Abstract
Neurofunctional mechanisms underlying cognitive behavior therapy (CBT) are still not clearly understood. This functional magnetic resonance imaging (fMRI) study focused on changes in brain activation as a result of one-session CBT in patients suffering from spider phobia. Twenty-six female spider phobics and 25 non-phobic subjects were presented with spider pictures, generally disgust-inducing, generally fear-inducing and affectively neutral scenes in an initial fMRI session. Afterwards, the patients were randomly assigned to either a therapy group (TG) or a waiting list group (WG). The scans were repeated one week after the treatment or after a one-week waiting period. Relative to the non-phobic participants, the patients displayed increased activation in the amygdala and the fusiform gyrus as well as decreased activation in the medial orbitofrontal cortex (OFC) during the first exposure. The therapy effect consisted of increased medial OFC activity in the TG relative to the WG. Further, therapy-related reductions in experienced somatic anxiety symptoms were positively correlated with activation decreases in the amygdala and the insula. We conclude that successful treatment of spider phobia is primarily accompanied by functional changes of the medial OFC. This brain region is crucial for the self-regulation of emotions and the relearning of stimulus-reinforcement associations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spider phobia is a common anxiety disorder with a point prevalence of 3.5% in the general population [5]. The predominantly female sufferers experience intense fear when confronted with spiders, and as a result develop pronounced avoidance behavior that subsequently interferes with their normal occupational and social functioning. The somatic fear response, which in some cases may escalate into panic attacks, is sympathetically dominated and includes increases in heart rate, electrodermal activity, and blood pressure [10, 22, 23]. Electrocortical changes, such as enhancements of P300 potentials during symptom provocation, mirror the fast neural processing of phobia-relevant information [21].
Since EEG parameters are characterized by a high temporal but a low spatial resolution, brain-imaging methods such as positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) show promise as being helpful tools for pinpointing the neural substrates of spider phobia. Several PET and fMRI studies have been conducted where phobic symptoms were experimentally provoked. The observed activation pattern included the visual association cortex [4, 6, 24, 27], the orbitofrontal and dorsolateral prefrontal cortex [4, 6, 12, 24, 25, 27], the hippocampus/parahippocampal gyrus [6, 24], the insula [4, 11, 25] and the amygdala [4, 11, 16, 27]. Overall, these studies were quite consistent in demonstrating the significance of the extrastriate cortex and fronto-temporal regions for phobic states.
Aside from symptom provocation, the investigation of treatment effects on brain activity forms a second promising approach to broaden the knowledge on the pathophysiology of spider phobia [7, 9, 18]. Cognitive behavior therapy (CBT) is currently the most effective intervention method for individuals suffering from this disorder [1]. The patients are taught to gradually approach spiders until their anxiety is considerably reduced and to correct their misattributions about the animal. Despite the fact that controlled clinical trials have demonstrated positive and long-lasting therapy outcomes [22, 23], there are only two fMRI studies in the literature on CBT effects in spider phobia [24, 28]. Paquette et al. [24] scanned patients while they viewed film excerpts showing spiders and butterflies before and after CBT. The first presentation of the spider film was associated with significant activation of the dorsolateral prefrontal cortex (DLPFC) and the parahippocampal gyrus, which was not present anymore after successful CBT completion. The authors suggest that the activation decrease reflects the deconditioning of contextual fear at the level of the parahippocampus and the reduction of cognitive misattributions at the level of the prefrontal cortex. This interpretation however may be premature, since the authors only studied a therapy group (TG) and did not include a waiting list group (WG) in their experimental design. Without studying a group, which did not receive CBT, observed activation changes cannot be attributed to the treatment per se and may be habituation effects due to the repeated presentation of the phobic stimulus.
This methodological problem was solved in a study by Straube et al. [28] who investigated a TG, a WG and a healthy control group. The subjects were exposed to film clips either showing a moving spider or a control object. The first viewing of the spider provoked greater insula and anterior cingulate cortex (ACC) activation in the phobic sample relative to the control sample. Following successful CBT, the TG (and not the WG) displayed activation attenuation in the insula and the ACC. Since both brain regions are concerned with the regulation of autonomic responses to emotional events, their functional change was interpreted to indicate a therapy-induced normalization of hyperactivation.
The most critical aspect of this investigation refers to the fact that the initial symptom provocation elicited greater amygdala activation in the non-phobic relative to the phobic subjects. This finding is very surprising considering the crucial function of the amygdala for the decoding of emotional salience in general, and fear relevance in particular [17]. Neither in the experiment by Paquette et al. [24], nor in the study by Straube et al. [28], was a hyperactivation of the amygdala observed before therapy and neither of the authors reported a reduction in amygdala activity after treatment. This is at odds with current models of the pathophysiology of specific phobia [18].
The design of the present fMRI investigation was an extension of the experiment by Straube et al. [28]. We investigated spider phobics who had been randomly assigned to either a TG or a WG and compared them with non-phobic subjects. The patients were scanned twice during a picture perception experiment; either before/after CBT, or before/after a comparable waiting period. The design was extended by additionally presenting the subjects with generally fear- and disgust-evoking pictures. This was done in order to explore the neural response specificity to phobic vs. generally aversive stimuli. Further, we were interested in the hemodynamic pattern of symptom provocation during the first picture presentation and expected activation in previously detected phobia-relevant brain regions (DLPFC, lateral OFC, amygdala, insula, ACC, parahippocampal gyrus, and extrastriate cortex). Finally, we examined the effects of CBT on brain activity. Response changes from the first to the second fMRI session were analyzed separately within the WG and TG, and then compared between the groups. We tested if previously described therapy effects, such as activation decreases in the DLPFC, the parahippocampus, the insula and the ACC [24, 28], would also be present in the TG of the current study.
Materials and method
Subjects
Twenty-eight female patients suffering from spider phobia (DSM-IV: 300.29) participated in the experiment. They had been recruited via announcements in local newspapers and at the campus. The patients had been randomly assigned to either a therapy group (TG) or a waiting list group (WG). Both groups were comparable with respect to age (Mean (SD): TG = 27.2 years, (9.2); WG = 24.3 years, (2.0) and years of education (mean TG = 15.2 years; WG = 14 years). Two of the WG participants did not complete the second session and were therefore excluded from the analysis. This left 12 WG subjects and 14 TG subjects in the samples. We also studied 25 non-phobic females, who were comparable to the patient group with respect to age and socioeconomic status (mean age: M = 24.6 years; SD = 6.3; years of education: M = 14.5). All subjects were medication-naïve and right-handed. They gave written informed consent after the nature of the experiment had been explained to them. The ethics committee of the German Society of Psychology approved this study.
Procedure
After a first phone screening, the subjects were invited to a diagnostic session. Here they were interviewed with the short form of the clinical interview for DSM-IV [19]. Then, the participants filled out the Spider Phobia Questionnaire (SPQ, [14]) and underwent a behavior test. A spider was put in a transparent case and placed 5 m from the subjects, who were then instructed to approach the box. The subjects received points (range: 1–12) based on their approach behavior (1 point = no movement, 12 points = removing the spider from the box and holding it in their hands for 20 s). The diagnostic session was ended with an anatomical scan (duration: 5 min) in order to familiarize the subjects with the tomograph.
The first fMRI session had been scheduled approximately one week after the diagnostic session. Here, the subjects were exposed to a total of 160 pictures representing four emotional categories: ‘Spider’, ‘Fear’, ‘Disgust’ and ‘Neutral’. Most of the scenes (116) had been selected from a picture set of the authors. The other scenes were chosen from the International Affective Picture System [15]. The phobia-relevant pictures showed spiders in different environments. Disgust-relevant scenes represented the domains ‘poor hygiene’ and ‘repulsive animals’ (e.g., cockroaches, worms). Threatening pictures showed attacks by animals (e.g., sharks, lions) or humans (e.g., with knives or pistols), whereas neutral scenes consisted e.g., of household articles, or geometric figures. Each picture was shown for 1.5 s within a block consisting of 40 pictures of the same category. Within a sixty-second block the pictures directly followed each other in a randomized sequence. Each block was shown six times during the course of the experiment in a quasi-randomized order with the restriction that no more than two categories of the same type were allowed to follow each other. There were no pauses between the blocks. The total experiment lasted 24 minutes. The pictures were viewed by means of a mirror attached to the head coil (visual field = 18°).
After the scanning, subjects rated their impression of the 40 pictures from a category on four nine-point Likert scales for the dimensions arousal, valence, fear and disgust (range: 1–9, with ‘9’ indicating that the subject felt very aroused, pleasant, anxious and disgusted). In addition, they estimated the intensity of experienced panic symptoms (e.g., pounding heart, sweating) as described in the DSM-IV (criteria for panic attacks). Possible mean scores ranged from 1 (no symptoms) to 9 (very intense symptoms).
The CBT [22, 23] was scheduled in the following week after the first fMRI session (the WG received no treatment). The program consisted of a one-session therapy of approximately 4 h and combined exposure in vivo and modeling. The patients, who participated in groups of up to four patients, were taught to gradually approach a spider (e.g., looking at a spider, catching a spider with a glass and a piece of paper, holding a spider in the hands). Each task was first demonstrated by the therapist and then repeated by the patient. A task was considered as successfully managed when the anxiety level had been reduced by at least 50% of its highest value.
The second fMRI session was repeated one week after the treatment for the TG and after one-week of waiting for the WG. Again, the subjects underwent the behavior test and filled out the SPQ prior to the scanning. Subsequent to the picture presentation they were asked to rate the stimulus material with regard to arousal, valence, disgust, fear and experienced panic symptoms.
Imaging and statistical analysis
Brain images were acquired using a 1.5 T whole-body tomograph (Siemens Symphony, Erlangen, Germany) with a standard head coil. For the functional imaging a total of 492 volumes were registered using a T 2*-weighted gradient echo-planar imaging sequence (EPI) with 30 slices covering the whole brain (slice thickness = 5 mm, no gap, interleaved, TE = 60 ms, flip angle = 90°, field of view = 192 mm × 192 mm, matrix size = 64 × 64). The orientation of the axial slices was parallel to the AC-PC line. The first 6 volumes were discarded to control for saturation effects. For the preprocessing and statistical analyses the statistical parametric mapping software package (SPM2, Wellcome Department of Cognitive Neurology, London) implemented in Matlab (Mathworks, Inc., Natick, MA, USA, release 12) was used, which is based on the general linear model (GLM) approach. Slice time correction, realignment and normalization to the standard space of the Montreal Neurological Institute brain were performed. Smoothing was executed with an isotropic three-dimensional Gaussian filter with a full width at half maximum (FWHM) of 9 mm. Each of the four experimental conditions Phobia, Neutral, Disgust and Fear was modeled by a boxcar function convolved with a hemodynamic response function in the GLM. The six movement parameters of the rigid body transformation applied by the realignment procedure were introduced as covariates in the model. Serial correlations were controlled by an AR(1) process; the high pass filter was set at 512 s.
Several t-contrasts (first level) were calculated for each subject. The effects of the symptom provocation during the first session (1) were studied by analyzing the contrast Phobia1 > Neutral1. We also contrasted the Phobia with the Disgust and the Fear condition in order to separate phobia-specific activation from activation which is generally present during the processing of aversive stimuli (Phobia1 </> Disgust 1; Phobia1 </> Fear1). Then, we analyzed the response changes from the first (1) to the second (2) session. We checked for decreases of activation ([Phobia1 > Neutral1] > [Phobia2 > Neutral2]) and increases of activation ([Phobia2 > Neutral2] > [Phobia1 > Neutral1]) in the phobic sample. These contrasts were then used in second level random effect analyses. First, we investigated the activation in the phobic and the control sample separately with one sample t-tests. Two-sample t-tests were conducted in order to compare the subject groups with each other.
We computed exploratory voxel intensity tests for the whole brain volume and for the following regions of interest (ROIs): amygdala, ACC, insula, medial/lateral OFC, DLPFC, fusiform gyrus, and parahippocampal gyrus. The ROIs had been defined by the anatomical parcellation of the normalized brain (single-subject high-resolution T1 volume of the Montreal Neurological Institute) as described by Tzourio-Mazoyer et al. [29]. Based on this assignment between anatomical structures and voxel coordinates we created masks with the MARINA software [31]. When exploratory analyses were conducted, p was corrected for the whole brain volume, when a ROI-test was used p was corrected for the specific volume of interest. The multiple comparison correction (family-wise error) was based on the Gaussian random field theory [2]. The significance level was always set to alpha = 0.05.
Results
Self-report and behavior test data
Effects of the symptom provocation in the first session
The therapy group (TG) and the waiting list group (WG) did not differ in the degree of reported phobic symptoms (SPQ) and in the performance during the behavior test. Both groups kept a distance of approximately one meter from the spider box. There were no differences in the affective ratings (valence, arousal, fear, disgust, panic) for the spider pictures between the TG and WG (Table 1). All control subjects held the spider for 20 s in their hands and had significantly lower SPQ scores than the phobic subjects (t(49) = 33, P < 0.001). Relative to the patients, the non-phobic participants gave lower ratings for experienced fear, disgust, arousal and panic as well as higher valence ratings for the spider pictures (all P < 0.01; Table 1).
Changes of self-reports from the first to the second session
The therapy group (TG) reported a pronounced reduction in phobic symptoms (SPQ) from the first to the second session, whereas the SPQ scores for the waiting list group (WG) hardly changed (Table 1). The conducted analysis of variance with the factors group (WG, TG) and session (1, 2) resulted in a significant interaction effect (F(1,24) = 165, P < 0.001). The behavior test indicated that all of the TG patients were able to hold the spider in their hands after the therapy. In contrast, the WG subjects still kept a distance of approximately one meter from the spider box. The interaction effect group x session was highly significant (F(1,24) = 163, P < 0.001).
Pronounced changes in the affective ratings for the spider pictures only occurred in the TG and were in the predicted direction with a reduction in experienced fear, disgust, arousal, and panic as well as with an increase in valence ratings from the first to the second session (Table 1). The analyses of variance showed significant interactions group × session for all ratings (fear: F(1,24) = 10, P = 0.004; disgust: F(1,24) = 22, P < 0.001; arousal: F(1,24) = 31, P < 0.001; valence: F(1,24) = 52, P < 0.001; panic: F(1,24) = 3.9, P = 0.001).
Brain imaging data
Effects of symptom provocation in the first session
Across patient groups (TG + WG): There were no differences between the therapy group (TG) and the waiting list group (WG) for the contrast Phobia1 > Neutral1. Therefore, the groups were combined. The exploratory analysis revealed significant activation in the right superior occipital gyrus. ROI activation occurred bilaterally in the amygdala, the insula, the parahippocampal gyrus, and the fusiform gyrus as well as in the right lateral OFC and the ACC (Table 2).
Control Group: The exploratory analysis indicated significant activation in the bilateral angular gyrus, the right lingual gyrus and in the left ACC. Significant ROI effects were observed for the bilateral medial OFC, DLPFC and fusiform gyrus as well as for the right insula and the right ACC.
Phobic Group > Control Group: The phobic patients showed greater ROI activation in the left amygdala and in the bilateral fusiform gyrus than the control subjects.
Control Group > Phobic Group: The non-phobic subjects displayed stronger responses in the right inferior parietal gyrus and in the inferior frontal gyrus (exploratory effects) as well as in the bilateral ACC, the medial OFC, and the right DLPFC (ROI effects).
Comparison of responses to phobia, disgust and fear pictures
In order to differentiate phobia-specific response components from those components which are characteristic for the processing of generally aversive stimuli, we compared the Phobia, Disgust and Fear conditions with each other. Since the TG and the WG had shown comparable activation to the generally disgust-evoking and fear-evoking pictures (contrasts: Disgust1 > Neutral1, Fear1 > Neutral1), both patient samples were combined when contrasting the disorder-relevant with the other emotion conditions.
Across patient groups (TG + WG): Relative to the disgust-inducing pictures (Phobia1 > Disgust1), spider pictures induced greater activation in the bilateral ACC, the right insula, the right amygdala and the left DLPFC. The contrast Phobia1 > Fear1 was associated with right ACC activation. The reversed contrasts Disgust1 > Phobia1 and Fear1 > Phobia1 were both characterized by medial OFC involvement (Table 3).
Activation changes from the first to the second session
Therapy group: The TG showed an activation reduction from the first to second session in the right insula. The effect for the left parahippocampal gyrus was marginally significant (P = 0.06). An increase in activation occurred in the right medial OFC (Table 4).
Waiting list group: The WG was characterized by a reduction in activation in the bilateral parahippocampal gyrus as well as in the right lateral and left medial OFC. There was no significant activation increase from the first to the second session.
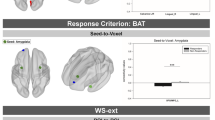
TG > WG: When contrasting the response increases (Phobia2 > Phobia1) between the two groups, the interaction effect was highly significant (Table 4, Fig. 1). As a result, the TG showed greater left (MNI x,y,z: −9,33,−12, t = 4.5, P = 0.023) as well as right medial OFC activation (MNI x,y,z: 12,42,−3, t = 5.0, P = 0.009) than the WG in the second session. Results for the contrast Phobia 1 > Phobia2 were nonsignificant.
Correlations between changes in activation and affective ratings
TG: Since we did not find therapy-related activation decreases in those brain areas which are considered to be core structures of the central fear circuit (e.g., the amygdala), we additionally executed exploratory correlation analyses (simple regression) for the therapy group. We explored the association between changes in ROI activation and changes in affective ratings. There was a positive correlation between the reduction of experienced somatic panic symptoms and an activation decrease in the right amygdala (MNI x,y,z: 24,0,−18, t = 7.8, P < 0.001) and in the left insula (−39,6,3, t = 8.3, P < 0.001). The reduction of arousal ratings was positively correlated with a decrease of the right amygdala response (24,0,−15, t = 3.8, P = 0.033).
Discussion
This fMRI study focused on the neural activation pattern during symptom provocation in spider phobia and on activation changes as a result of CBT.
The symptom provocation was successfully realized by exposing the phobic subjects to spider pictures, which had been perceived as highly arousing and unpleasant. Their initial viewing relative to neutral scenes was accompanied by increased activation of the visual association cortex (including the fusiform gyrus), the amygdala, the insula, the dorsal ACC, the parahippocampal gyrus and the lateral OFC in the patient group. This pattern is in accordance with previous neuroimaging studies where activity in these brain regions had also been observed during exposure [4, 6, 25, 27].
Relative to the control group, the patients showed greater activation of the amygdala and the extrastriate cortex while viewing the phobic material for the first time. Both brain regions have been conceptualized as core elements of the neural fear circuit [17]. They are critical for recruiting and coordinating cortical arousal and for the maintenance of attention. These processes are accomplished by the extensive bilateral connectivity between both brain regions [32].
Further evidence for the important phobia-relevant function of the amygdala became obvious when contrasting the Phobia with the Disgust condition. Here, the amygdala together with the insula showed increased activity in the phobic state. However, a comparable amygdala engagement was observed in the Phobia and Fear condition, which would point to an overlap of involved brain regions in phobia-specific and general threat processing. Activation differences were restricted to the dorsal ACC, a region involved in cognitive control processes [3].
Taken together the symptom provocation had been successfully realized and both patient groups (TG and WG) not only showed comparable hemodynamic responses during the first session, but were also characterized by an equivalent symptom severity as indicated by the SPQ scores, by the avoidance test performance, and by similar affective ratings for the spider scenes. This situation considerably changed during the second fMRI session. After successful CBT completion the TG reported significantly less phobic symptoms (SPQ) and rated the spider pictures as hardly arousing, disgusting and fear-inducing anymore. In contrast, the WG showed no significant changes in the SPQ scores or in the avoidance behavior. Furthermore, the affective ratings for the spider pictures did not show any significant change. Thus, consistent with previous studies [22, 23], CBT turned out to be an effective means to reduce affective and behavioral phobic symptoms in individuals suffering from spider phobia.
In order to identify the underlying neurobiological mechanisms of successful CBT, we contrasted the hemodynamic response changes from the first to the second session between the two patient groups. Relative to the WG, the TG patients displayed greater left medial orbitofrontal cortex (OFC) activation after successful therapy completion. This effect resulted from an increase of activation in the TG and a decrease in the WG. Interestingly, the main CBT effect occurred in a region implicated in emotion and emotion-related learning [20, 30]. The OFC is not only central for the rapid learning but also for the reversing of stimulus-reinforcement associations [26]. This is a key process in CBT where the patients are able to experience that contact with a spider does not involve catastrophic consequences, but is in fact innocuous.
A similar OFC function has been proposed by Johanson et al. (2006) in a recent PET study on the effects of cognitive therapy in spider phobia. Here, the patients were asked to explore and change their thoughts and misconceptions about the phobic object, but were not exposed to living spiders. The cognitive restructuring led to an increase in medial prefrontal cortex (PFC) activation in those patients who had been characterized by severe anxiety symptoms prior to the therapy. Since the medial PFC holds specific functions for cognitive and self-referential processes as well as emotion modulation, the authors propose that the increased cognitive control of the fear reaction provoked this localized augmentation in cerebral blood flow.
In line with this interpretation are the data for patient group (contrasts: Disgust > Phobia and Fear > Phobia). The phobics experienced the disorder-irrelevant conditions (Disgust, Fear) as aversive but more controllable than the Phobia condition, which was accompanied by a relative increase in medial OFC activation. Moreover, relative to the patients, the non-phobic subjects showed a greater involvement of the medial OFC and the adjacent ventral ACC during the first presentation of the spider pictures (contrast: Phobia > Neutral). Activation of the ventral ACC has been reported during various emotional states and manipulations. The ventral part is often referred to as ‘affective subdivision’ of the ACC and is (as the medial OFC) implicated in emotional regulation and control [3].
Altogether our data fit nicely with the concept of the medial OFC as a processor of stimulus valence and valence modulation. A similar idea has been put forward by LeDoux [17], who suggested that CBT should involve the medial PFC, since this region becomes relevant in extinction processes and during the development of new associations and implicit learning. However, according to LeDoux the therapy effect should not only be restricted to the prefrontal cortex, but also include the amygdala which receives inhibitory control by the medial PFC. Preliminary support for this assumption was found through the correlation analysis. Here, the reduction of somatic anxiety symptoms (e.g., experienced heart pounding, sweating) was positively associated with the reduction of amygdala and insular activation. This latter finding is in accordance with a previous fMRI therapy study [28], where the main treatment effect consisted of a normalization of insular hyperactivation.
However, our CBT study also clearly differs from the investigation by Straube et al. [28], e.g., with respect to the brain activation of the patients before therapy engagement, the applied symptom provocation method, and the chosen therapeutic approach. The phobic individuals studied by Straube et al. [28] showed no significant amygdala activation during the first exposure with spiders. This finding might be a consequence of habituation during the sustained stimulation. Previous fMRI studies have shown that phobic responses in the amygdala are strong but brief [16]. Habituation was probably slowed down by our design with short and alternating picture presentations (1.5 s per picture). Inconsistent with the interpretation is the fact that Straube et al. [28] observed greater amygdala activation in non-phobic relative to phobic subjects, which would imply a lack of habituation within the healthy group. This response pattern stands in sharp contrast with current models on the pathophysiology of specific phobia [18].
Additionally, we used static stimuli for symptom provocation, whereas Straube et al. [28] showed moving spiders. This might have led to the recruitment of different brain regions during exposure (e.g., attention-related areas such as the ACC).
Finally, despite the fact that in both investigations structured and comparable CBT manuals were employed, deviations in the particular therapeutic strategy cannot be ruled out. These differences might refer to the two main mechanisms of how CBT exert its effects; namely habituation of somatic arousal and cognitive restructuring [1]. Whereas in the present study the therapist focused on the correction of misattributions and thinking errors during the exposure, it is possible that the therapist of the other study directed the attention of the patients more towards the reduction of their somatic arousal.
This last point underlines that many important issues still need to be addressed in future brain-imaging investigations on how psychotherapy changes the brain of phobic patients. One of these issues refers to the specificity of therapy effects. Could similar brain activation changes be observed using different treatment methods? Furmark et al. [8] compared the neural effects of successful CBT and drug therapy (citalopram) in phobic patients. They found that regardless of the treatment approach improvement was accompanied by a decreased regional blood flow in the amygdala, which would point to a nonspecific therapy effect. The study of psychotherapy variations (e.g., habituation-focused vs. cognition-focused approaches) on neural activation also seems a promising approach to broaden the knowledge on the psychobiology of specific therapeutic interventions.
Further, it would be important to also study phobic subjects, who are not able to successfully complete CBT. Differences in OFC activation correlated with differences in therapy outcome could further elucidate the role of this brain region for emotional learning. Finally, the question with regard to the temporal stability of the altered OFC functioning should be addressed. Considering the long-lasting positive CBT effects on the behavioral and emotional dimension [23], this should also be reflected in a stable medial OFC involvement during recurrent exposure (e.g., in a follow-up session).
Conclusion
This controlled fMRI study on CBT effects indicated that successfully learned approach behavior and the correction of misattributions in spider phobics were accompanied primarily by functional changes of the medial OFC. This brain region plays an important role for the revising of stimulus-reinforcement associations and the cognitive control over fear responses.
References
Becker ES, Hoyer J (1995) Konfrontationsbehandlungen bei Spezifischen Phobien. In: Neudeck P, Wittchen H-U (Hrsg) Konfrontationstherapie bei psychischen Störungen. Hogrefe, Göttingen
Brett M, Penny W, Kiebel S (2004) An introduction to random field theory. In: Frackowiak RSJ, Friston K (ed) Human brain function, 2nd edn. Elsevier, Oxford
Davidson RJ, Pizzagalli D, Nitschke JB, Putnam K (2002) Depression: Perspectives from Affective Neuroscience. Annu Rev Psychol 53:545–74
Dilger S, Straube T, Mentzel HJ, Fitzek C, Reichenbach J, Hecht H, Krieschel S, Gutberlet I, Miltner W (2003) Brain activation to phobia-related pictures in spider phobic humans: an event-related functional magnetic resonance imaging study. Neurosci Lett 248:29–32
Fredrikson M, Annas P, Fischer G, Wik P (1996) Gender and age differences in the prevalence of specific fears and phobias. Behav Res Ther 34:33–39
Fredrikson M, Wik G, Annas P, Ericson K, Stone-Elander S (1995) Functional neuroanatomy of visually elicited simple phobic fear: Additional data and theoretical analysis. Psychophysiology 32:43–48
Fu CHY, McGuire PK (1999) Functional neuroanatomy in psychiatry. Philos Trans R Soc Lond Biol Sci 354:1359–1370
Furmark T, Tillfors M, Marteinsdottir I, Fischer H, Pissiota A, Langstrom B, Fredrikson M (2002). Common changes in cerebral blood flow in patients with social phobia treated with citalopram or cognitive-behavioral therapy. Arch Gen Psychiatry 59:425–433
Gabbard GO (2000) A neurobiologically informed perspective on psychotherapy. Br J Psychiatry 177:117–122
Globisch J, Hamm AO, Esteves F, Öhman A (1999) Fear appears fast: temporal course of startle reflex potentiation in animal fearful subjects. Psychophysiology 36:66–75
Goossens L, Schruers K, Peeters R, Griez E, Sunaert S (2007) Visual perception of phobic stimuli: amygdala activation via an extrageniculostriate pathway? Psychiatry Res Neuroimaging 155:113–120
Johanson A, Gustafson L, Passant U, Risberg J, Smith G, Warkentin S, Tucker D (1998) Brain function in spider phobia. Psychiatry Res Neuroimaging 84:101–111
Johanson A, Risberg J, Tucker DM, Gustafson L (2006) Changes in frontal lobe activity with cognitive therapy for spider phobia. Applied Neuropsychology 13:34–41
Klorman R, Weerts T, Hastings J, Melamed B, Lang P (1974) Psychometric description of some fear-specific questionnaires. Behav Res 5:401–409
Lang PJ, Bradley M, Cuthbert B (1997) International Affective Picture System. Center for Research in Psychophysiology, University of Florida Gainesville
Larson CL, Schaefer HS, Siegle GJ, Jackson CAB, Anderle MJ, Davidson RJ (2006) Fear is fast in phobic individuals: amygdala activation in response to fear-relevant stimuli. Biol Psychiatry 60:410–417
LeDoux J (2002) Synaptic self. How our brains become what we are. Penguin Books, London
Linden DEJ (2006) How psychotherapy changes the brain – the contribution of functional neuroimaging. Mol Psychiatry 11:528–538
Margraf J (1994) Diagnostisches Kurz-Interview bei psychischen Störungen, MiniDIPS. Springer-Verlag, Berlin
O’Doherty J (2001) Abstract reward and punishment representations in the human orbitofrontal cortex. Nat Neurosci 4:95–102
Miltner WH, Trippe RH, Krieschel S, Gutberlet I, Hecht H, Weiss T (2005) Event-related brain potentials and affective responses to threat in spider/snake-phobic and non-phobic subjects. Int J Psychophysiol 57:43–52
Öst LG (1996) One-session group treatment of spider phobia. Behav Res Ther 34:707–715
Öst LG, Ferebee I, Furmark T (1997) One-session group therapy of spider phobia: direct versus indirect treatments. Behav Res Ther 35:721–732
Paquette V, Lévesque J, Mensour B, Leroux JM, Beaudoin G, Bourgouin P, Beauregard M (2003) Change the mind and you change the brain: effects of cognitive behavioral therapy on the neural correlates of spider phobia. Neuroimage 18:401–409
Rauch SL, Savage CR, Alpert NM, Miguel EC, Baer L, Breiter HC (1995) A positron emission tomography study of simple phobic symptom provocation. Arch Gen Psychiatry 52:20–28
Rolls ET (1999) The brain and emotion. University press, Oxford
Schienle A, Schäfer A, Walter B, Stark R, Vaitl D (2005) Brain activation of spider phobics towards disorder-relevant, generally disgust- and fear-inducing pictures. Neurosci Lett 388:1–6
Straube T, Glauer M, Dilger S, Mentzel HJ, Miltner WHR (2006) Effects of cognitive-behavioral therapy on brain activation in specific phobia. Neuroimage 29:125–135
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, Mazoyer B, Joliot M. (2002) Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage 15:273–289
Ursu S, Carter CS (2005) Outcome representations, counterfactual comparisons and the human orbitofrontal cortex: implications for neuroimaging studies of decision-making. Cogn Brain Res 23:51–60
Walter B, Blecker C, Kirsch P, Sammer G, Schienle A, Stark R (2003) MARINA: An easy to use tool for the creation of MAsks for Region of INterest Analyses. Neuroimage 19: CD-ROM
Zald DH (2003) The human amygdala and the emotional evaluation of sensory stimuli. Brain Res Rev 41:88–123
Acknowledgements
This work was supported by a grant from the German Research Foundation to A.S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schienle, A., Schäfer, A., Hermann, A. et al. Symptom provocation and reduction in patients suffering from spider phobia. Eur Arch Psychiatry Clin Neurosc 257, 486–493 (2007). https://doi.org/10.1007/s00406-007-0754-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-007-0754-y