Abstract
The mini-mental state examination (MMSE) has been widely used as a screening instrument for cognitive disorders. Age, schooling and many other sociodemographic and health variables may be associated with a worse performance on the MMSE. The objectives of this study were to investigate the distribution of MMSE percentiles in a large Brazilian community-based elderly sample, divided according to age and schooling, and to evaluate the impact of sociodemographic and health variables on groups of elderly people with lower cognitive performance. The MMSE was applied to a sample of 2,708 adults, aged 60 years and older. Of this population, 1,563 individuals were living in the city of São Paulo, while 1,145 were living in the city of Ribeirão Preto. The subjects were divided into six groups according to the amount of schooling that they had received (no formal education, 1–4 and ≥5 years) and age (<75 and ≥75 years old). To each one of the subgroups a stepwise logistic regression was applied, considering the following dependent variable: subjects who scored under or above the 15th percentile on MMSE. High scores on a depression scale, high scores on a memory complaints scale and low socio-economic levels were associated with poorer performance on the MMSE. Being currently employed and being married were related to higher scores on the test. Many sociodemographic and health variables can influence MMSE performance, with impacts depending on age and schooling. Clinicians and primary care physicians should pay attention to variables that may be associated with worse cognitive performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ageing process in Latin America has had significant effects on the elderly population, which experience a sustained decrease in real income, decreased access to health services and insufficient public resources for retirement, compared to other countries [41].
In Brazil, ageing is taking place at a more accelerated pace than in developed countries, very quickly modifying the Brazilian population’s age structure [30]. Because of this, Brazilian health authorities will face new challenges, such as an increasing number of persons with cognitive disorders [14]. A very similar situation will likely be seen in other developing countries in the next few years, requiring a more active approach for detecting dementia, as stated by Lopponen et al. [38].
Since its introduction in 1975, the mini-mental state examination (MMSE) [23, 24] has been used widely as a screening instrument to assess cognitive disorders and dementia. It is a brief, standardised method to determine a patient’s cognitive function that assesses orientation, attention, immediate and short-term recall, language and the ability to follow simple verbal and written commands [21]. It has been used as a brief cognitive test [7] in clinical practice and research, as well as in epidemiological studies [7, 9]. The MMSE has been translated into several languages and has been used successfully in many independent cross-national epidemiological studies of dementia [10, 11].
Age and schooling influence subjects’ performance on the MMSE [4, 7, 9, 11, 21, 31, 32, 34, 35, 39, 46], as do many other sociodemographic characteristics (e.g., social class, occupation, gender) and health variables [2, 4, 31, 39, 44, 46].
Various strategies have been proposed as an attempt to minimise the effects of these sociodemographic factors, especially age and level of schooling, on the interpretation of the MMSE results. One of the most common approaches is the adjustment of cut-off points according to level of schooling [11, 13, 34]. However, there is no consensus to date regarding which cut-off points are the best for determining the presence of cognitive disorders in community-based studies or even in clinical samples [15]. Some authors who have recommended a different strategy for the investigation of population samples have suggested the use of the MMSE score percentiles [15, 43]. In some of these studies, the prevalence of community-dwelling elderly people with significant cognitive disorders was close to 15% [12, 28, 35], suggesting that scores below the 15% MMSE percentile can be applied to maximise screening accuracy.
However, although some studies in developed countries [4, 21] and even recent studies in Brazil [34, 43, 46] have investigated the performance of the MMSE in large community-based samples, additional evaluations are needed to address the influence of sociodemographic and health variables on the MMSE performance, particularly in community samples from developing countries.
The aims of this study were to investigate the distribution of MMSE percentiles in a large Brazilian community-based elderly sample, divided according to age and schooling, and to evaluate the impact of sociodemographic and health variables on groups of elderly people with lower cognitive performance who are, therefore, at risk of being cognitively impaired or demented.
Methods
Sample
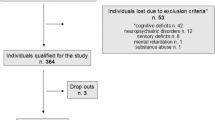
A cluster random sampling of a population of individuals aged 60 years old and over from three different socioeconomic classes (upper, middle and lower) was applied. This strategy aimed to evaluate a sample containing cities’ districts that were representative of the elderly living in São Paulo [29] and in Ribeirão Preto [37], two cities in São Paulo state, which is located in the Southeast region of Brazil. Both cities’ districts were ranked from the wealthiest to the poorest according to data from the 2000 Census, provided by the Brazilian Institute of Geography and Statistics (IBGE; [30]). The following parameters were applied to classify the districts: income, schooling, proportion of elderly living in each district and sanitation. Afterwards, in both cities, the districts were divided into three groups, and one district representative of each socioeconomic stratum was chosen to represent the upper, middle and lower groups. In each of the three districts, census sectors were selected with a probability proportional to each cluster size. Blocks of 10 domiciles were randomly chosen in each of the selected census sectors. Following local media (newspaper, radio, television) and mail advertisements, a trained team started a systematic door knocking survey in order to find elderly subjects. After the identification, a community sample of 2,233 subjects older than 60 years was approached in São Paulo city, and a total of 1,563 subjects who agreed to be visited by a trained interviewer (response rate = 70%) were assessed. In the city of Ribeirão Preto, a sample of 1,784 subjects was approached, of which 1,145 agreed to participate (response rate = 64.2%). The interviewers tried at least three times to evaluate the elderly subjects at home before they were considered to be refusals. A Brazilian version of the MMSE was applied to a community sample of 2,708 subjects: 1,563 individuals from São Paulo city [29] and 1,145 from Ribeirão Preto [37].
Instruments
The MMSE version utilised was a Brazilian version that was included in the Cambridge Examination for Mental Disorders of the Elderly (CAMDEX) [8]. The interviewers were trained before administering the MMSE to the sample. Both the serial seven and spelling “world” backwards items were applied; however, only the highest value of each of them was considered in the total MMSE score.
The following instruments were also administered: a sociodemographic questionnaire (including occupation); a clinical inventory; an inventory of previous personal history and habits; and, using the questionnaire of the Brazilian Association of Market Research (ABIPEME) [1], a socioeconomic classification scale that allowed for 5 levels of classification (from A, the highest, to E, the lowest). This scale classifies the families based on schooling and in the owning of consumption goods, such as household appliances. A nine-item scale (scores from 0 to 9) was administered to evaluate cognitive and/or memory complaints. Five of the items were based on questions from the CAMDEX interview [8] (e.g. has presented memory problems lately, has forgotten where stored objects, has forgotten the name of well-known persons) and four additional items (e.g. has difficulties to remember recent facts, has difficulties to remember appointments) were assigned through a consensus of the study team composed of psychiatrists and neurologists with clinical experience caring for Brazilian elderly patients. The scale showed internal consistency measured by a Cronbach alpha of 0.778 in the community sample. A ten-item instrument (D-10), which is being developed by our research group, was administered for the evaluation of depressive symptoms (escores from 0 to 10) in the elderly [6]. This instrument is similar to the GDS-5 (geriatric depression scale) [48] and D-10 psychometric properties were presented elsewhere [6].
Data (other than the MMSE) were obtained directly from the cognitively intact elderly subjects and/or from an informant, who was usually a close relative, when the subject was cognitively impaired.
Statistical analysis
The sample was divided according to age (below and above 75 years old) and schooling (no formal schooling, 1–4 and ≥5 years of education), classifying the subjects into six groups, to calculate the MMSE percentiles.
The correlation between the MMSE scores, age and schooling was investigated with the Pearson (r) and Spearman (ρ) correlation coefficients, respectively. The Spearman correlation coefficient was applied because the variable schooling did not have a normal distribution. MMSE scores were compared between the two age groups with the Student’s t test and among the three schooling groups with the one-way analysis of variance followed by a Tukey post-hoc comparison. The influence of schooling on MMSE scores, considering the influence of ageing, was addressed with the analysis of covariance.
For each one of these groups a stepwise logistic regression was applied, considering as the dependent variable subjects who scored under or above the 15th percentile on MMSE. The independent variables were the sociodemographic (gender, present occupation, marital status, type of occupation, socioeconomic class) and health variables (depressive symptoms, memory complaints, personal history of stroke, Parkinson’s disease, head trauma, epilepsy, diabetes, hypertension, hypercholesterolemia, acute myocardial infarction, and tumour/cancer).
A stepwise forward adjusted and unadjusted logistic regression based on the Akaike’s information criterion was applied to investigate which variables were relevant for each one of the six groups divided by age and schooling. For all six groups, the interaction between depression symptoms (assessed by the D-10 depression scale) and subjective memory impairment (assessed by a memory complaint scale) was also investigated. The significance level was α = 0.05 for all comparisons. The analyses were run in SPSS 14.0.
Both investigations were approved by the São Paulo and the Ribeirão Preto Universities ethics committees, and all the subjects or their relatives agreed to participate in the study by signing an informed consent form.
Results
The mean age of the whole sample (n = 2,712) was 70.88 ± 7.79 years (range 42), and 66.5% were females. Age groups, gender, education, socioeconomic class, and marital status of the population samples are presented in Table 1.
The mean MMSE scores for the whole sample were 25.0 ± 5.04, for the São Paulo sample 24.76 ± 5.00, and for the Ribeirão Preto sample 25.32 ± 5.08. The MMSE scores were negatively correlated with age (r = −0.33, p < 0.001) and positively correlated with schooling (ρ = 0.52, p < 0.001).
The sample was divided into six groups classified by age and schooling, as can be seen in Table 2. MMSE scores were significantly different between the two age groups (t = 12.42, p < 0.001). MMSE scores were also significantly different among the three schooling groups (F = 651.71, p < 0.001). The difference remained significant after controlling for age (F = 638.16, p < 0.001).
The MMSE percentiles in the sample divided by the two age groups and the three schooling levels are presented in Table 3.
Logistic regression analysis was performed for each of the six groups, and the results are presented in Table 4.
Group A (no formal schooling, <75 years old)
High scores in the depression scale (D-10) were associated with worse performance on the MMSE for individuals without formal schooling under the age of 75 years (OR 1.24, 95% CI: 1.03–1.48).
Group B (1–4 years of schooling, <75 years old)
Socioeconomic class and memory complaints were the relevant variables impacting MMSE scores for individuals under the age of 75 years and with 1–4 years of schooling.
There was a positive interaction between high scores in the memory and depression scales (D-10) and worse performance on the MMSE (OR 1.01, 95% CI: 1.01–1.03).
Lower socioeconomic level was also associated with scores under the 15th percentile in the MMSE as individuals belonging to classes D + E had a higher odds ratio compared to those from classes A + B (OR 2.32, 95% CI: 1.13–4.78). On the other hand, subjects from class C did not differ from subjects classified in class A + B.
Group C (≥5 years of schooling, <75 years old)
Socio-economic levels were related to scores under the 15th MMSE percentile in group C.
Socioeconomic class C (OR 1.75, 95% CI: 1.19–2.60) and D + E (OR 5.24, 95% CI: 2.50–11.02) were significantly associated with a worse performance on the MMSE compared to class A + B.
Group D (no formal schooling, ≥75 years old)
For the group D, higher score on the memory complaint scale was the only variable related to poorer performance on the MMSE (OR 1.40, 95% CI: 1.10–1.80).
Group E (1–4 years of schooling, ≥75 years old)
In individuals from Group E, high scores on the memory complaints scale were associated with MMSE scores under the 15th percentile (OR 1.50, 95% CI: 1.25–1.80).
Group F (≥5 years of schooling, ≥75 years old)
Being currently employed was related to high scores on the MMSE in Group F (OR 0.39, 95% CI: 0.19–0.82).
Being married was associated with a better performance on the test, in comparison to being widowed (OR 0.32, 95% CI: 0.13–0.78). No significant differences were found among single and separated subjects when compared to widowed ones.
For all groups, no significant association between any of the health-related factors (excluding memory complaints and depressive symptoms) and MMSE scores was found.
Discussion
Our study showed a relationship between certain sociodemographic and health variables and worse performance on the MMSE in elderly subjects from a large community-based sample. High scores in the D-10 depression scale, high scores on a memory complaint scale, an interaction between the depression and memory scales, and low socioeconomic level were associated with a poorer performance on the MMSE. On the other hand, better performance on the MMSE was associated with marital status (married) and being currently employed.
The choice of the 15th MMSE percentile as an indication of relevant cognitive dysfunction was based on previous data that have shown that around 60% of MCI and dementia cases can be found when subjects who scored between under 15th or 16th MMSE percentiles were further investigated [23]. In another community-based study, Callahan et al. [12] found a prevalence of cognitive impairment among patients aged 60 years and over of 15.7%.
Brazil is a large country, with extreme socio-cultural differences found among the regions of its territory. Basic education is consequently very heterogeneous and can be associated with differential cognitive performance [46].
As the MMSE scores in the present study were not normally distributed, the assumptions of a normal theory do not apply [21], preventing the analysis of the MMSE scores as a continuous variable. Moreover, we agree with authors who have stated that the most adequate option to study the MMSE performance of a population sample would be to consider the percentile distribution of the test scores [15, 43]. This rational was applied in our research, with the MMSE scores being presented as a percentile distribution, and applying logistic regression to investigate the characteristics of those community-dwelling elderly with ‘possible’ cognitive disorders.
Consistent with previous studies from Brazil [11, 34, 35, 46] and from other countries [2, 4, 7, 9, 31, 39, 47], our results suggest that older age and lower education levels both have a significant effect on MMSE performance, increasing the likelihood of obtaining lower test scores. Higher education levels were associated with better performance on the MMSE, in agreement with previous studies that have suggested the use of higher cut-off scores for more highly educated individuals [40].
Association of socioeconomic level and cognitive performance has already been described [17]. Socioeconomic levels may reflect educational attainments, but they are also related to lifestyle differences in socioeconomic groups that may prove to be important in maintaining cognition [19, 22].
In a study about the impact of sociodemographic variables on the MMSE performance of older Australians, the regression models also showed that older age, educational levels, language spoken at home and in country of birth, socioeconomic status, occupation, sex, and presence of a mood disorder made significant and unique contributions to performance on the MMSE [4]. Language spoken at home was very important for Australian subjects since local natives do not speak English at home [4]. There is no analogous situation in Brazil; however, regarding some of the other variables (socioeconomic status, depressive symptoms) we also found an impact on the MMSE performance in our sample.
The influence of depressive symptoms on the MMSE performance, as was observed in our sample, has already been reported [34]. Depressive symptoms may be an early manifestation of a cognitive disorder [16], and depression itself can be associated with lower cognitive functioning [26].
Anderson et al. [4] described both early and recent intellectual activity as relevant to the MMSE performance, which could explain the higher scores among subjects who were presently employed. Such a measure can be considered as a possible correlate of intellectual activity, but it is also possible that those with cognitive difficulties were more likely to stop working. Fratiglioni et al. [25] reported in a review that socially, mentally and physically active lifestyles were associated with beneficial effects on cognition, suggesting a protective effect of these factors against dementia.
Memory complaints had a very important impact on the present research, since in three of the six groups this variable was associated with worse performance on the MMSE. During the last few years, many authors have discussed the association between memory complaints and the risk of developing dementia [33]. Clarnette et al. [18] showed that those with memory complaints have worse cognitive performance than those without such complaints, suggesting that subjective memory loss may be a reliable indicator of cognitive decline. Consistent with these findings, Crowe et al. [20] found that, for mild cognitive impairment, the one-item complaint of subjective change in memory at baseline predicted future cognitive decline. Despite the present results being consistent with the studies mentioned, there are some authors who have not found an association between memory complaints and mild cognitive impairment or dementia [36, 42].
One of the limitations of the present study was that, as the population samples were selected to represent elderly living in different socioeconomic strata in São Paulo and Ribeirão Preto, they might not be representative of the general elderly population from both cities. Another limitation could be the response rate of 64.2–70%. However, in other community-based studies with elderly individuals performed in Brazil [5], Australia [27], Denmark [3] and Japan [48], the response rates were, respectively, 65.2, 68.6, 64.6, and 75.7%. Therefore, the response rate obtained during the field phase of our study was similar to the rate found in other studies involving elderly individuals in Brazil (and in the city of São Paulo), as well as in developed countries. Finally, the clinical and health variables were assessed exclusively through self-reports by the elderly adults in our sample. However, there are some studies that demonstrate that there is usually enough agreement between data on health variables provided by self-report and proxy information [28, 45]. As dementia was not ruled out from our sample, demented subjects were probably included among those with MMSE scores below the 15th percentile and the characteristics of these subjects could in part justify the results of our study.
Conclusions
Many sociodemographic and health variables can influence general cognitive performance, with different impacts depending on age and schooling. These data may help to detect those patients who are likely to perform worse on the MMSE and are in need of more attention by clinicians or primary care physicians. Looking for memory complaints and depressive symptoms is definitely relevant, especially for those subjects with low educational attainment.
Our results suggest a need for normative measurements of cognitive function in heterogeneous community-based groups in order to distinguish cognitive dysfunction severity from possible measurement bias. The percentile distribution and the attention to specific sociodemographic and health variables, specifically age and schooling, should provide a more reliable interpretation of cognitive dysfunction even among subjects from different socioeconomic and cultural backgrounds. Clinicians should pay attention to the variables that might be associated with a worse general cognitive performance in order to select those individuals that would benefit from an additional cognitive evaluation.
References
ABIPEME—Critério de Classificação Econômica Brasil [ABEP Web site] (2000) Dados com base no Levantamento Sócio Econômico (2000) IBOPE. http://www.abep.org/codigosguias/ABEP_CCEB.pdf
Acevedo A, Loewentein DA, Agrón J, Duara R (2007) Influence of sociodemographic variables on neuropsychological test performance in Spanish-speaking older adults. J Clin Exp Neuropsychol 29(5):530–544
Andersen K, Lolk A, Nielsen H, Andersen J, Olsen C, Kragh-Sorensen P (1997) Prevalence of very mild to severe dementia in Denmark. Acta Neurol Scand 96(2):82–87
Anderson TM, Sachdev PS, Brodaty H, Trollor J, Andrews G (2007) Effects of sociodemographic and health variables on mini-mental state exam scores in older Australians. Am J Geriatr Psychiatry 15(6):467–476
Andrade L, Walters EE, Gentil V, Laurenti R (2002) Prevalence of ICD-10 mental disorders in a catchment area in the city of São Paulo, Brazil. Soc Psychiatry Psychiatr Epidemiol 37:316–325
Barcelos-Ferreira R, Pinto JA Jr, Nakano EY, Steffens DC, Litvoc J, Bottino CM (2009) Clinically significant depressive symptoms and associated factors in a community sample of elderly subjects from Sao Paulo, Brazil. Am J Geriatr Psychiatry 17(7):582–590
Bleeckr ML, Bolla-Wilson K, Kawas C, Agnew J (1988) Age-specific norms for the Mini-Mental State Exam. Neurology 38:1565–1568
Bottino CMC, Almeida OP, Tamai S, OV Forlenza, MZ Scalco, IAM Carvalho (1999) Entrevista estruturada para diagnóstico de transtornos mentais em idosos (CAMDEX) The Cambridge examination for mental disorders of the elderly. Brazilian version (translated and adapted on behalf of the editors, Cambridge University Press), São Paulo
Bravo G, Hebert R (1997) Age and education specific reference values for the mini-mental and modified mini-mental state examinations derived from a non-demented elderly population. Int J Geriatric Psychiatry 12:1008–1018
Brayne C, Calloway P (1990) The case identification of dementia in the community: a comparison of methods. Int J Ger Psychiatry 5:309–316
Brucki SMD, Nitrini R, Caramelli P, Bertolucci PHF, Okamoto IH (2003) Sugestões para o uso do Mini-Exame do Estado Mental no Brasil. Arq Neuropsiquiatr 61(3-B):777–781
Callahan CM, Hendrie HC, Tierney WM (1995) Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann Intern Med 122(6):422–429
Caramelli P, Herrera E Jr, Nitrini R (1999) The Mini-State Examination and the diagnosis of dementia in illiterate elderly. Arq Neuropsiquiatr 57(Suppl 1):S7
Carvalho JAM, Garcia RA (2003) O envelhecimento da população brasileira: um enfoque demográfico. Cad Saúde Pública 19(3):725–733
Castro-Costa E, Fuzikawa C, Uchoa E et al (2008) Norms for the mini-mental state examination adjustment of the cut-off point in population–based studies (evidences from the Bambuí Health Aging Study). Arq Neuropsiquiatr 66(3):524–528
Chen P, Ganguli M, Mulsant BH et al (1999) The temporal relationship between depressive symptoms and dementia. A community based prospective study. Arch Gen Psychiatry 40:922–935
Chin A, O’Connell H, Kirby M, Denihan A (2006) Int J Geriatr Psychiatry 21:1150–1155
Clarnette RM, Almeida OP, Forstl H et al (2001) Clinical characteristics of individuals with subjective memory loss in Western Australia: results from a cross-sectional survey. Int J Geriatr Psychiatry 16:168–174
Coulson I, Strang V, Marino R, Minichiello V (2004) Knowledge and lifestyle behaviours of healthy older adults related to modifying the onset of vascular dementia. Arch Gerontol Geriatr 39:43–58
Crowe M, Andel R, Wadley V et al (2006) Subjective cognitive function and decline among older adults with psychometrically defined amnestic MCI. Int J Geriatr Psychiatry 21:1187–1192
Crum R, Anthony JC, Basset SS, Folstein MF (1993) Population-based norms for the mini-mental state examination by age and educational level. JAMA 269(18):2386–2391
Evans DA, Hebert LE, Beckett LA et al (1997) Education and other measures of socioeconomic status and risk of incident Alzheimer disease in a defined population of older persons. Arch Neurol 54:1399–1405
Folstein M, Anthony JC, Parhad I, Duffy B, Gruenberg EM (1985) The meaning of cognitive impairment in the elderly. J Am Geriatr Soc 33:228–235
Folstein ME, Folstein SE, McHugh PR (1975) “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Fratiglioni L, Paillard-Borg S, Winblad B (2004) An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol 3:343–353
Ganguli M, Du Y, Dodge HH et al (2006) Depressive symptoms and cognitive decline in late life. A prospective epidemiological study. Arch Gen Psychiatry 63:153–160
Henderson AS, Jorm AF, Mackinnon A, Christensen H, Scott LR, Korten AE, Doyle C (1994) A survey of dementia in the Canberra population: experience with ICD-10 and DSM-III-R criteria. Psychol Med 24:473–482
Herrera E Jr, Caramelli P, Silveira AS, Nitrini R (2002) Epidemiologic survey of dementia in a community-dwelling Brazilian population. Alzheimer Dis Assoc Disord 16(2):103–108
Hototian SR, Lopes MA, Azevedo D Jr, Tatcsh M, Bazzarella MC, Bustamante SEZ, Litvoc J, Bottino CM (2008) Prevalence of cognitive and functional impairment in a community sample from São Paulo, Brazil. Dement Geriatr Cogn Disord 25(2):135–143
Instituto Brasileiro de Geografia e Estatística (IBGE) (2002) Perfil dos Idosos Responsáveis pelos Domicílios no Brasil 2000. IBGE, Rio de Janeiro, Brasil, n. 9, pp 1–97
Inzelberg R, Schechtman E, Abuful A, Masarwa M, Mazarib A, Stugatsky R, Farrer LA, Green RC, Friedland P (2007) Education effects on cognitive function in a healthy aged Arab population. Inter Psychogeriatr 19(3):593–603
Jones RN, Gallo JJ (2001) Education bias in the mini-mental state examination. Int Psychogeriatr 13(3):299–310
Jonker C, Geerlings MI, Schmand B (2000) Are memory complaints predictive for dementia? A review of clinical and population based studies. Int J Geriatr Psychiatry 15:983–991
Laks J, Baptista EMR, Coutino ALB, de Paula EO, Engelhardt E (2007) Mini-mental state examination norms in a community-dwelling sample of elderly with low schooling in Brazil. Cad Saúde Pública 23(2):315–319
Laks J, Batista EMR, Guilherme ERL, Coutinho ALB, Faria MEV, Figueira I, Engelhardt E (2003) O Mini Exame do Estado Mental em Idosos de uma Comunidade–Dados parciais de Santo Antônio de Pádua, Rio de Janeiro. Arq Neuropsiquiatr 61(3):782–785
Lavery LL, Lu S, Chang CH et al (2007) Cognitive assessment of older primary care patients with and without memory complaints. J Gen Intern Med 22(7):949–954
Lopes MA, Hototian SR, Bustamante SEZ, Azevedo D, Tatsch M, Bazzarella MC, Litvoc J, Bottino CM (2007) Prevalence of cognitive and functional impairment in a community sample in Ribeirão Preto, Brazil. Int J Geriatr Psychiatry 22:770–776
Lopponen M, Raiha I, Isoaho R, Vahlberg T, Kivela SL (2003) Diagnosing cognitive impairment and dementia in primary health care—a more active approach is needed. Age Ageing 32:606–612
Ng TP, Chiam PC, Kua EH (2007) Ethnic and educational differences in cognitive test performance on mini-mental state examination in Asians. Am J Geriatr Psychiatry 15(2):130–139
O’Bryant SE, Humphreys JD, Smith GE et al (2008) Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol 65(7):963–967
Palloni A, Pinto-Aguirre G, Pelaez M (2002) Demographic and health conditions of ageing in Latin America and the Caribbean. Int J Epidemiol 31:762–771
Riedel-Heller SG, Matschinger H, Schork A et al (1999) Do memory complaints indicate the presence of cognitive impairment? Results of a Field Study. Eur Arch Psychiatry Clin Neurosci 249:197–204
Scazufca M, Almeida OP, Vallada HP, Tasse WA, Menezes PR (2009) Limitations of the mini-mental state examination for screening dementia in a community with low socioeconomic status: results from the Sao Paulo Ageing & Health Study. Eur Arch Psychiatry Clin Neurosci 259(1):8–15
Sinclair AJ, Girling AJ, Bayer AJ (2000) Cognitive dysfunction in older subjects with diabetes mellitus: impact on diabetes self-management and use of care services. Diabetes Res Clin Pract 50:203–212
The Medical Research Council Cognitive Function and Ageing Study (2000) Survey into health problems of elderly people: a comparison of self-report with proxy information. Int J Epidemiol 29(4):684–697
Valle EA, Castro-Costa E, Firmo JO, Uchoa E, Lima-Costa MF (2009) A population-based study on factors associated with performance on the mini-mental state examination in the elderly: the Bambuí Study. Cad Saude Publica 25(4):918–926
Wood RY, Giuliano KK, Bignell CU, Pritham WW (2006) Assessing cognitive ability in research: use of MMSE with minority populations and elderly adults with low education levels. J Gerontol Nurs 32(4):45–54
Yamada M, Sasaki H, Mimori Y, Yamada M, Sasaki H, Mimori Y, Kasagi F, Sudoh S, Ikeda J, Hosoda Y, Nakamura S, Kodama K (1999) Prevalence and risks of dementia in the Japanese population: RERF’s adult health study Hiroshima subjects. Radiation Effects Research Foundation. J Am Geriatr Soc 47:189–195
Yesavage JA, Brink TL, Rose TL et al (1983) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr 17:37–49
Acknowledgments
We would like thank the elderly adults from São Paulo and Ribeirão Preto who agreed to participate in this research. This study was supported by “Fundação de Apoio à Pesquisa do Estado de São Paulo” (FAPESP), Grant no. 01/05959-7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moraes, C., Pinto, J.A., Lopes, M.A. et al. Impact of sociodemographic and health variables on mini-mental state examination in a community-based sample of older people. Eur Arch Psychiatry Clin Neurosci 260, 535–542 (2010). https://doi.org/10.1007/s00406-010-0104-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-010-0104-3