disruptive and attention problems may also be modulated by the origin of the sample [14, 18, 19]. For example, these traits might be associated with lower cortisol levels in severe clinical samples [14, 18, 19] or slightly higher levels in a general population sample [20].
The mineralocorticoid receptor (MR) is involved in the onset of stress response [21]. MR is present in the kidney cells, where it is aldosterone selective and controls the salt homeostasis [22], and also in the brain, especially in the hippocampus, where it regulates the basal activity of the HPA and sets the activation threshold of stress responsiveness [21, 23]. Although MR binds cortisol and aldosterone with similar affinity [24, 25], brain MR is mainly exposed to cortisol, which circulates at up to 1000-fold excess compared to aldosterone [23]. MR is involved in anxiety and cognitive function [26]. The blockade of MR by spironolactone (a MR antagonist) in healthy men impairs several aspects of cognition, including selective attention [27].
The MR gene (NR3C2) is located on chromosome 4q31.1, with its coding region being formed by exons 2–9 [28]. Common gene variants, including NR3C2-2G/C (rs2070951) and the MRI180V (rs5522), have been associated with changes in the HPA axis reactivity [29]. There is evidence that MRI180V is involved in the vulnerability for psychiatric disorders [30] and cognitive functions [31]. This SNP is a missense mutation, notably an A-G transition in the second exon of the gene, at codon 180, resulting in an Isoleucine to Valine change [29]. In vitro studies demonstrated that the Val allele implies a loss of function using cortisol as ligand, but not aldosterone [23, 32]. This allele has also been associated with increased endocrine and autonomic responses to acute stress [23], diminished cortisol-induced NR3C2 gene expression [23, 32], geriatric depressive symptoms [30], neuroticism [33] and reward learning deficits [31]. The Val allele has also been shown to be a moderator of parenting and infant attachment security, suggesting that the interaction between genetic and environmental factors may help explain developmental outcomes [34].
In sum, there is evidence that the MRI180V polymorphism may be involved in the modulation of cortisol levels [23], which in turn have a complex association with attention deficits [13–19], cognitive performance [27] and depressive symptoms [30]. Despite the heterogeneity of stress response in ADHD studies, and the central role of the MR in HPA axis function, NR3C2 has not been investigated in an ADHD candidate gene approach yet. This study tests the possible role of MRI180V in ADHD susceptibility and symptom dimensions among adult patients with ADHD and healthy volunteers.
Materials and methods
Sample
The ADHD sample included 478 adult patients that were recruited consecutively in the ADHD outpatient Program of the Hospital de Clínicas de Porto Alegre (HCPA). The mean age of the ADHD sample was 34 years (±11.2). The inclusion criteria were as follows: (a) native Brazilians of European descent (b) age 18 years or older and (c) fulfillment of DSM-IV diagnostic criteria for ADHD [35], both currently and during childhood. The exclusion criteria were as follows: (a) evidence of clinically significant neurologic diseases that might affect cognition (e.g., delirium, dementia, epilepsy, head trauma and multiple sclerosis), (b) current or past history of psychosis and (c) intelligence quotient (IQ) ≤70 [36]. Data on symptom dimensions were available for 449 patients.
The control sample was composed of blood donors (n = 597 for genotype frequencies; n = 132 for symptom dimensions). Volunteers were recruited in the same hospital where patients were ascertained. The inclusion criteria were being both native Brazilians of European descent and 18 years of age or older. The control sample was matched to the ADHD patients on age, sex, years of formal schooling and socioeconomic status (Table 1). The exclusion criteria for controls were the same used for the patients (as mentioned above) added to the fulfillment of DSM-IV ADHD diagnosis [35].
In order to deal with a putative cultural bias toward claiming European ancestry, we used morphological classification based on skin color and morphological traits combined with self-classification for ethnicity. That is, cases and controls were included in the study if, in addition to morphological characteristics of European ancestry, they informed to have grandparents of European origin. The population from Southern Brazil, where this study was performed, is mainly of European descent [37], and no significant population structure was found in the European-derived population of Rio Grande do Sul [38]. The interethnic admixture estimates show that individuals from Southern Brazil present a predominantly European ancestry (94 %) [39], making population stratification unlikely to occur in this situation [40]. The MRI180V Val allele frequency in our control sample (12.1 %) was similar to those reported in other European-derived control groups, varying from 12 % [23] to 14 % [30].
All subjects (patients and controls) signed an informed consent form approved by the Ethics Committee of the HCPA.
Diagnostic procedures
The presence of ADHD and comorbid diagnoses were evaluated through the following semi-structured interviews: (a) K-SADS-E (Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version), adapted to adults, for ADHD and oppositional defiant disorder (ODD) [41, 42]; (b) SCID-IV-R (Structured Clinical Interview for DSM-IV) for the Axis I psychiatric comorbidities [43] and (c) M.I.N.I (Mini-international Psychiatric Interview) for the diagnoses of conduct and antisocial personality disorder [44]. The estimated IQ scores were obtained from the vocabulary and block design subtests of the Wechsler Adult Intelligence Scale-Revised (WAIS-R) [45] administrated by a trained psychologist.
The Portuguese version of the Swanson, Nolan and Pelham Rating Scale-version IV (SNAP-IV) addressed the severity of current ADHD and ODD symptoms [46]. Barkley’s scales were used to evaluate both DSM-IV ADHD symptoms (Barkley severity scores) and impairment (how often their symptoms interfere in 10 areas of life activities—Barkley problem areas). They are all self-report forms that include current (last 6 months) and childhood evaluations [47]. A more detailed description of the ascertainment methods and psychiatric profile of the ADHD sample is described elsewhere [48–51].
Laboratory methods
DNA was extracted from peripheral blood with the salting out procedure [52] and standardized (1:10). The SNP rs5522 in the NR3C2 gene was genotyped applying the TaqMan technology on an ABI7500 system (Applied Biosystems, Foster City, CA, USA) with the following assay-ID: C_12007869_20. The standard PCR was carried out using TaqMan Genotyping PCR Master Mix reagent kit according to the manufacturer’s instructions. Reference sequences and SNP rs-number were obtained from the National Center for Biotechnology Information (NCBI) database (http://www.ncbi.nlm.nih.gov/).
Ten percent of the total sample was randomly re-genotyped by a different researcher. The overall genotyping successful rate (considering genotyping and re-genotyping) was 99.1 %, and the reproducibility accuracy was 98.2 %. For those samples with divergence between first and second genotypes, a third round of genotyping was carried out by a third researcher in order to assure data confidence and the correct genotype was assumed as that with two coincidences.
Statistical analysis
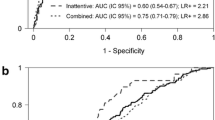
Genotype and allele frequencies were compared between cases and controls by Pearson chi-square tests. ADHD symptom and impairment dimensions (SNAP and Barkley scores) were analyzed by ANCOVA, comparing carriers and non-carriers of the Val allele. Val carriers (homozygous and heterozygous) were grouped due to the small frequency of Val/Val homozygotes (~1 %).
The dimensional analysis was performed using the entire sample (cases and controls), adjusting for the ADHD diagnosis, which was always included as a covariate (except for Barkley severity scores, which were available only for patients). This approach was chosen because the direction of the association is the same in cases and controls, consistently with a possible dimensional nature of the effect of MRI180V SNP. The direction of the findings was also checked in an analysis restricted to patients with ADHD. Sex, age, IQ, socioeconomic status, educational level and frequent comorbidities (major depressive disorder, bipolar disorder, generalized anxiety disorder, obsessive–compulsive disorder, antisocial personality disorder, nicotine dependence, alcohol dependence and drug dependence) were considered for inclusion as covariates. Since none of these variables were associated with both the MRI180V and severity scores with P < 0.20, they were not included in the final analyses. In addition, none of these variables was associated with MRI180V with P < 0.05.
Results
Genotype and allele frequencies of the MRI180V polymorphism in ADHD patients and controls are presented in Table 2. In both samples, the MRI180V polymorphism is in Hardy–Weinberg equilibrium (patients: χ² = 0.13; P = 0.934; control subjects: χ² = 0.06; P = 0.969). Patients and controls did not differ in allele (χ² = 2.46; P = 0.117) and genotype frequencies, using different genetic models (Ile/Ile × Ile/Val × Val/Val: χ² = 2.71, P = 0.258; Ile/Ile + Ile/Val × Val/Val: χ² = 0.24, P = 0.625; Val/Val + Ile/Val × Ile/Ile: χ² = 2.27, P = 0.132).
SNAP severity scores and Barkley problem areas were analyzed as dimensional variables (Table 3). Both cases and controls were included, using ADHD diagnosis as a covariate (the footnote of Table 3 presents results restricted to the ADHD sample). The results for Barkley severity scores were based only on the ADHD sample, since this data are not available for controls.
Carriers of the Val allele of the MRI180V polymorphism presented higher SNAP scores of inattention (P = 0.045), hyperactivity/impulsivity (P = 0.010) and the total sum of symptoms (P = 0.014), but the presence of this allele was not associated with ODD scores (P = 0.304).
The analysis of self-reported Barkley scores in the last 6 months did not reveal differences between carriers and non-carriers of the Val allele for inattention, but carriers presented higher scores in hyperactivity (P = 0.045) and a trend in the total scores (P = 0.063). The analysis on childhood symptoms showed that carriers of the Val allele presented higher scores for inattention (P = 0.011), hyperactivity (P = 0.002) and total scores (P = 0.001). Carriers of the Val allele presented more impairment according to the Barkley problem areas scales, both in childhood (P = 0.011) and in the last 6 months (P = 0.012).
Discussion
Carriers of the Val allele of the MRI180V polymorphism presented higher inattention and hyperactivity/impulsivity scores and higher impairment, with findings coming from two different assessment instruments. The direction of the association was the same among patients with ADHD and healthy volunteers.
Although there are a very small number of previous genetic association studies considering the NR3C2 gene, some patterns start to emerge. An interesting point is that the Val allele has consistently been reported as the risk allele. That is, some phenotypes that include putative maladaptive behavioral symptoms [30, 31] have been suggested to be associated with the Val allele. Interestingly, these findings are in agreement with those obtained with the spironolactone blockade of MR, which impairs several aspects of cognition, including selective attention [27]. Several phenotypes related to the Val allele are also related to ADHD dimensions. These include smoking behavior [53], depression [54] and emotional instability [55, 56], which are associated with inattention and hyperactivity.
In the present study, we found associations between the presence of the Val allele and higher inattention, hyperactivity/impulsivity and impairment scores, which might indicate that Val carriers are predisposed to a variety of psychopathological symptoms whose exact nature remains to be clarified. Taken together, there are potential interrelationships between the Val allele, inattention and hyperactivity symptoms and other psychiatric phenotypes. Future research should address how the physiologic consequences of Val allele relate to these behavioral phenotypes. We should have in mind that multiple genes are regulated by the MR as a transcription factor, with putative pleiotropic consequences [57].
Previous GWAS findings in ADHD have not detected a signal in the NR3C2 region [6, 58]. A meta-analysis of GWAS in ADHD children [58] found no association between MRI180V and ADHD (P = 0.308). Consistent with these previous studies, we found no association between MRI180V and ADHD. However, GWAS for IQ scores [59] and tobacco use [60] detected signals in the NR3C2 gene. Considering the small effect sizes and heterogeneity effects detected in meta-analyses for ADHD-related genes [5], it is plausible that some findings may appear only in a dimensional analysis. This is especially true for ADHD, where the nature of the disorder is indeed dimensional [61–63].
Some limitations have to be considered in the interpretation of these findings. The modulation of the HPA axis and stress response is influenced by many genetic and environmental factors [64, 65]. For example, the cortisol level is also influenced by other polymorphisms in the mineralocorticoid and glucocorticoid receptor genes [29, 66]. MRI180V is a functional SNP [23, 32] and is the most frequently studied polymorphism in NR3C2. However, a more detailed analysis of this gene, including other polymorphisms and haplotype structure could potentially provide additional information. In the CEU population of HapMap database, the MRI180V is in strong linkage disequilibrium with several others SNPs forming a haplotype block into the NR3C2 gene. There are evidences that the MRI180V is in strong linkage disequilibrium with the downstream rs5525 SNP, also in exon 2, and with the functional upstream -2 G/C SNP (rs2070951) [28], which affects transactivation in vitro [67]. Another limitation is the fact that we did not perform an evaluation of cortisol levels in our sample. Future studies might explore the relationships between genetic polymorphisms, physiologic response and dimensional or categorical definitions of ADHD. These studies might be designed for an in-depth analysis of stress response factors in ADHD. Statistical power is certainly an issue in this study, as usual in this field, considering either disorders or dimensional approaches [68]. Even considering the highest OR for a gene with significant association in a meta-analysis with ADHD in children—OR of 1.33 for the Exon 3 VNTR of DRD4 [5], our sample size would still allow for a power of approximately 50 %. Indeed, our sample size would allow for a power of 80 % only with an OR of 1.48. However, it is more difficult to predict the statistical power for a dimensional analysis as the one that we performed. Lack of statistical power might explain, for example, the lack of association between MRI180V SNP and SNAP ODD and Barkley inattention scores in the last 6 months. We think that a cautious interpretation is the best approach, and this data should be used in future meta-analytic studies aiming to evaluate the relationships between HPA-related genes and ADHD.
In conclusion, there is increasing evidence of the implications of stress response variations in mental disorders. Our findings support the consideration of stress response genes, especially NR3C2, as candidate gene in future genetic studies of attention symptoms and disorders.
References
Faraone SV, Biederman J, Mick E (2006) The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med 36:159–165
Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, De Girolamo G, Haro JM, Karam EG, Lara C, Lépine JP, Ormel J, Posada-Villa J, Zaslavsky AM, Jin R (2007) Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 190:402–409
Polanczyk G, Lima MS, Horta BL, Biederman J, Rohde LA (2007) The Worldwide Prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164:942–948
Simon V, Czobor P, Bálint S, Mészáros A, Bitter I (2009) Prevalence and correlates of adult attention deficit/hyperactivity disorder: meta-analysis. Br J Psychiatry 194:204–211
Gizer IR, Ficks C, Waldman ID (2009) Candidate gene studies of ADHD: a meta-analytic review. Hum Genet 126:51–90
Franke B, Neale BM, Faraone SV (2009) Genome-wide association studies in ADHD. Hum Genet 126:13–50
Alleva E, Francia N (2009) Psychiatric vulnerability: suggestions from animal models and role of neurotrophins. Neurosci Biobehav Rev 33:525–536
Maccari S, Darnaudery M, Morley-Fletcher S, Zuena AR, Cinque C, Van Reeth O (2003) Prenatal stress and long-term consequences: implications of glucocorticoid hormones. Neurosci Biobehav Rev 27:119–127
Meier A (1985) Child psychiatric sequelae of maternal war stress. Acta Psychiatr Scand 72:505–511
Schell LM (1981) Environmental noise and human prenatal growth. Am J Physiol Anthropol 56:63–70
Weinstock M (1997) Does prenatal stress impair coping and regulation of hypothalamic–pituitary–adrenal axis? Neurosci Biobehav Rev 21:1–10
Weinstock M (2005) The potential influence of maternal stress hormones on development and mental health of the offspring. Brain Behav Immun 19:296–308
King JA, Barkley RA, Barrett S (1998) Attention-deficit hyperactivity disorder and the stress response. Biol Psychiatry 44:72–74
Hong HJ, Shin DW, Lee EH, Oh YH, Noh KS (2003) Hypothalamic-pituitary-adrenal reactivity in boys with attention deficit hyperactivity disorder. Yonsei Med J 44:608–614
Yang SJ, Shin DW, Noh KS, Stein MA (2007) Cortisol is inversely correlated with aggression for those boys with attention deficit hyperactivity disorder who retain their reactivity to stress. Psychiatry Res 153:55–60
Lackschewitz H, Huther G, Kroner-Herwig B (2008) Physiological and psychological stress responses in adults with attention-deficit/hyperactivity disorder (ADHD). Psychoneuroendocrinology 33:612–624
van West D, Claes S, Deboutte D (2009) Differences in hypothalamic-pituitary-adrenal axis functioning among children with ADHD predominantly inattentive and combined types. Eur Child Adolesc Psychiatry 9:543–553
Kariyawasam SH, Zaw F, Handley SL (2002) Reduced salivary cortisol in children with comorbid Attention deficit hyperactivity disorder and oppositional defiant disorder. Neuro Endocrinol Lett 1:45–48
Ma L, Chen YH, Chen H, Liu YY, Wang YX (2011) The function of hypothalamus-pituitary-adrenal axis in children with ADHD. Brain Res 1368:159–162
Sondeijker FE, Ferdinand RF, Oldehinkel AJ, Veenstra R, Tiemeier H, Ormel J, Verhulst FC (2007) Disruptive behaviors and HPA-axis activity in young adolescent boys and girls from the general population. J Psychiatr Res 41:570–578
de Kloet ER, Vreugdenhil E, Oitzl MS, Joëls M (1998) Brain corticosteroid receptor balance in health and disease. Endocr Rev 19:269–301
de Kloet ER, Van Acker SA, Sibug RM, Oitzl MS, Meijer OC, Rahmouni K, de Jong W (2000) Brain mineralocorticoid receptors and centrally regulated functions. Kidney Int 57:1329–1336
de Rijk RH, Wust S, Meijer OC, Zennaro MC, Federenko IS, Hellhammer DH, Giacchetti G, Vreugdenhil E, Zitman FG, de Kloet ER (2006) A common polymorphism in the mineralocorticoid receptor modulates stress responsiveness. J Clin Endocrinol Metab 91:5083–5089
Reul JM, de Kloet ER (1985) Two receptor systems for corticosterone in rat brain: microdistribution and differential occupation. Endocrinology 117:2505–2511
Funder JW (2004) Aldosterone, mineralocorticoid receptors and vascular inflammation. Mol Cell Endocrinol 217:263–269
de Kloet ER (2003) Hormones, brain and stress. Endocr Regul 37:51–68
Otte C, Moritz S, Yassouridis A, Koop M, Madrischewski AM, Wiedemann K, Kellner M (2007) Blockade of the mineralocorticoid receptor in healthy men: effects on experimentally induced panic symptoms, stress hormones, and cognition. Neuropsychopharmacology 32:232–238
de Rijk RH, van Leeuwen N, Klok MD, Zitman FG (2008) Corticosteroid receptor-gene variants: modulators of the stress-response and implications for mental health. Eur J Pharmacol 585:492–501
de Rijk RH (2009) Single nucleotide polymorphisms related to HPA axis reactivity. NeuroImmunoModulation 16:340–352
Kuningas M, de Rijk RH, Westendorp RG, Jolles J, Slagboom PE, van Heemst D (2007) Mental performance in old age dependent on cortisol and genetic variance in the mineralocorticoid and glucocorticoid receptors. Neuropsychopharmacology 32:1295–1301
Bogdan R, Perlis RH, Fagerness J, Pizzagalli DA (2010) The impact of mineralocorticoid receptor ISO/VAL genotype (rs5522) and stress on reward learning. Genes Brain Behav 9:658–667
Arai K, Nakagomi Y, Iketani M, Shimura Y, Amemiya S, Ohyama K, Shibasaki T (2003) Functional polymorphisms in the mineralocorticoid receptor and amirolide-sensitive sodium channel genes in a patient with sporadic pseudohypoaldosteronism. Hum Genet 112:91–97
de Rijk RH, de Kloet ER, Zitman FG, van Leeuwen N (2011) Mineralocorticoid receptor gene variants as determinants of HPA axis regulation and behavior. Endocr Dev 20:137–148
Luijk MP, Tharner A, Bakermans-Kranenburg MJ, van Ijzendoorn MH, Jaddoe VW, Hofman A, Verhulst FC, Tiemeier H (2011) The association between parenting and attachment security is moderated by a polymorphism in the mineralocorticoid receptor gene: evidence for differential susceptibility. Biol Psychol 88:37–40
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Press, Washington, DC
Kaplan E, Fein D, Morris R, Delis DC (1991) WAIS-R: manual. Psychological corporation, San Antonio
Salzano FM, Bortolini MC (2002) The evolution and genetics of Latin American populations. Cambridge University Press, Cambridge
Zembrzuski VM, Callegari-Jacques SM, Hutz MH (2006) Application of an African Ancestry Index as a genomic control approach in a Brazilian population. Ann Hum Genet 70:822–828
Santos NP, Ribeiro-Rodrigues EM, Ribeiro-Dos-Santos AK, Pereira R, Gusmão L, Amorim A, Guerreiro JF, Zago MA, Matte C, Hutz MH, Santos SE (2010) Assessing individual interethnic admixture and population substructure using a 48-insertion-deletion (insel) ancestry-informative marker (aim) panel. Hum Mutat 31:184–190
Hutchison KE, Stallings M, McGeary J, Bryan A (2004) Population stratification in the candidate gene study: fatal threat or red herring? Psychol Bull 130:66–79
Mercadante MT, Asbahar F, Rosário MC, Ayres AM, Karman L, Ferrari MC, Assumpcão FB, Miguel EC (1995) K-SADS, entrevista semi-estruturada para diagnóstico em psiquiatria da infância, versão epidemiológica. FMUSP, São Paulo
Grevet EH, Bau CH (2005) Interrater reliability for diagnosis in adults of attention deficit hyperactivity disorder and oppositional defiant disorder using K-SADS-E. Arq Neuropsiquiatr 63:307–310
First MB, Spitzer RL, Gibbon M, Williams JB (1998) Structured clinical interview for DSMIV (SCID-I). Biomedics Research Department, New York
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–33; quiz 34–57
Wechsler D (1981) WAIS-R—Manual for the Wechsler Adult Intelligence Scale—Revised. The Psychological Corporation, San Antonio
Swanson JM (1992) School-based assessments and interventions for ADD students. KC Publishing, Irvine
Barkley RA, Murphy KR (1998) Attention deficit hyperactivity disorder: a clinical workbook, vol 2. The Guilford Press, New York
Grevet EH, Bau CH, Salgado CA, Ficher A, Kalil K, Victor MM, Garcia C, Sousa NO, Belmonte-de-Abreu P (2006) Lack of gender effects on subtype outcomes in adults with attention-deficit/hyperactivity disorder: support for the validity of subtypes. Eur Arch Psychiatry Clin Neurosci 256:311–319
Fischer AG, Bau CH, Grevet EH, Salgado CA, Victor MM, Kalil KL, Sousa NO, Garcia CR, Belmonte-de-Abreu P (2007) The role of comorbid major depressive disorder in the clinical presentation of adult ADHD. J Psychiatr Res 41:991–996
Contini V, Victor MM, Cerqueira CC, Polina ER, Grevet EH, Salgado CA, Karam RG, Vitola ES, Belmonte-de-Abreu P, Bau CH (2011) Adrenergic α2A receptor gene is not associated with methylphenidate response in adults with ADHD. Eur Arch Psychiatry Clin Neurosci 261:205–211
Karam RG, Bau CH, Salgado CA, Kalil KL, Victor MM, Sousa NO, Vitola ES, Picon FA, Zeni GD, Rohde LA, Belmonte-de-Abreu P, Grevet EH (2009) Late-onset ADHD in adults: milder, but still dysfunctional. J Psychiatr Res 43:697–701
Lahiri DK, Nurnberger JI Jr (1991) A rapid non-enzymatic method for the preparation of HMW DNA from blood for RFLP studies. Nucleic Acids Res 19:5444
Sousa NO, Grevet EH, Salgado CA, Silva KL, Victor MM, Karam RG, Vitola ES, Picon FA, Zeni GD, Rohde LA, Belmonte-de-Abreu P, Bau CH (2011) Smoking and ADHD: an evaluation of self medication and behavioral disinhibition models based on comorbidity and personality patterns. J Psychiatr Res 6:829–834
Cole J, Ball HA, Martin NC, Scourfield J, McGuffin P (2009) Genetic overlap between measures of hyperactivity/inattention and mood in children and adolescents. J Am Acad Child Adolesc Psychiatry 11:1094–1101
Blase SL, Gilbert AN, Anastopoulos AD, Costello EJ, Hoyle RH, Swartzwelder HS, Rabiner DL (2009) Self-reported ADHD and adjustment in college: cross-sectional and longitudinal findings. J Attend Disord 3:297–309
Purper-Ouakil D, Franc N (2011) Emotional dysfunctions in attention deficit hyperactivity disorder. Arch Pediatr 6:679–685
Le Menuet D, Viengchareun S, Muffat-Joly M, Zennaro MC, Lombès M (2004) Expression and function of the human mineralocorticoid receptor: lessons from transgenic mouse models. Mol Cell Endocrinol 217:127–136
Neale BM, Medland SE, Ripke S, Asherson P, Franke B, Lesch KP, Faraone SV, Nguyen TT, Schäfer H, Holmans P, Daly M, Steinhausen HC, Freitag C, Reif A, Renner TJ, Romanos M, Romanos J, Walitza S, Warnke A, Meyer J, Palmason H, Buitelaar J, Vasquez AA, Lambregts-Rommelse N, Gill M, Anney RJ, Langely K, O’Donovan M, Williams N, Owen M, Thapar A, Kent L, Sergeant J, Roeyers H, Mick E, Biederman J, Doyle A, Smalley S, Loo S, Hakonarson H, Elia J, Todorov A, Miranda A, Mulas F, Ebstein RP, Rothenberger A, Banaschewski T, Oades RD, Sonuga-Barke E, McGough J, Nisenbaum L, Middleton F, Hu X, Nelson S; Psychiatric GWAS Consortium: ADHD Subgroup (2010) Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 49:884–897
Pan Y, Wang KS, Aragam N (2011) Ntm and nr3c2 polymorphisms influencing intelligence: Family-based association studies. Prog Neuropsychopharmacol Biol Psychiatry 35:154–160
Berrettini W, Yuan X, Tozzi F, Song K, Francks C, Chilcoat H, Waterworth D, Muglia P, Mooser V (2008) Alpha-5/alpha-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol Psychiatry 13:368–373
Shaw P, Gilliam M, Liverpool M, Weddle C, Malek M, Sharp W, Greenstein D, Evans A, Rapoport J, Giedd J (2011) Cortical development in typically developing children with symptoms of hyperactivity and impulsivity: support for a dimensional view of attention deficit hyperactivity disorder. Am J Psychiatry 168:143–151
Lubke GH, Hudziak JJ, Derks EM, van Bijsterveldt TC, Boomsma DI (2009) Maternal ratings of attention problems in ADHD: evidence for the existence of a continuum. J Am Acad Child Adolesc Psychiatry 48:1085–1093
Polderman TJ, Derks EM, Hudziak JJ, Verhulst FC, Posthuma D, Boomsma DI (2007) Across the continuum of attention skills: a twin study of the SWAN ADHD rating scale. J Child Psychol Psychiatry 48:1080–1087
El Hage W, Powell JF, Surguladze SA (2009) Vulnerability to depression: what is the role of stress genes in gene x environment interaction? Psychol Med 39:1407–1411
Gillespie CF, Phifer J, Bradley B, Ressler KJ (2009) Risk and resilience: genetic and environmental influences on development of the stress response. Depress Anxiety 26:984–992
van Leeuwen N, Bellingrath S, de Kloet ER, Zitman FG, DeRijk RH, Kudielka BM, Wüst S (2011) Human mineralocorticoid receptor (MR) gene haplotypes modulate MR expression and transactivation: implication for the stress response. Psychoneuroendocrinology 5:699–709
van Leeuwen N, Kumsta R, Entringer S, de Kloet ER, Zitman FG, DeRijk RH, Wüst S (2010) Functional mineralocorticoid receptor (MR) gene variation influences the cortisol awakening response after dexamethasone. Psychoneuroendocrinology 35:339–349
Kebir O, Joober R (2011) Neuropsychological endophenotypes in attention-deficit/hyperactivity disorder: a review of genetic association studies. Eur Arch Psychiatry Clin Neurosci 261:583–594
Acknowledgments
We thank the following Brazilian funding agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Conselho de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação de Amparo a Pesquisa do Rio Grande do Sul (FAPERGS-DECIT/PPSUS) and Programa de Apoio a Núcleos de Excelência (PRONEX). Our thanks are also due to Stephen Faraone and Benjamin Neale for information and data on GWAS studies in ADHD.
Conflict of interest
Dr Rohde was on the speaker’s bureau and/or acted as consultant for Eli-Lilly, Janssen-Cilag and Novartis in the last 3 years. Currently, his only industry-related activity is taking part in the advisory board/speaker’s bureau for Eli-Lilly and Novartis (less than U$ 10,000 per year and reflecting less than 5 % of his gross income per year). The ADHD Program chaired by him received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Abbott, Bristol-Myers Squibb, Eli-Lilly, Janssen-Cilag and Novartis. Dr Belmonte-de-Abreu is on the speaker’s bureau or is a consultant for Janssen-Cilag and Bristol-Myers Squibb. Dr Grevet is on the speaker’s bureau or is a consultant for Novartis, Janssen-Cilag and Shire.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kortmann, G.L., Contini, V., Bertuzzi, G.P. et al. The role of a mineralocorticoid receptor gene functional polymorphism in the symptom dimensions of persistent ADHD. Eur Arch Psychiatry Clin Neurosci 263, 181–188 (2013). https://doi.org/10.1007/s00406-012-0321-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-012-0321-z