Abstract
The purpose of this study is to describe possible differences in cognitive functioning between smoking and non-smoking patients with first-episode psychosis and to determine whether there is a better cognitive profile associated with smoking. We assessed 61 first-episode psychosis patients with a neuropsychological battery that included computerized measurements of attention, working memory, and executive functioning. Patients were grouped into two categories: non-smokers (0 cigarettes/day; n = 30) and smokers (≥20 cigarettes/day; n = 31). No significant differences were detected in sociodemographic and clinical data between the two groups. For attention tasks, smokers exhibited shorter reaction times in the sustained attention test than non-smokers (P = 0.039) and needed less time to complete the Stroop interference test (P = 0.013). In the working memory task, smokers exhibited shorter reaction times (P = 0.029) and presented a significantly lower percentage of omission (P = 0.002) and commission errors (P = 0.020) than non-smokers. For executive functioning, no differences were detected between groups in performance on the Wisconsin Card Sorting Test. Results indicate that first-episode psychosis patients who are nicotine users have better cognitive functioning in the areas of attention and working memory than patients who are not nicotine users. This study supports the cognitive approach to the self-medication hypothesis, to explain the high rates of cigarette smoking among psychosis patients. These results may be relevant for developing new strategies involving nicotinic receptors for cognitive enhancement in psychosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well recognized that cigarette smoking is more prevalent among patients with psychosis, especially in schizophrenia, with rates of 70–80% versus 25–30% in the general population [13, 14, 21, 22]. The evidence for a relationship between cigarette smoking and schizophrenia is undeniable; however, the mechanisms underlying this relationship remain unclear. The remarkably high prevalence of smoking in schizophrenia patients has prompted speculation that smoking is an attempt at self-medication. One of the most popular approaches to the self-medication hypothesis is that smoking reverses the side effects of antipsychotic medication [15]. It has been reported that nicotine increases the metabolism of antipsychotics and decreases their therapeutic effects [9, 35], leading smoking patients to display fewer antipsychotic induced side effects, e.g., extrapyramidal symptoms [15, 20, 32]. However, controversy has arisen, as the metabolism of some atypical antipsychotics (e.g., risperidone, quetiapine, ziprasidone, and aripiprazole) has proven to be not sensitive to the effects of smoking [12]. Other contradictory evidence derives from the fact that 90% of patients who smoke start smoking before the onset of the illness and, therefore, before antipsychotic medications are prescribed [30]. Consequently, antipsychotic treatment alone may not explain the high rates of cigarette smoking among schizophrenia patients.
Another explanatory approach to the self-medication hypothesis is that smoking partly counteracts some of the cognitive deficits involved in the physiopathology of schizophrenia itself [38, 43, 46]. Cognitive deficits have been extensively studied in psychosis and have been characterized as an inherent feature of the illness [23]. Neuropsychological studies have consistently described deficits affecting attention, working memory, executive functioning, learning and memory [27]. These impairments have been described in first-episode patients, seem to be stable over time [1], are not exclusively explained by clinical symptomatology, and are present in individuals even before they develop psychotic symptoms [11].
There is increasing evidence that the altered expression of central nicotinic cholinergic receptors in schizophrenia may be related to the cognitive deficits associated with the illness [33, 42]. The hypothesis that smoking in psychosis may be a self-medication behavior to directly reverse cognitive deficits has been supported by evidence showing that cigarette smoking and other forms of nicotine administration (nasal spray, gum, or patch) produce positive effects on some of the psychophysiological abnormalities and neuropsychological impairments related to the illness. The literature has reported that nicotine administration transiently reverses eye-tracking abnormalities [3, 5, 39] and normalizes the auditory sensory gating (P50) deficit, both in patients and their relatives [2]. Studies also suggest that nicotine administration can improve attention and working memory deficits [6, 16, 28, 32, 44] and may reverse abstinence-related impairments in these cognitive domains in smoking patients [19, 45]. Additionally, nicotine has been shown to have positive effects on verbal memory deficits [37, 44], although not without controversy [32, 45], while no positive effects have yet been described on executive functioning deficits [42].
The main objectives of this study were to describe possible differences in cognitive functioning between smoking and non-smoking patients with first-episode psychosis (FEP) and to determine whether there is a better cognitive profile associated with smoking. We hypothesized that smoking patients would perform better on attention, working memory, and executive functioning tests than non-smoking patients. To our knowledge, no previous studies have evaluated this issue in FEP. Research on this population affords an opportunity to study the early phases of this disease and avoids dealing with certain confounding variables such as chronicity or long-term antipsychotic treatment that could interfere with the results.
Materials and methods
This article reports the baseline neuropsychological results based on smoking data from a prospective longitudinal study of FEP.
Subjects
Patients were recruited from inpatient and outpatient facilities in Vizcaya (a region in the North of Spain) that covered a catchment area of approximately 500,000 inhabitants. All patients consecutively seen in these facilities between March 2003 and November 2005 who fulfilled the inclusion criteria described below were invited to participate in the study. Visits were performed at two general hospitals in the geographical region.
Inclusion criteria for participation in the study were: (1) age between 15 and 65 years, (2) presence of FEP defined as the existence of at least one of the following symptoms: delusions, hallucinations, formal thought disorder, and catatonic symptoms, and symptoms were determined to be present when the Positive and Negative Syndrome Scale (PANSS) score for item 1, 2, or 3 was greater than or equal to 4, and (3) presence of a first degree relative to act as an informant, when necessary. Exclusion criteria were: (1) previous hospitalizations or outpatient psychiatric treatment for psychotic symptoms, (2) significant medical or neurological illness, (3) history of head injury with loss of consciousness, (4) mental retardation, (5) current diagnosis of substance dependence (except tobacco), and (6) participation in a clinical trial. A total of 89 patients with FEP were enrolled in a general FEP research project. Nicotine consumption was assessed by self-report in a personal interview and patients were classified into smoking categories according to previous literature [17, 19, 48]. Considering the specific aims of the present study, patients were selected from the general sample if they were non-smokers (0 cigarettes/day; n = 35) or if they were smokers and clearly habitual nicotine users (≥20 cigarettes/day; n = 36). Five patients in the group of non-smokers and five in the group of smokers did not cooperate with the neuropsychological evaluation, leaving a final sample of 61 patients divided into two groups as follows: (a) non-smoking FEP patients, n = 30; and (b) smoking FEP patients, n = 31. Mild smokers (1–19 cigarettes/day; n = 18) were not included in the analyses, as significant intra-subject variations in daily consumption were detected in this group, also reflecting a large dispersion of frequencies.
The institutional review boards of the participating hospitals approved the study. After receiving a comprehensive explanation of the study procedures, all patients provided written informed consent.
Psychiatric assessment
The Structured Clinical Interview for DSM-IV Axis I disorders [18] was used for diagnostic purposes. FEP was defined as the first time a patient displayed positive psychotic symptoms. All subjects satisfied the DSM-IV [4] criteria for a schizophreniform disorder, schizoaffective disorder, schizotypal disorder, delusional disorder, brief psychotic disorder, bipolar I/II disorder, substance-induced psychosis, or atypical psychosis. For diagnostic distribution, see Table 2. The presence and severity of psychotic symptoms at baseline were evaluated using the Spanish version of the Positive and Negative Syndrome Scale (PANSS) [41]. Other scales used for the clinical baseline assessment were: the Montgomery-Asberg Depression Rating Scale (MADRS) [36], the Young Mania Rating Scale (YMRS) [47], and the Clinical Global Impression (CGI) Scale [25]. The clinical presentation data (Table 2) correspond to discharge examinations at baseline. At the time of the neuropsychological assessment, all patients were on antipsychotic treatment (92% with an atypical antipsychotic).
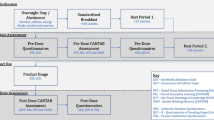
Neuropsychological assessment
The cognitive functioning of patients was assessed with a neuropsychological test battery that included computerized measurements of sustained and selective attention, working memory, and executive functioning. In the sustained attention task, the subject was instructed to press the button as quickly as possible when the letter O appeared on the screen. In the working memory task the subject was instructed to respond only when the letter O was preceded by the letter X. For both tasks, the following results were analyzed: mean reaction time for hits, percentage of commissions, and percentage of omissions. Selective attention was evaluated with the Stroop Color-Word Test-Interference (Stroop-I), in which the subject is asked to report when the color of the ink in which the color name is printed do not match each other, causing perceptual interference. The mean time to complete this task and the percentage of errors were recorded. Executive functioning was assessed using the Wisconsin Card Sorting Test (WCST). In this task, 128 cards are presented to the subject, who is asked to sort the cards on the basis of three different categories (color, shape, number) that the subject has to identify, maintain, and change throughout the test. The only feedback provided in this task is whether responses are correct or not. The WCST variables analyzed were number of categories completed (with a maximum of 6) and percentage of perseverative errors.
The tests were always administered by the same experienced clinical psychologist, trained in neuropsychological assessment, who was blind to the smoking status of the patient. Cognitive evaluations were performed during or immediately after discharge, when symptomatology was properly remitted.
Data analysis
Distributions of variables were examined and log-transformations were done in order to correct for skewness, where appropriate. Descriptive data are tabulate as means and standard deviations (SD) or medians and inter-quartile ranges (IQR). Differences in the demographic and clinical characteristics between groups were assessed using Student’s t tests for the continuous data and chi-square analyses for the nominal data. Differences in cognitive performance between patient groups were analyzed with a full factorial multivariate analysis of covariance (MANCOVA) model, using group (smoker, non-smoker) as fixed factor, neuropsychological test performance scores as dependent variables, diagnosis as the covariate and Bonferroni correction for multiple comparisons. All statistical tests were two-tailed and analyses were performed using SPSS for Windows software, version 11.5.1.
Results
No significant differences were detected between smoking and non-smoking FEP patients with respect to sociodemographic data (Table 1) or clinical features (Table 2). There were no significant differences in distribution of antipsychotic treatment among the groups, χ²(2) = 0.238, P = 0.888. Forty-three percent (n = 13) of the non-smoking patients were on olanzapine, 40% (n = 12) on risperidone, and 17% (n = 5) on other antipsychotic treatments. Similarly, 48% (n = 15) of the smoking patients were on olanzapine, 39% (n = 12) on risperidone, and 13% (n = 4) on other antipsychotic treatments.
Neuropsychological data are summarized in Table 3. Smoking patients exhibited shorter reaction times than non-smokers in the sustained attention task, with no differences in the percentage of omission or commission errors. Compared to non-smokers, smokers needed significantly less time to complete the Stroop-I task with no significant differences in the percentage of correct responses. For the working memory task, smokers exhibited shorter reaction times than non-smokers and presented a significantly lower percentage of omission errors, with no differences in the percentage of commission errors. No differences were detected between groups in the number of categories completed or in the percentage of perseverative errors on the WCST.
Discussion
The primary result of this study is the detection of a different cognitive profile for smoking and non-smoking patients with FEP. Those patients who were classified as smokers showed better neuropsychological performance on attention and verbal working memory tasks than non-smoking patients. However, the potential benefits of nicotine on cognition in our sample of smoking patients did not extend to all areas, since no differences in executive functioning were detected between groups. This outcome is in accordance with previous reports in which it has been concluded that nicotine improves performance on specific domains of cognition in schizophrenia patients, with attention and working memory being the most replicated areas [26, 42, 45].
The group of smoking patients showed significantly overall lower reaction times on attention and verbal working memory tasks than non-smokers. Results also indicate that the accuracy in the response was not negatively affected by a faster response in the attention tasks, but even accuracy was increased in the verbal working memory test. This pattern indicating beneficial scores with faster perceptual processing speed for those patients who are cigarette smokers in the areas of attention and working memory is supported by recent studies that have described how nicotine withdrawal in smoking schizophrenia patients led to a worsen performance in sustained attention and spatial working memory tasks and how reinstatement reversed abstinence-related impairments in these cognitive domains [42, 45]. Similarly, other studies assessing the cognitive effects of smoking and nicotine administration in schizophrenia patients have reported a nicotine mediated benefit on sustained attention and spatial working memory measures in smoking schizophrenia patients [16, 31, 42]. However, it should be noted that the potential benefits of nicotine on selective attention in psychosis has not been as consistently reported. During short-term/overnight abstinence, no significant changes in Stroop-I performance have been detected [42] and conversely to our results, a previous study comparing smoking (n = 23) versus non-smoking (n = 8) patients did not find differences in response time in Stroop-I baseline performance between groups [19]. However, this same study supports the idea of this positive influence of nicotine on selective attention, as those patients who quit smoking (n = 8) showed an increase in reaction times on the Stroop-I task compared with patients who continued smoking (n = 15) in a 3-week follow-up assessment. The fact that nicotine may have a beneficial effect not only on sustained attention but also on selective attention has been described in a healthy non-smoking population and in non-smoking schizophrenia patients after transdermal nicotine administration, with the improvement in scores being greater in the latter group [6].
We did not detect significant differences in performance on the WCST between our smoking and non-smoking FEP patients. In keeping with this result, no previous studies have reported potential nicotine-related benefits to executive functioning in patients with psychosis [42].
The specific differences in the cognitive pattern described between our smoking and non-smoking patients support a possible nicotine mediated enhancement that may affect selectively concrete areas of cognition such as attention and working memory. Additionally, our results offer new evidence that in this last domain, the positive effects of nicotine described in schizophrenia may be not exclusive to visuospatial information processing but also apply to its verbal modality. To our knowledge no previous studies have compared performance on a verbal working memory task between smoking and non-smoking patients. Enhancement of performance on a verbal task similar to the one used in this study has been reported in a healthy non-smoking population and in non-smoking schizophrenia patients after transdermal nicotine administration [6].
Overall, our results support the cognitive approach to the self-medication hypothesis, to explain the high rates of smoking in psychosis patients [48]. Based on the assumption that nicotine administration enhances specific cognitive deficits and on the reported reduction in central nicotinic cholinergic receptors in schizophrenia and its relationship to the cognitive impairment associated with the illness, new pharmacological strategies are being developed for cognitive augmentation. For example, alpha-7 nicotinic acetylcholine receptor agonists appear to be viable candidates for the treatment of cognitive deficits in schizophrenia [33, 42], whereas negative results have been recently reported for the cholinesterase inhibitor donepezil [29].
One limitation of the present study is that it was not designed with an experimental methodology and, therefore, it is not clear if the differences detected are due to nicotine, other components of cigarettes, or the fact of smoking. A second limitation is that, although non-significant differences were detected in the distribution of the type of antipsychotic treatment between groups, we did not control our results for the potential effects of medication and its relationship to the smoking status of the patient. One of the most popular explanations for the high rates of cigarette smoking in schizophrenia has been that patients smoke primarily to reverse the side-effects of the antipsychotic drugs. However, this hypothesis may be controversial considering the following facts: (a) the metabolism of some atypical antipsychotics is not sensitive to the effects of smoking [30], (b) rates of noncompliance with antipsychotic medication have been estimated around 43–78% in chronic patients [40] and up to 59% in first-episode patients after a one-year follow-up [8], (c) first-episode patients present the same prevalence of smoking as chronic patients, [34] and (d) 90% of smoking patients with schizophrenia start smoking before the onset of the illness [30]. On the contrary, there is evidence to support direct beneficial effects of cigarette smoking on cognition in psychosis, independent of its interactions with antipsychotics, as these beneficial effects have been described not only in patients, but also in their first-degree relatives [24]. Deficits in attention and working memory processes have been described in a population at high risk for development of psychosis and are considered to be present in the premorbid phases [7, 10]. Some authors have asserted that neurocognitive deficits may constitute a vulnerability factor for the initiation and maintenance of cigarette smoking in schizophrenia [42], supporting the direct therapeutic effects of nicotine on cognition. These findings may indicate that it is the illness and not its treatment with antipsychotic drugs that determines the high prevalence of cigarette smoking in psychosis [34].
Conclusion
First-episode psychosis patients who are nicotine users present better cognitive functioning in the areas of attention and working memory than first-episode patients who are not nicotine users. Smoking may constitute a self-medication behavior to enhance neuropsychological dysfunction. This may be relevant to developing new pharmacotherapies for cognitive deficits in psychosis and establishing strategies to reduce cigarette-smoking rates in this population.
References
Addington J, Saeedi H, Addington D (2005) The course of cognitive functioning in first episode psychosis: changes over time and impact on outcome. Schizophr Res 78:35–43
Adler LE, Hoffer LD, Wiser A, Freedman R (1993) Normalization of auditory physiology by cigarette smoking in schizophrenic patients. Am J Psychiatry 150:1856–1861
Adler LE, Olincy A, Waldo M, Harris JG, Griffith J, Stevens K, Flach K, Nagamoto H, Bickford P, Leonard S, Freedman R (1998) Schizophrenia, sensory gating, and nicotinic receptors. Schizophr Bull 24:189–202
American Psychiatric Association A (1994) Diagnostic and statistical manual of mental disorders. APA, Washington DC
Avila MT, Sherr JD, Hong E, Myers CS, Thaker GK (2003) Effects of nicotine on leading saccades during smooth pursuit eye movements in smokers and nonsmokers with schizophrenia. Neuropsychopharmacology 28:2184–2191
Barr RS, Culhane MA, Jubelt LE, Mufti RS, Dyer MA, Weiss AP, Deckersbach T, Kelly JF, Freudenreich O, Goff DC, Evins AE (2007) The Effects of Transdermal Nicotine on Cognition in Nonsmokers with Schizophrenia and Nonpsychiatric Controls. Neuropsychopharmacology 33(3):480–490
Chen WJ, Liu SK, Chang CJ, Lien YJ, Chang YH, Hwu HG (1998) Sustained attention deficit and schizotypal personality features in nonpsychotic relatives of schizophrenic patients. Am J Psychiatry 155:1214–1220
Coldham EL, Addington J, Addington D (2002) Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand 106:286–290
Dalack GW, Meador-Woodruff JH (1996) Smoking, smoking withdrawal and schizophrenia: case reports and a review of the literature. Schizophr Res 22:133–141
Davalos DB, Compagnon N, Heinlein S, Ross RG (2004) Neuropsychological deficits in children associated with increased familial risk for schizophrenia. Schizophr Res 67:123–130
Davidson M, Reichenberg A, Rabinowitz J, Weiser M, Kaplan Z, Mark M (1999) Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry 156:1328–1335
de Leon J (2004) Psychopharmacology: atypical antipsychotic dosing: the effect of co-medication with anticonvulsants. Psychiatr Serv 55:125–128
de Leon J, Becona E, Gurpegui M, Gonzalez-Pinto A, Diaz FJ (2002) The association between high nicotine dependence and severe mental illness may be consistent across countries. J Clin Psychiatry 63:812–816
de Leon J, Diaz FJ (2005) A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res 76:135–157
Decina P, Caracci G, Sandik R, Berman W, Mukherjee S, Scapicchio P (1990) Cigarette smoking and neuroleptic-induced parkinsonism. Biol Psychiatry 28:502–508
Depatie L, O’Driscoll GA, Holahan AL, Atkinson V, Thavundayil JX, Kin NN, Lal S (2002) Nicotine and behavioral markers of risk for schizophrenia: a double-blind, placebo-controlled, cross-over study. Neuropsychopharmacology 27:1056–1070
Eppolito AK, Smith RF (2006) Long-term behavioral and developmental consequences of pre- and perinatal nicotine. Pharmacol Biochem Behav 85:835–841
First M, Spittzer R, Gibbon M, Williams J (1995) Structured Clinical Interview for DSM-IV axis I disorders, patient ediction (SCID-P), Version 2. Biometrics Research, New York
George TP, Vessicchio JC, Termine A, Sahady DM, Head CA, Pepper WT, Kosten TR, Wexler BE (2002) Effects of smoking absinence on visuospatial working memory function in schizophrenia. Neuropsychopharmacology 26:75–85
Goff DC, Henderson DC, Amico E (1992) Cigarette smoking in schizophrenia: relationship to psychopathology and medication side effects. Am J Psychiatry 149:1189–1194
Gonzalez-Pinto A, Gutierrez M, Ezcurra J, Aizpuru F, Mosquera F, Lopez P, de Leon J (1998) Tobacco smoking and bipolar disorder. J Clin Psychiatry 59:225–228
González Pinto A, Gutiérrez M, de León J, Mosquera F, Elizagarate E, BR (1998) Tabaquismo en población psiquiátrica. Actas Luso-Españolas de Neurología, Psiquiatría y Ciencias Afines 26:48–50
Green MF (2006) Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry 67:e12
Griffith JM, O’Neill JE, Petty F, Garver D, Young D, Freedman R (1998) Nicotinic receptor desensitization and sensory gating deficits in schizophrenia. Biol Psychiatry 44:98–106
Guy W (1976) Assessment manual for psychopharmacology (revised). US Department of Health, Education and Welfare, Rockville, MD
Harris JG, Kongs S, Allensworth D, Martin L, Tregellas J, Sullivan B, Zerbe G, Freedman R (2004) Effects of nicotine on cognitive deficits in schizophrenia. Neuropsychopharmacology 29:1378–1385
Heinrichs RW, Zakzanis KK (1998) Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 12:426–445
Jacobsen LK, D’Souza DC, Mencl WE, Pugh KR, Skudlarski P, Krystal JH (2004) Nicotine effects on brain function and functional connectivity in schizophrenia. Biol Psychiatry 55:850–858
Keefe RS, Malhotra AK, Meltzer HY, Kane JM, Buchanan RW, Murthy A, Sovel M, Li C, Goldman R (2008) Efficacy and safety of donepezil in patients with schizophrenia or schizoaffective disorder: significant placebo/practice effects in a 12-week, randomized, double-blind, placebo-controlled trial. Neuropsychopharmacology 33(6):1217–1228
Kelly C, McCreadie RG (1999) Smoking habits, current symptoms, and premorbid characteristics of schizophrenic patients in Nithsdale, Scotland. Am J Psychiatry 156:1751–1757
Levin ED, Conners CK, Sparrow E, Hinton SC, Erhardt D, Meck WH, Rose JE, March J (1996) Nicotine effects on adults with attention-deficit/hyperactivity disorder. Psychopharmacology (Berl) 123:55–63
Levin ED, Wilson W, Rose JE, McEvoy J (1996) Nicotine-haloperidol interactions and cognitive performance in schizophrenics. Neuropsychopharmacology 15:429–436
Martin LF, Freedman R (2007) Schizophrenia and the alpha7 nicotinic acetylcholine receptor. Int Rev Neurobiol 78:225–246
McEvoy JP, Brown S (1999) Smoking in first-episode patients with schizophrenia. Am J Psychiatry 156:1120–1121
Miller DD, Kelly MW, Perry PJ, Coryell WH (1990) The influence of cigarette smoking on haloperidol pharmacokinetics. Biol Psychiatry 28:529–531
Montgomery SA, Asberg M (1979) A new depression scale designed to be sensitive to change. Br J Psychiatry 134:382–389
Myers CS, Robles O, Kakoyannis AN, Sherr JD, Avila MT, Blaxton TA, Thaker GK (2004) Nicotine improves delayed recognition in schizophrenic patients. Psychopharmacology (Berl) 174:334–340
Nomikos GG, Schilstrom B, Hildebrand BE, Panagis G, Grenhoff J, Svensson TH (2000) Role of alpha7 nicotinic receptors in nicotine dependence and implications for psychiatric illness. Behav Brain Res 113:97–103
Olincy A, Johnson LL, Ross RG (2003) Differential effects of cigarette smoking on performance of a smooth pursuit and a saccadic eye movement task in schizophrenia. Psychiatry Res 117:223–236
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353:487–497
Peralta V, Cuesta M (1994) Validación de la escala de los síndromes positivo y negativo (PANSS) en una muestra de esquizofrénicos españoles. Actas Luso Esp Neurol Psiquiatr 22:171–177
Sacco KA, Termine A, Seyal A, Dudas MM, Vessicchio JC, Krishnan-Sarin S, Jatlow PI, Wexler BE, George TP (2005) Effects of cigarette smoking on spatial working memory and attentional deficits in schizophrenia: involvement of nicotinic receptor mechanisms. Arch Gen Psychiatry 62:649–659
Sherr JD, Myers C, Avila MT, Elliott A, Blaxton TA, Thaker GK (2002) The effects of nicotine on specific eye tracking measures in schizophrenia. Biol Psychiatry 52:721–728
Smith RC, Singh A, Infante M, Khandat A, Kloos A (2002) Effects of cigarette smoking and nicotine nasal spray on psychiatric symptoms and cognition in schizophrenia. Neuropsychopharmacology 27:479–497
Smith RC, Warner-Cohen J, Matute M, Butler E, Kelly E, Vaidhyanathaswamy S, Khan A (2006) Effects of nicotine nasal spray on cognitive function in schizophrenia. Neuropsychopharmacology 31:637–643
Taiminen TJ, Salokangas RK, Saarijarvi S, Niemi H, Lehto H, Ahola V, Syvalahti E (1998) Smoking and cognitive deficits in schizophrenia: a pilot study. Addict Behav 23:263–266
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435
Zammit S, Allebeck P, Dalman C, Lundberg I, Hemmingsson T, Lewis G (2003) Investigating the association between cigarette smoking and schizophrenia in a cohort study. Am J Psychiatry 160:2216–2221
Acknowledgments
This study was supported in part by the University of the Basque Country (UPV-EHU), the Spanish Department of Health, Instituto de Salud Carlos III, Mental Health CIBER-SAM, RETICS RD06/0011(REM-TAP Network), and by grants PI01/1455; PI05/1508 (Spanish Department of Health: Healthcare Research Fund).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zabala, A., Eguiluz, J.I., Segarra, R. et al. Cognitive performance and cigarette smoking in first-episode psychosis. Eur Arch Psychiatry Clin Neurosci 259, 65–71 (2009). https://doi.org/10.1007/s00406-008-0835-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-008-0835-6