Abstract
Background
(Acetyl-)cholinesterase (ChE) inhibitors have been approved for the treatment of mild to moderate Alzheimer’s disease (AD). However, use of ChE inhibitors is limited by budget constraints and disincentives on the side of health insurances and nursing care insurances.
Objective
To analyse under what conditions the application of the acetylcholinesterase inhibitor donepezil is favourable for the treatment of patients with AD from the perspective of health insurance and nursing care insurance companies in Germany, taking into account factors such as start and duration of treatment, duration of follow-up, drug costs, internalization of opportunity costs and varying mortality and efficacy rates.
Methods
Transition probabilities from a Swedish study and German cost data for donepezil were merged in a Markov model to follow a cohort of patients over a period of 5–10 years. We defined a base case with 1 year treatment and follow-up over 5 years and varied treatment length, follow-up interval and cost factors in sensitivity analyses.
Results
In the base case, the ChE inhibitor donepezil did not lead to cost savings but to a cost-effective outcome on side of health insurances and nursing care insurances. Early treatment of AD and internalization of opportunity costs (caring time devoted to patients) led to less costs per quality adjusted life years gained. However, results are very sensitive with respect to varying mortality and efficacy rates.
Conclusion
The application of donepezil may be cost-effective, but considerable uncertainties remain. Moreover, the way the reimbursement system in Germany is presently arranged does not support the application of ChE inhibitors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The most prominent feature of Alzheimer’s disease (AD) is decline in patients’ cognitive function although other symptoms accompany the disease [18]. AD causes both direct costs such as medical treatment and institutionalization of the patient as well as unpaid costs caused by an extensive amount of time spent with patients by family members and other caregivers [29]. Both sources of costs are closely related to functional and behavioural impairment of daily living abilities [29, 31], which in turn is associated with the degree of cognitive decline.
Throughout Europe, including Russia, the number of patients with AD will rise from about 7.6 million at present to about 16.2 million in the year 2050 [34]. At the same time the number of persons at working-age will decline so that the financial burden imposed by dementia on the working-age population will markedly rise. Therefore, treatments that delay the time to institutionalization by way of slowing down the decline of cognitive and functional abilities are of high relevance not only to improve the quality of life of patients, but also to reduce health care costs and caregiver burden. Various (acetyl-)cholinesterase (ChE) inhibiting drugs such as donepezil [3], rivastigmine [2], or galantamine [16] have been evaluated in the past. A large number of double-blind placebo controlled trials involving several thousands of patients show that ChE inhibitors slow down cognitive decline, improve abilities of daily living and reduce care-giver burden [33]. Cost-effectiveness studies have applied different techniques such as Markov [13, 22, 32] or hazard models [11] to simulate the effect of ChE inhibitors on disease progression (for an overview see [4]). Results range from cost-savings to high additional costs through treatment.
Although the literature comprises a large variety of cost-effectiveness models, only few studies [28] examined the reimbursement structure that covers direct and indirect costs caused by AD. Moreover, previous cost-effectiveness studies focussed on the effect of short-term treatment. However, recently clinical studies provided data on effects of treatment over one year and longer [5, 19, 37]. Integration of long-term effects will markedly influence the cost-effectiveness of ChE treatment of mild to moderate AD since the delay of institutionalization is likely to become effective only after an extended period of disease progression that needs to be balanced against accumulated treatment costs. Treatment costs, in turn, depend on treatment related alterations of mortality. Most substantial cost savings are realized if patients’ survival probability does not depend on disease stage: it pays to keep patients in less severe stages. There is some evidence, however, that ChE inhibitor treatment may reduce mortality in patients with moderate to severe stages of AD [7], although data are not conclusive [8].
Thus, in the current study, we set out a cost-effectiveness model for the long-term effects of treatment with donepezil, taking into account multiple types of costs associated with AD and varying mortality scenarios. We considered the impact of the specific organization of the reimbursement system in Germany, with a differentiation between health and nursing care insurances, on the estimates of cost-effectiveness.
Methods and data
Framework
Cost-effectiveness analysis calculates the ratio of incremental costs and effects of an intervention compared to an alternative [9]. A positive incremental cost-effectiveness ratio usually implies that higher intervention costs go along with an increase in outcome measures such as life expectancy or health-related quality of life. An intervention is cost saving if it achieves an improvement in outcome measures with costs unchanged or even lower.
The model
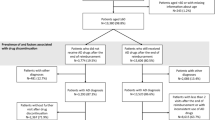
We applied a state-transition (Markov) model to simulate the progression of the severity of AD through the course of the disease. The classic Markov assumption is that the process has no memory of prior states, i.e. all AD patients in a given state have the same prognosis, independently of how they got to the present state [14]. Disease progression was modelled through iteration of transition probabilities for multiple cycles. We adopted estimates of transition probabilities and severity specific mortality rates from a Swedish population-based study that followed a group of elderly people for more than 4 years (the Kungsholmen project) [13] (see Fig 1).
One year transition probabilities of placebo treatment based on Jönsson et al. [13]
Patients were classified into one of four disease stages according to the MMSE score, which ranges between 0 and 30. Two treatment scenarios were compared: placebo, and donepezil with 10 mg dose. State transitions were estimated in cycles of a yearFootnote 1. The model ran 5 cycles to compare results with other cost-effectiveness studies. Additionally, we increased the time span up to 10 years (cycles) to investigate long-term effects since median survival of AD patients after symptom onset has been estimated at about 11 years from onset of symptoms and 6–7 years from diagnosis [6, 35].
Efficacy of Donepezil and mortality
Three multicenter doubleblind trials have examined the efficacy of Donepezil [5, 19, 37] over a period of 1 year and longer. Over one year treatment, the risk reducing effect of Donepezil treatment was 70% in a study by Winblad et al. [37] using MMSE score as measure of cognitive decline, and 38% in a study by Mohs et al. [19] using MMSE score, the AD Functional Assessment and Change Scale and the Clinical Dementia Rating Scale. The only study assessing effects of Donepezil treatment after three years found only small, non-significant effects [5]. We applied the estimates by Mohs et al. [19] as an intermediate starting point, varying the effectiveness estimates in sensitivity analysis. Transition probabilities to progress to worse stages of AD were reduced by the efficacy probability (in the base case with Mohs et al. study by 38% for example) to model efficacy. It was assumed that only patients in the mild to moderate stages received treatment with Donepezil since the vast majority of clinical trials on ChE inhibitors studied patients in mild to moderate stages of AD. One year treatment length constituted our base case to be in line with the trial length.
The mortality issue is a source of much controversy [7, 8]: an equally substantial gain in outcome and life expectancy through treatment means that the patient will experience basically the same course of disease, only with a time lag. Nursing care needs to be supplied to the same extent, only later. To highlight this aspect, we varied mortality in two ways: Firstly, it was assumed that treatment reduced mortality up to 20% in the treated cohort. Secondly, differences in mortality with respect to severity of AD were varied by multiplying the mortality rate of the mildly affected AD patients with a factor and the mortality rate of moderately and severely affected with its reciprocal value (for example a factor 0.5 for the mortality of the mildly affected patients means a doubling (1/0.5) of the mortality in the more severely affected patient group and vice versa). This factor was varied between 0.7 and 1.3. Transition probabilities for survival were adjusted proportionately in both cases.
Health-state valuation
Health-related quality of life was estimated as a function of disease severity [20, 23, 24] based on the information from the Health Utilities Index Mark II (HUI:2) [23] provided by caregivers. We used the HUI:2 scores for mild (0.69), moderate (0.53), severe (0.38) and profound (0.27) dementia. Quality-adjusted life years (QALYs) were computed by multiplying the utility score by cycle length (1 year). For sensitivity analysis, the utility range was varied to account for possible inadequacies in the fit of the original and MMSE-based classification of stages of disease. We stretched the range of the scale by multiplying utility differences with a common factor between 1 and 1.4 in sensitivity analysis. In addition, we investigated life years gained in the base case.
Initial severity distribution
Since the disease severity at the beginning of the ChE treatment is important for the efficacy, we estimated the cost-effectiveness for a range of initial disease severities. The distribution of disease severity was estimated on the basis of the MMSE scores of AD patients included in the database established at the Alzheimer Memorial Center of the Maximilian University of Munich with a total of 570 patients examined since 1998 (see Appendix Table A-1).
Estimation of costs
Estimates of costs for paid and unpaid care giving as well as direct medical and non-medical costs without Donepezil were obtained from estimates based upon a survey of 1682 German AD patients [10]. Our base year is 2004. Cost data were adjusted for price trends since 1998 (+1.4% per year [30]). Since the costs of care giving are typically only partially remunerated, we assumed costs equal to € 5 per hour as opportunity costs in sensitivity analysis. This amount accounts for received lump sum payments and is comparable to typical payments to unskilled employees. The number of hours a caregiver devotes to a patient ranges from no time at all devoted to mildly affected patients per day to the mean of 13.94 h/day for patients with a MMSE score of less than 10. Further financial details are given in Table 1. Patients in more severe stages are more likely to need inpatient care (see Appendix Table A-1: Institutionalization) the cost of which is basically covered by nursing care insurances (InCare). Direct outpatient costs (OutCare) are shared by three cost units—nursing care insurance, health insurance and families—while indirect costs in form of time devoted to care are exclusively covered by families.
The degree of institutionalization determines the extent of inpatient and outpatient care required. The severity dependent degree of institutionalization was derived from Hux et al. [12]. Since these data derive from Canada, we performed sensitivity analysis by subtracting a common absolute percentage value for all severity groups to reflect a broader range of degrees of institutionalization in different western countries. The upper bound was the degree of institutionalization in the mild-moderate group (15.5%). Costs per year, severity grade, and patient were calculated according to the formula in Appendix Table A-1.
Prices of Donepezil were taken from the German drug register [1]: drug costs for 10 mg donepezil are about € 5—per day and patient. Sensitivity analysis covered price reductions up to 60%. Placebo probabilities were associated with no drug treatment and thus zero costs. The treatment was taken as an adjunct rather than a substitute to other medication.
Discount rate
The discount rate is supposed to express preferences for time, i.e. the stronger weighing of future relative to current costs. If costs and outcomes are accumulated over time, cost figures need to be devalued by a constant discount rate, which was subject to alteration in sensitivity analysis. The base case was 5% per year [27]. Variations covered the range between 0 and 10% per year. Half-cycle corrections were calculated since the software (TreeAge Software Inc., Williamstown, USA) calculates costs of treatment and gains in QALYs either at the beginning or the end of the cycle, thus ignoring constant utilization. An overview of the base case is given in Appendix Formula A-1.
Results
Base case (Table 2)
For the base case, treatment with donepezil is not cost saving when compared to placebo (Table 2). Savings in inpatient care only partly offset medication costs. In addition, the number of QALYs increases by 4.1% adding up to € 4,264 per QALY gained. The ratio considering life years is similar with about € 5,000 per life year gained.
Sensitivity analysis (Table 3)
In our model, donepezil is cost saving if care giving is better paid than € 4.20 per hour. Similar, if the cost of inpatient care rises by more than 30% or the drug price is reduced to about 35% of its actual price, the application of donepezil is cost saving. Results are very sensitive regarding to the assumed efficacy of donepezil and its effect on mortality. If donepezil reduces disease progression only by 20% over a year, the incremental cost-effectiveness ratio is € 16,726 per QALY gained, while a 54% reduction of disease progression turns donepezil into a cost saving alternative.
Variation of the remaining variables influences the incremental cost-effectiveness ratio but does not lead to a cost saving scenario: If treatment reduces mortality by about 20% the incremental cost-effectiveness ratio raises to € 14,875 per QALY gained. In addition, the ratio increases if differences in mortality between mildly and severely affected patients become more pronounced. Increase in duration of treatment raises the incremental cost-effectiveness ratio to € 13,169 per QALY for 3 years of treatment. Duration of follow-up shows a U-shaped course with decrease of the incremental cost-effectiveness ratio between 1 and 5 years of follow-up and an increase between 5 and 10 years of follow-up. The earlier treatment starts, i.e. the higher the probability of being mildly affected at beginning of treatment, the less has to be paid for a QALY gained. Reductions in inpatient care influence the results only marginally.
Additional remuneration payments of € 5 per hour care giving (last column in Table 3) lower the cost-effectiveness ratio: For example, in the presence of this remuneration early treatment (by way of early diagnosis) leads to a cost saving outcome. In this case, already an efficacy of 35% reduction of disease progression would make donepezil the dominant treatment.
Discussion
The main results of the current study show that the treatment of AD with donepezil leads not to a saving of costs, but still a cost-effective outcome is achieved even if only direct costs are considered. Incremental cost-effectiveness ratios become increasingly advantageous under two conditions: First, remunerations to caregivers are increased. Second, treatment starts early in the course of the disease. However, results are sensitive to efficacy of treatment and treatment-related mortality.
Our results lie within the wide range of earlier studies. While Jönsson et al. [13] and O’Brian et al. [25] found donepezil to be cost saving from a health-care system perspective, Neumann et al. [22] estimate incremental costs per QALY up to $ 76,000, even from a societal perspective. The National Institute of Clinical Excellence (NICE) in England proposed to withdraw ChE inhibitors since their estimates add up to £ 48,000 [15]. The AD2000 study did not detect benefits above minimally relevant thresholds, however, long-term results were based on low numbers of patients due to high drop-outs of patients opting for open-label treatment [5]. A case-control study from a US cohort between 1999 and 2001 suggests that donepezil use was associated with significantly lower medical costs [17]. However, it was not assessed whether parameters of socio-economic status, education and premorbid intelligence level had an influence on these effects (as in 1999 donepezil user might have come from a higher socio-economic background than non-users).
Our data suggest that length of treatment increases the incremental cost-effectiveness ratio. This reflects the observation that the clinical effect of treatment with ChE inhibitors decreases over time, possibly related to the progressive degeneration of cortical input neurons of cholinergic projections. The cost-effectiveness ratio showed a U-shaped association with duration of follow-up, with minimum costs per QALY somewhere near five years of follow-up. Shorter follow-up intervals may compromise the detection of treatment-related decrease of transition in more severe stages of disease. In contrast, longer follow-up intervals are likely to increase the effect of an implicit decrease of mortality by treatment, because more severe stages of disease bear a higher risk of death, but are reached later with effective treatment.
Mortality rates derived from clinical trials represent the lower limit of mortality rates in the population because patients that participate in clinical trials are typically healthier than the general population. Because there are no decisive data on effects of cholinergic treatment on mortality in AD, we used sensitivity analysis with representative estimates from population-based data to more closely reflect population-wide variations in mortality. Assumptions on mortality are a pivotal factor in the analysis of cost-effectiveness: to keep patients in less severe stages, in which they die with the same probability as in the more severe stages, produces cost savings. This connection is even stronger if patients start treatment in an early stage of AD. Furthermore, the drug is taken as an adjunct rather than a replacement of conventional treatments. In case of replacement, a cost saving outcome becomes more likely.
We performed sensitivity analysis considering effects of treatment on progression to more severe stages of dementia. Estimates from clinical trials based on selected populations and obtained under ideal circumstances most likely overestimate effects. We therefore chose to use sensitivity analysis with rates of efficacy ranging between a low estimate of 20%, a moderate estimate based on one long-term clinical trial of 40% [19] and a high estimate based on another long-term clinical trial of 60% [37]. High rates of efficacy render Donepezil the cost saving alternative. There is one double-blind placebo controlled study on the effects of Donepezil over 3 years of treatment [5]. This study showed effect sizes comparable to previous clinical trials within the fist half year of the study. Subsequently, effect sizes became much lower. The great advantage of this study is the use of a routine clinical setting for follow-up. Unfortunately, interpretation of these data is compromised by the unclear selection criteria, the repeated withdrawal periods and the systematic attrition of sample size due to changes in drug availability during the trial period.
The development of health care costs in the future can induce an incentive to apply donepezil. Thus, donepezil as an exemplary ChE inhibitor bears the potential to be economically attractive despite high acquisition costs. Similar results can be expected for other ChE inhibitors given recent studies on efficacy and cost-effectiveness. Decrease of drug costs by about 40% renders donepezil treatment the cost saving alternative. Availability of generic formulations in the future may make price reductions possible to some extent. Adding a remuneration of € 5 per hour care giving renders early treatment with donepezil the cost-saving alternative. Patient care by family members is real work that has to be provided by somebody. If care is provided by formal services, in Germany there are fixed budgets for different types of services. The same type of care provided by family members has no formal budget. However, nursing care insurances in Germany pay a certain amount of money for caring for patients living in the community if the care is not provided by formal services but by family members. The money amounts to 250.-€ per months for a patient with mild to moderate dementia and some extent of somatic comorbidity (for example urinary incontinence). Assuming a very low estimate of 2 h care per day in these stages of dementia this would amount to 5.-€ per hour. Use of imputed values for unpaid informal care has a long tradition in pharmaco-economy [26]. Presently, 50 % (in mild dementia) to 75% (in severe dementia) of costs of care are covered by families in Germany [10]. With the increasing numbers of elderly people without close relatives in the next two decades in Germany and other industrialized countries, these imputed costs of informal care will become real costs of formal care that will have to be covered by the health system. Another important socio-economic factor is loss of income of care-givers dedicating their time to the patient resulting in decrease of productivity for the economy. This will also lead to reduced funds for health and nursing care insurances, but to our knowledge there are no data and models available to quantify this effect.
Uncertainties surrounding parameter values demand further research considering mortality, efficacy, diagnostic accuracy and health-related quality of life with AD. These uncertainties do not allow a general statement about the cost-effectiveness of donepezil beyond our model specifications.
For the interpretation of the results one has to consider two further caveats. First, data on costs, health-related quality of life and transition probabilities were drawn from different sources merging clinical and quality data from the US, population-based data from Sweden, and cost figures from Germany. In addition, clinical data provide evidence of efficacy, not effectiveness. However, the sensitivity analyses gave no indication that the results are substantially biased. Second, the population-based data from Sweden on transition probabilities are based on a cohort of people older than 75 years. Participants are thus substantially older than patients in clinical trials. Based on the CERAD data, the transition probabilities from mild to moderate and moderate to severe stages were not different between age groups from below 65 years of age, between 65 and 74 years of age and above 75 years of age [21]. Mortality rates, however, were higher in older subjects. A lower mortality rate (independent of treatment) in younger subjects may lead to higher incremental costs per QALY due to longer survival in more advanced stages.
It is noteworthy that under the specific conditions of the reimbursement system in Germany the cost of the drug will mainly affect the budget of health insurances while the benefits affect nursing care insurances. Screening of at risk subjects (allowing early intervention) or higher compensation payments to family members may foster a favourable, societal outcome. A last note of caution seems important. Cost-efficacy analysis is an important tool to inform decision makers on potential socio-economic consequences of the allocation of resources to certain treatments. It contributes to an informed and rational selection of and among treatment options, but it does not exempt decision makers or the public from an ethical discourse on the allocation of resources within a limited budget.
Notes
The structure of the model in DATA PRO is available upon request
References
(2003/II) Rote Liste®. Editio Cantor Verlag für Medizin und Naturwissenschaften GmbH, Aulendorf
Birks J, Iakovidou V, Tsolaki M (2000) Rivastigmine for Alzheimer’s disease. Cochrane Database Syst Rev: CD001191
Birks JS, Harvey R (2003) Donepezil for dementia due to Alzheimer’s disease. Cochrane Database Syst Rev: CD001190
Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, Waugh N (2002) Clinical and cost-effectiveness of donepezil, rivastigmine, and galantamine for Alzheimer’s disease. A systematic review. Int J Technol Assess Health Care 18: 497–507
Courtney C, Farrell D, Gray R, Hills R, Lynch L, Sellwood E, Edwards S, Hardyman W, Raftery J, Crome P, Lendon C, Shaw H, Bentham P (2004) Long-term donepezil treatment in 565 patients with Alzheimer’s disease (AD2000): randomised double-blind trial. Lancet 363: 2105–2115
Fitzpatrick AL, Kuller LH, Lopez OL, Kawas CH, Jagust W (2005) Survival following dementia onset: Alzheimer’s disease and vascular dementia. J Neurol Sci 229–230: 43–49
Gasper MC, Ott BR, Lapane KL (2005) Is donepezil therapy associated with reduced mortality in nursing home residents with dementia? Am J Geriatr Pharmacother 3: 1–7
Geldmacher DS, Provenzano G, McRae T, Mastey V, Ieni JR (2003) Donepezil is associated with delayed nursing home placement in patients with Alzheimer’s disease. J Am Geriatr Soc 51: 937–944
Gold MR, Siegel JE, Russell LB, M.C. W (1996) Cost-effectiveness in Health and Medicine. Oxford University Press, New York
Hallauer JF, Schons M, Smala A, Berger K (2000) Costs of medical treatment of Alzheimer patients in Germany. Gesundheitsökonomie & Qualitätsmanagement 5: 73–79
Hauber AB, Gnanasakthy A, Mauskopf JA (2000) Savings in the cost of caring for patients with Alzheimer’s disease in Canada: an analysis of treatment with rivastigmine. Clin Ther 22: 439–451
Hux MJ, O’Brien BJ, Iskedjian M, Goeree R, Gagnon M, Gauthier S (1998) Relation between severity of Alzheimer’s disease and costs of caring. Cmaj 159: 457–465
Jönsson L, Lindgren P, Wimo A, Jonsson B, Winblad B (1999) The cost-effectiveness of donepezil therapy in Swedish patients with Alzheimer’s disease: a Markov model. Clin Ther 21: 1230–1240
Kemeny JG, Snell JL (1976) Finite Markov chains. Springer, New York
Kmietowicz Z (2005) NICE proposes to withdraw Alzheimer’s drugs from NHS. BMJ 330: 495
Loy C, Schneider L (2004) Galantamine for Alzheimer’s disease. Cochrane Database Syst Rev: CD001747
Lu S, Hill J, Fillit H (2005) Impact of donepezil use in routine clinical practice on health care costs in patients with Alzheimer’s disease and related dementias enrolled in a large medicare managed care plan: a case-control study. Am J Geriatr Pharmacother 3: 92–102
Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S (2002) Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. Jama 288: 1475–1483
Mohs RC, Doody RS, Morris JC, Ieni JR, Rogers SL, Perdomo CA, Pratt RD (2001) A 1-year, placebo-controlled preservation of function survival study of donepezil in AD patients. Neurology 57: 481–488
Neumann PJ (2005) Health utilities in Alzheimer’s disease and implications for cost-effectiveness analysis. Pharmacoeconomics 23: 537–541
Neumann PJ, Araki SS, Arcelus A, Longo A, Papadopoulos G, Kosik KS, Kuntz KM, Bhattacharjya A (2001) Measuring Alzheimer’s disease progression with transition probabilities: estimates from CERAD. Neurology 57: 957–964
Neumann PJ, Hermann RC, Kuntz KM, Araki SS, Duff SB, Leon J, Berenbaum PA, Goldman PA, Williams LW, Weinstein MC (1999) Cost-effectiveness of donepezil in the treatment of mild or moderate Alzheimer’s disease. Neurology 52: 1138–1145
Neumann PJ, Kuntz KM, Leon J, Araki SS, Hermann RC, Hsu MA, Weinstein MC (1999) Health utilities in Alzheimer’s disease: a cross-sectional study of patients and caregivers. Med Care 37: 27–32
Novella JL, Jochum C, Jolly D, Morrone I, Ankri J, Bureau F, Blanchard F (2001) Agreement between patients’ and proxies’ reports of quality of life in Alzheimer’s disease. Qual Life Res 10: 443–452
O’Brien BJ, Goeree R, Hux M, Iskedjian M, Blackhouse G, Gagnon M, Gauthier S (1999) Economic evaluation of donepezil for the treatment of Alzheimer’s disease in Canada. J.Am Geriatr Soc 47: 570–578
Rice DP, Fox PJ, Max W, Webber PA, Lindeman DA, Hauck WW, Segura E (1993) The economic burden of Alzheimer’s disease care. Health Aff (Millwood) 12: 164–176
Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT, Group tDS (1998) A 24-week, double-blind, placebo-contolled trial of donepezil in patients with Alzheimer’s disease. Neurology 50: 136–145
Ruof J, Mittendorf T, Pirk O, von der Schulenburg JM (2002) Diffusion of innovations: treatment of Alzheimer’s disease in Germany. Health Policy 60: 59–66
Small GW, McDonnell DD, Brooks RL, Papadopoulos G (2002) The impact of symptom severity on the cost of Alzheimer’s disease. J Am Geriatr Soc 50: 321–327
Statistik Bf (2004) Statistisches Jahrbuch. Metzler-Poeschel, Stuttgart
Steele C, Rovner B, Chase GA, Folstein M (1990) Psychiatric symptoms and nursing home placement of patients with Alzheimer’s disease. Am J Psychiatry 147: 1049–1051
Stewart A, Phillips R, Dempsey G (1998) Pharmacotherapy for people with Alzheimer’s disease: a Markov-cycle evaluation of five years’ therapy using donepezil. Int J Geriatr Psychiatry 13: 445–453
Thompson S, Lanctot KL, Herrmann N (2004) The benefits and risks associated with cholinesterase inhibitor therapy in Alzheimer’s disease. Expert Opin Drug Saf 3: 425–440
Wancata J, Musalek M, Alexandrowicz R, Krautgartner M (2003) Number of dementia sufferers in Europe between the years 2000 and 2050. Eur Psychiatry 18: 306–313
Waring SC, Doody RS, Pavlik VN, Massman PJ, Chan W (2005) Survival among patients with dementia from a large multi-ethnic population. Alzheimer Dis Assoc Disord 19: 178–183
Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB (1996) Recommendations of the panel on cost-effectiveness in health and medicine. Jama 276: 1253–1258
Winblad B, Engedal K, Soininen H, Verhey F, Waldemar G, Wimo A, Wetterholm AL, Zhang R, Haglund A, Subbiah P (2001) A 1-year, randomized, placebo-controlled study of donepezil in patients with mild to moderate AD. Neurology 57: 489–495
Acknowledgement
We thank Johannes F. Hallauer of the Charité University Hospital and Peter J. Neumann of the Harvard Center for Risk Analysis for helpful comments. Financial support for this study was provided by the German Centre of Gerontology, Office of the Committee of Experts to the 4th Report on the Elderly, Manfred-von-Richthofen-Str.2, 12101 Berlin, Germany, to M.H. There are no competing interests.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Formula A-1: Cost calculations for different severity grades of Alzheimer disease.
Cost[i] = DrugCost + InCare[i] × InstGrad[i] + [OutCare[i] + FamCare[i] × Remuneration] × [1 − InstGrad[i]]
-
DrugCost = Acquisition costs of donepezil within a year of therapy
-
[i] = Severity grade
-
InCare [i] = Direct inpatient costs within a year with respect to severity [i]
-
OutCare[i] = Direct outpatient costs within a year with respect to severity [i]
-
Fam Care [I] = Time devoted to care by families within a year
-
Remuneration = Hypothetical wage rate for care
-
InstGrad [i] = Degree of institutionalization with respect to severity [i]
Rights and permissions
About this article
Cite this article
Teipel, S.J., Ewers, M., Reisig, V. et al. Long-term cost-effectiveness of donepezil for the treatment of Alzheimer’s disease. Eur Arch Psychiatry Clin Neurosc 257, 330–336 (2007). https://doi.org/10.1007/s00406-007-0727-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-007-0727-1