Abstract
Objectives
We investigated the relationship between Onodi cells and optic canal by paranasal sinus computed tomography (PNSCT).
Methods
In this retrospective study, 508 PNSCT (265 males and 243 females) was examined. Onodi cell presence, pneumatization types, optic canal types; and also sphenoid sinusitis and anterior clinoid process pneumatization were evaluated.
Results
The prevalence of Onodi cells was 21.2% of the patients. Onodi cells were observed 40.7% on the right side and 25.9% on the left side. In 33.4% of the patients, bilateral Onodi cells were present. Male/Female ratio was 24.5%/17.6%. Onodi cell types were detected as Type I > Type II > Type III bilaterally. There was a positive correlation between the right and left Onodi cell types (p < 0.05). Optic canal types were detected as Type IV > Type I > Type II > Type III. bilaterally. There was a positive correlation between right and left optic canal types. Onodi cell presence and ACP pneumatization were found as statistically significant (p < 0.05). In 65.5% of the patients, Onodi cells and ACP pneumatization were absent. ACP pneumatization was present in 35.4% of the cases. In nine cases, bilateral Onodi cells and ACP pneumatization were detected. Sphenoid sinusitis was detected in 11.4% of Type I and 13.8% of the Type II Onodi cells on the right side. On the left side, it was detected in 12.9% of the Type I and 19.0% of Type II Onodi cells.
Conclusion
Identification of Onodi cell is very important clinically because of its proximity to optic nerve canal. We concluded that type IV Onodi–optic canal relationship was the most common finding in our study. Onodi cell presence and their patterns of pneumatization must be evaluated on PNSCT preoperatively to avoid optic canal damage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Onodi cell (OC) or sphenoethmoidal air cell is a posterior‑most ethmoidal air cell that pneumatized either superolateral, superior or lateral to sphenoid sinus [1]. Embryologically, sphenoid bone ossifies from the lower chondral ossification center and the upper ossification center merging with that of ethmoid [2].
Posterior ethmoid cells extend beyond the ethmoid bone to the sphenoid bone superolaterally and surround the optic channel that simulates the Onodi cell in most cases. Surgical approach will change once the Onodi cell is identified and it may extend to the anterior surface of the sphenoid sinus up to 1.5 cm. The inferomedial floor of sphenoid sinus is the preferred route to enter Onodi cell so as to prevent any damage to the optic nerve [3].
Özturan et al. [4] reported that coexistence of OC could alter the morphological changes in the floor and/or lateral wall of the sphenoid sinus. In addition, it is stated that OC has poor ventilation and ineffective drainage. It causes stasis of secretions, infections, optic neuropathies, optic neuritis or mucoceles [5,6,7].
In the present study, we investigated the relationship between Onodi cells and optic canal. Onodi cell pneumatization types, optic canal types and also sphenoid sinusitis and anterior clinoid process pneumatization were evaluated. The evaluation was performed by multi-slice computed tomography (MSCT) of the paranasal sinuses (PNSCT).
Materials and methods
This retrospective study was conducted in Kırıkkale University Faculty of Medicine, Departments of Radiology and Otolaryngology, according to the principles of Declaration of Helsinki. Ethics Committee approval was taken from Kırıkkale University Non-invasive Research Ethics Committee (Date: 24.10.2018, Number: 2018.10.15).
Subjects
Paranasal sinus computed tomography (PNSCT) images (Multi-slice CT-MSCT) were obtained from the digital archive of the Kırıkkale University Faculty of Medicine Radiology Department between December 2017 and June 2018. PNSCT images of 508 patients (265 males and 243 females) between 18 and 75 years were evaluated. Mean of the ages were 34.1 ± 14.3 years.
The reason for performing the PNSCT was chronic sinusitis, nasal obstruction and headache.
Patients under the age of 18 years and older than 75 years, patients with nasal polyposis, patients who have had surgery or have a history of trauma from the sinonasal region, and patients with benign or malignant tumors were excluded from the study.
CT imaging and analysis
All of the scans were obtained with routine PNS computed tomography imaging in the supine position, with no contrast or sedation being used for the procedures. The images were acquired using a 64-slice CT (MSCT; Brilliance 64, Philips Medical System, Best, the Netherlands). All of the scans were obtained using the following parameters: tube voltage 120 kV, effective mAs 350, slice thickness 1.00 mm, field of view (FOV) 180 mm, and image matrix 768 × 768. The images were transferred to a commercially available workstation, and the raw data were reconstructed using bone algorithms. After scanning, the coronal, axial, and sagittal images were reconstructed with a slice thickness of 1.00 mm. The coronal and axial plan was often preferred. All of the cases included in the study were evaluated by the same radiology expert (AÖ).
The following measurements were performed:
-
1.
Onodi cells Onodi cell or sphenoethmoidal air cell is a posterior-most ethmoidal air cell that pneumatized either superolateral, superior or lateral to sphenoid sinus [1]. The presence of the Onodi cells was evaluated as absent or present (right, left or bilateral).
-
2.
The pneumatization of the anterior clinoid process (ACP): ACP pneumatization was evaluated as absent, or present (right, left or bilateral).
-
3.
The pneumatizations of the Onodi cells were evaluated according to the study of Thimmaiah et al. [3]: a horizontal line was drawn at the uppermost part of sphenoid sinus in the coronal reformatted image at a plane where maximum size of Onodi cell was seen in contact with bony sphenoid sinus. If the cell was seen above and medial to sphenoid sinus, then it was labeled as Type I pattern of pneumatization, Type II if the air cell was seen both above and below the horizontal line and Type III if it was seen below the horizontal line, (Figs. 1, 2 and 3).
-
4.
The relationship of the optic canal and Onodi cells: The optic canal and the Onodi cell often show close proximity. The relationship between these two structures was evaluated as stated in the study of Chmielik and Chmielik [8, 9].
Type I “There was no contact between the wall of the ethmoid cell and optic nerve canal” [8, 9] (Fig. 4).
a On coronal PNSCT, Onodi cell (*) is shown, b on sagittal PNSCT, Onodi cell (*), sphenoid sinus (S) and optic canal (white arrow) (type 1) are shown. There was no contact between the wall of the Onodi cell and optic nerve canal, c on axial PNSCT, Onodi cell (*), sphenoid sinus (s) and optic canal (white arrow) are shown
Type II “The wall of the ethmoid cell was adjacent to the optic nerve canal wall on the distance maximum 2 mm (measuring in axial and sagittal planes) not extending laterally or superolaterally” [8, 9] (Fig. 5).
a On coronal PNSCT, Onodi cell (*) is shown, b on sagittal PNSCT, Onodi cell (*) and optic canal (white arrow) (type II) are shown. The wall of the Onodi cell was adjacent to the optic nerve canal wall on the distance maximum 2 mm (measuring in axial and sagittal planes) not extending laterally or superolaterally, c on axial PNSCT, Onodi cell (*) and optic canal (white arrow) are shown
Type III “The wall of the ethmoid cell was adjacent to the optic nerve canal wall within distance > 2 mm in the axial and/or sagittal plane extending laterally or supero-laterally without bulging of the optic nerve canal into the ethmoid bone” [8, 9] (Fig. 6).
a On coronal PNSCT, Onodi cell (*) and optic canal (white arrow) are shown, b on sagittal PNSCT, Onodi cell (*) and optic canal (white arrow) (type III) are shown. The wall of the Onodi cell was adjacent to the optic nerve canal wall within distance > 2 mm in the axial and/or sagittal plane extending laterally or supero-laterally without bulging of the optic nerve canal into the ethmoid bone, c on axial PNSCT, Onodi cell (*) and optic canal (white arrow) are shown
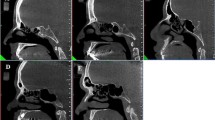
Type IV “The wall of the ethmoid cell was adjacent to the optic nerve canal-wall for a distance of more than 5 mm (measuring in the axial or sagittal plane) extending supero-laterally with bulging. The bulging was defined as the protrusion of the optic nerve into the ethmoid cell visualized in two planes. The very thin slice thickness guaranteed not missing any bulging of the optic nerve canal”. [8, 9] (Fig. 7).
a On coronal PNSCT, Onodi cell (*), sphenoid sinus (S), optic canal (white arrow) and anterior clinoid process pneumatization (A) are shown, b on sagittal PNSCT, Onodi cell (*), optic canal (white arrow) (type IV) and anterior clinoid process pneumatization (A) are shown. The wall of the Onodi cell was adjacent to the optic nerve canal wall for a distance of more than 5 mm (measuring in the axial or sagittal plane) extending supero-laterally with bulging. The bulging was defined as the protrusion of the optic nerve into the ethmoid cell visualized in two planes, c on axial PNSCT, Onodi cell (*), optic canal (white arrow) and anterior clinoid process pneumatization (A) are shown
-
5.
Sphenoid sinusitis: In our study, the relationship between sphenoid sinusitis (sphenoiditis) and Onodi cell was also evaluated. In our study, sphenoid sinusitis was accepted as a mucosal thickening greater than 2 mm as described by Gliklich and Metson [10].
Statistical analysis
SPSS for Windows 16.0 (SPSS, INC, an IBM Company, Chicago, Illinois). McNemar-Bowker test, Chi-square test and Spearman’s correlation rho efficient test were used.
p < 0.05 was considered as statistically significant.
Results
In our study, we detected Onodi cells in 108 of the patients (21.2%). Onodi cells were observed on the right side in 44/108 patients (40.7%), on the left side 28/108 patients (25.9%) and in 36/108 patients, bilateral Onodi cells were present (33.4%) (Table 1). In the male group, Onodi cells were detected in 65 (24.5%)patients: 26 (9.8%) right, 19 (7.2.%) left and 20 (7.5%) bilateral. In the females, Onodi cells were detected in 43 (17.6%) patients: 18 (7.4%) right, 9 (3.7.%) left and 16 (6.6%) bilateral.
The difference between Onodi cell presence and ACP pneumatization was found as statistically significant (p = 0.000). In 262 patients (65.5%), Onodi cells and ACP pneumatization were absent. ACP pneumatization was present in 177/500 cases (35.4%). In nine cases, bilateral Onodi cells and ACP pneumatization were detected (Table 1).
The relationship between Onodi cell types and Optic canal was shown for the right and left sides on Table 2. On the right side, Onodi cell types were detected as Type I (43.8%), Type II (36.2%) and Type III (20.0%). Right optic canal types were detected as Type IV (35%), Type I (25%), Type II (25%) and Type III (15%) (p > 0.05). On the left side, Onodi cell types were detected as Type I (48.4%), Type II (32.8%) and Type III (18.8%). Left optic canal types were detected as Type IV (34.4%), Type I (28.1%), Type II (23.4%) and Type III (14.1%) (p > 0.05) (Table 2).
The relationship between Onodi cell types and sphenoid sinusitis was shown in Table 3. On the right side, sphenoid sinusitis was detected in 11.4% of the Type I Onodi cells and 13.8% of the Type II Onodi cells (p > 0.05). On the left side, sphenoid sinusitis was detected in 12.9% of the Type I Onodi cells and 19.0% of the Type II Onodi cells (p > 0.05).
Spearman’s correlation rho efficient test results showed that there was a positive correlation between right and left sphenoid sinusitis (p = 0.000, r = 0.520), right and left Onodi cell types (p = 0.000, r = 0.466) and right and left optic canal types (p = 0.010, r = 0.424). There were no correlations between age, gender, and Onodi cell types and optic canal types (p > 0.05).
Discussion
During endoscopic procedures, the OC may be confused with the sphenoid sinus [11]. If present, Onodi cell has to be detected preoperatively because of its proximity to optic nerve and internal carotid artery canal so as to avoid injury during sinus surgeries [3]. The Onodi cell has to be differentiated from overriding posterior ethmoid cell because of their anatomical resemblance and both being closely related to optic nerve canal [12].
To avoid potential complications in endoscopic sinus surgery it is necessary to evaluate CT scans preoperatively [13], specially to identify bulging of the optic canal into a sphenoethmoidal cell [9].
In the literature, studies were mainly based on one CT plane: axial or coronal. Onodi cell prevalence was found to be higher when the CT examinations were evaluated in two planes [14, 15], whereas in our study, the evaluation of the Onodi cells was performed on the three planes: coronal, axial and sagittal. Therefore, we evaluated OCs more precisely.
In the present study, the prevalance of Onodi cells was 21.2% of the patients. Onodi cells were observed 40.7% on the right side and 25.9% on the left side. In 33.4% of the patients, bilateral Onodi cells were present. In the male group, Onodi cells were detected in 24.5% of the patients. In the females, Onodi cells were detected in 17.6% patients. According to Driben et al. the prevalence of Onodi cell was 39% on endoscopic examination of cadavers [14]. In the studies of Onodi cell conducted by CT, the prevalence was reported as 25% [16], 12% [17] and 8% [18].
Three patterns of pneumatization of Onodi cells are described in the Thimmaiah and Anupama’s study [3] with Type II (superolateral) being most common followed by Type I (superior) and Type III (Lateral). In the present study, Onodi cell types were detected as Type I (43.8%), Type II (36.2%) and Type III (20.0%) on the right side and Type I (48.4%), Type II (32.8%) and Type III (18.8%) on the left side. There was a positive correlation between the right and left Onodi cell types.
In the present study, Onodi cell presence and ACP pneumatization were found as statistically significant. In 65.5% of the patients, Onodi cells and ACP pneumatization were absent. ACP pneumatization was present in 35.4% of the cases. In nine cases, bilateral Onodi cells and ACP pneumatization were detected.
Nomura et al. [19] reported that OCs move the SS downwards, reduce volume, and, therefore, are associated with sphenoiditis. In the present study, sphenoid sinusitis was detected in 11.4% of the Type I and 13.8% of the Type II Onodi cells on the right side. On the left side, it was detected in 12.9% of Type I and 19.0% of the Type II Onodi cells. Senturk et al. [11] reported that the coexistence of ipsilateral Onodi cells increased the expression of sphenoiditis by 1.5-fold. In the present study, we did not find the relationship between Onodi cells and sphenoid sinusitis.
If the optic nerve bulging into the Onodi cell is prominent, this increases the risk of damage to the optic nerve during sphenoid sinus surgery. Furthermore, in most cases, the sphenoid sinus is located behind the posterior ethmoid cell, and at this point the bulging of the optic nerve can be observed only in the superolateral wall. Therefore, the surgeon who is not prepared to account for the ethmoid cell that extends over the sphenoid sinus may actually work on the Onodi cell instead of the sphenoid sinus [8].
Chmielik et al. [8] (in 18–82-year-old) adults; and Chmielik and Chmielik [9] (in 8–18-year-old children) reported that in their study of 196 cases, in 44.4%, there was no contact between the optic canal and posterior ethmoid cells (Type I). Type II optic canal was detected in 14.8% and type IV optic canal was detected in 25% of the cases. In the present study, type 1 optic canal (no contact between optic canal and posterior ethmoid cells) was detected as 25% on the right side and 28.1% on the left side. However, a total of type II, III and IV optic canals, detected in the patients with Onodi cells, were found in 75% of the patients on the right side and 71.9% of the patients on the left side. Right optic canal types were detected as Type IV > Type I > Type II > Type III. Left optic canal types were detected as Type IV > Type I > Type II > Type III. Our study shows that type 4 optic canal was detected mostly on both sides, 35% and 34.4% on the right and left sides, respectively. There was a positive correlation between right and left optic canal types.
De Lano et al. [20] reported that posterior ethmoid cell and optic nerve contact were detected in 3% of the patients with chronic inflammatory sinus disease by coronal CT. However, in another study of the Yeoh and Tan [21], in 65% of the cases, posterior ethmoid cells and optic nerve relationship was present. Optic canal into spheno-ethmoidal cell occurrence was detected in 51% of the cases.
Yeoh and Tan [21] concluded that the most dangerous type of the optic canals was the canals with no bulging, because of the extremely thin wall separating ethmoid cell and the optic canal [21]. On the contrary, Dessi thought that optic canal bulging more than 50% of the circumference into the ethmoid cells cause the risk during the surgery [22]. In the present study, the authors conclude that type 4 bulging of the optic canal is the most dangerous type for the damage of the optic canal during the surgery. Especially, inflammatory changes and tumoral pathologies may destroy the walls of the optic canals.
Identification of Onodi cell is very important clinically because of its proximity to optic nerve canal [22]. Improving the preoperative identification of these Onodi cells and their pattern of pneumatization by multi dimensional CT (MDCT) can decrease the risk of subsequent optic nerve injury [3].
We concluded that the type IV Onodi–optic canal relationship was the most common finding in our study. Onodi cell presence and their patterns of pneumatization must be evaluated on PNSCT preoperatively to avoid optic canal damage.
References
Stammberger HR, Kennedy DW, Anatomic Terminology Group (1995) Paranasal sinuses:anatomic terminology and nomenclature. Ann Otol Rhinol Laryngol Suppl 167:7–16
Lim CC, Dillon WP, McDermott MW (1999) Mucocele involving the anterior clinoid process: MR and CT findings. AJNR Am J Neuroradiol 20:287–290
Thimmaiah VT, Anupama C (2017) Pneumatization patterns of onodi cell on multidetector computed tomography. J Oral Maxillofac Radiol 5(3):63–66
Ozturan O, Yenigun A, Degirmenci N, Aksoy F, Veyseller B (2013) Co-existence of the Onodi cell with the variation of perisphenoidalstructures. Eur Arch Otorhinolaryngol 270:2057–2063
Chee E, Looi A (2009) Onodi sinusitis presenting with orbital apexsyndrome. Orbit 28:422–424
Deshmukh S, DeMonte F (2007) Anterior clinoidal mucocele causingoptic neuropathy: resolution with nonsurgical therapy: case report. J Neurosurg 106:1091–1093
Klink T, Pahnke J, Hoppe F, Lieb W (2000) Acute visual loss by an Onodi cell. Br J Ophthalmol 84:801–802
Chmielik A, Chmielik L, Boguslawska-Walecka R, Warszawa PL, Warsaw PL (2014) The prevalence and CT detection of Onodi cell types. ECR 2014 Congress, poster no: C-1566. https://doi.org/10.1594/ecr2014/C-1566. https://www.myesr.org/. Accessed 26 Oct 2018
Chmielik L, Chmielik A (2017) The prevalence of the Onodi cell—most suitable method of CT evaluation in its detection. Int J Pediatr Otorhinolaryngol 97:202–205
Metson R, Gliklich RE, Stankiewicz JA et al (1997) Comparison of sinus computed tomography staging systems. Otolaryngol Head Neck Surg 117(4):372–379
Senturk M, Guler I, Azgin I et al (2017) The role of Onodi cells in sphenoiditis: results of multiplanar reconstruction of computed tomography scanning. Braz J Otorhinolaryngol 83:88–93
Bilici S, Huq GE, Sunter AV, Yigit O, Yildiz M (2014) Onodi cell mucocele: case report. Otolaryngology 4–4
Kim JY, Kim HJ, Kim CH, Lee JG, Yoon JH (2005) Optic nerve injury secondary to endoscopic sinus surgery: an analysis of three cases. Yonsei Med J 46(2):300–304
Driben JS, Bolger WE, Robles HA, Cable B, Zinreich SJ (1998) The reliability of computerized tomographic detection of the Onodi (sphenoethmoid) cell. Am J Rhinol 12:105–111
Weinberger DG, Anand VK, Al-Rawi M, Cheng HI, Messina AV (1996) Surgical anatomy and variations of the Onodi cell. Am J Rhinol 10:365–370
Nitinavakarn B, Thanaviratananich S, Sangsilp N (2005) Anatomical variations of the lateral nasal wall and paranasal sinuses: a CT study for endoscopic sinus surgery (ESS) in Thai patients. J Med Assoc Thai 88:763–768
Unal B, Bademci G, Bilgili YK, Batay F, Avci E (2006) Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat 28:195–201
Arslan H, Aydinlioğlu A, Bozkurt M, Egeli E (1999) Anatomic variations of the paranasal sinuses: CT examination for endoscopic sinus surgery. Auris Nasus Larynx 26:39–48
Nomura K, Nakayama T, Asaka D et al (2013) Laterally attached superior turbinate is associated with opacification of the sphenoid sinus. Auris Nasus Larynx 40:194–198
De Lano MC, Fun FY, Zinreich SJ (1996) Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. Am J Neuroradiol 17(4):669–675
Yeoh KH, Tan KK (1994) The optic nerve in the posterior ethmoid in Asians. Acta Otolaryngol 114(3):329–336
Dessi I, Moulin G, Castro F, Chagnaud C, Cannoni M (1994) Protrusion of the optic nerve into the ethmoid and sphenoid sinus: prospective study of 150 CT studies. Neuroradiology 36:515–516
Funding
There is no funding for this article.
Author information
Authors and Affiliations
Contributions
AO: planning, designing, data collection, literature survey. NBM: planning, designing, literature survey, statistical analysis, writing. NA: planning, designing, literature survey. MHS: planning, designing, literature survey. MI: planning, designing, data collection, literature survey.
Corresponding author
Ethics declarations
Financial disclosure
There is no financial disclosures of the authors.
Conflict of interest
The author Adnan Özdemir declares that he has no conflict of interest. The author Nuray Bayar Muluk declares that she has no conflict of interest. The author Neşe Asal declares that she has no conflict of interest. The author Mehmet Hamdi Şahan declares that he has no conflict of interest. The author Mikail Inal declares that he has no conflict of interest.
Ethical approval
This study is retrospective. Ethics committee approval was obtained from Kırıkkale University Non-invasive Research Ethics Committee (Date: 24.10.2018, Number: 2018.10.15).
Informed consent
There is no need to take informed consent, because the data were evaluated retrospectively.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Özdemir, A., Bayar Muluk, N., Asal, N. et al. Is there a relationship between Onodi cell and optic canal?. Eur Arch Otorhinolaryngol 276, 1057–1064 (2019). https://doi.org/10.1007/s00405-019-05284-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05284-0