Abstract
Purpose
To evaluate, using drug-induced sleep endoscopy (DISE), sites of upper airway obstruction and pattern of collapse in patients over 65 years old affected by obstructive sleep apnea. To compare sites and pattern of collapse of elderly patients with a group of patients younger than 65 years.
Methods
A group of 55 patients aged over 65 years were enrolled in this prospective study. Fifty patients under 65 years old were collected in the control group. Polysomnographic data and clinical parameters such as the daytime sleepiness, and body mass index were evaluated for both groups of patients. All patients underwent DISE examination with VOTE classification.
Results
The AHI value increased with aging whereas elderly patients presented a reduction in daytime sleepiness. Elderly patients showed a higher incidence of total collapse in the velum region compared to younger patients (90.9% vs 70%;); the older patients showed a lower degree of total oropharyngeal lateral wall collapse with respect to younger patients, (20% vs 50%). No difference in tongue base collapse emerged between the two subgroups of patients.
Conclusion
Elderly patients showed a higher incidence of total collapse in the velum and a lower incidence in the oropharyngeal lateral wall compared to younger patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive Sleep Apnea (OSA) syndrome is a respiratory sleep disorder characterized by partial or complete recurrent episodes of upper airway collapse, that occurs during the night. OSA manifested with a reduction (hypopnea) or complete cessation (apnea) of airflow in the upper airways, in the presence of breathing effort [1,2,3].
OSA is a frequent and often underestimated pathology affecting between 2 and 5% of middle-aged population [3,4,5]. However, it has been observed that it may reach a much higher incidence in older people [6,7,8,9,10]. Different studies have estimated OSA incidence rates from 5.6 to 70% in people over 65 [7,8,9,10,11,12]. Analyzing 427 elderly people over 65, suffering from OSA, Ancoli et al. [7], showed that 24% of them had an apnea/hypopnea (AHI) index greater than 5 and that 62% had a respiratory disturbance, with a Respiratory Disorder Index (RDI) ≥ 10. In another study comprising 5615 men and women between 40 and 98 years of age, sleep apnea was found to be most frequent in subjects aged 60 years or older (approximately 50% had an AHI of 5–14, and approximately 20% had an AHI ≥ 15) [4].
Aging is also associated with changes in OSA related parameters (increase of AHI, reduction of night-time SpO2, reduction of daytime sleepiness, etc.) and type of sleep [9,10,11,12,13]. Therefore, it is possible that the number of obstruction sites and collapse pattern may change over time due to changes in pharyngeal anatomy, redistribution of body fat and/or the increased laxity of the oro/hypo-pharyngeal muscular structures, that are known to occur with aging [14,15,16,17].
These findings implicate the importance of assessment and classification of sites and patterns of collapse in elderly OSA patients. Polysomnography (PSG) is the gold standard for the diagnosis of OSA and evaluation of its severity (number of obstructive events per hour, SpO2 etc.), but it cannot provide detailed and accurate data regarding the anatomic localization of the obstructive sites [1, 18].
Drug-induced sleep endoscopy (DISE) is a fiber-optic examination of the upper airway under controlled sedation. It is considered the best procedure for determining the site(s) and grade of obstruction(s), and patterns of airways collapse in OSA patients. Moreover, it quantifies, with the aid of the DISE, the location and collapse pattern of the upper airways in OSA patients and can be used to customize treatment options and/or improve therapeutic outcomes [19,20,21].
The DISE examination studies reported in the literature were mainly performed in middle-aged adults [21,22,23,24,25]. To our knowledge, no clinical prospective studies have compared the results of upper airway DISE examination between elderly and younger OSA patients.
This study was designed to analyze the role of DISE for evaluation of obstructive sites and pattern of collapse in patients over 65 years old affected by OSA. Besides, the sites and pattern of collapse of elderly patients were compared with a group of patients younger than 65 years, evaluated using the same study protocol.
Materials and methods
Evaluating methods and enrollment of patients
In accordance with the existing literature, in this study an age over 65 years was taken to be indicative of elderly patients [7,8,9,10,11,12]. Patients aged over 65 years, consecutively admitted to our Department to underwent DISE, were initially enrolled in this prospective study. All the DISE procedures were performed at the Otolaryngology, Head and Neck and Oral Surgery Unit of the Morgagni Pierantoni Hospital in Forlì, Italy, between January 2016 and June 2018.
Patients submitted to surgical treatment for OSA or who had been submitted to other head-neck surgical procedures were excluded from the study, to evaluate the sites/pattern of collapse without surgical bias. Patients receiving pharmacological treatment for the OSA or drugs with an impact on the cognitive function were also excluded from the study. Patients with ASA 4, or with propofol allergy were also excluded to the study.
As a control group, patients aged under 65 years, who underwent DISE in the same period of time, were prospectively enrolled in the study, following the same exclusion criteria of the study group.
Daytime sleepiness, evaluated through the Epworth Sleepiness Scale (ESS), body mass index (BMI) and smoking history were assessed for both groups of patients.
The night before the DISE procedure all the patients of the study underwent a polysomnographic (PSG) examination.
The apnea-hypopnea index (AHI), Oxygen Desaturation Index (ODI), and the lowest SpO2 (LOS) were scored by a blinded registered polysomnographic technician using established criteria [1, 18]. The PSG data of both subgroups of patients was analyzed and compared.
In accordance with the American Academy of Sleep Medicine (AASM) [26, 27], diagnosis and classification of OSA was made on the basis of the Apnea-hypopnea index (AHI) index. Patients were classified into mild OSA (AHI ≥ 5 and < 15), moderate OSA (AHI ≥ 15 and < 30) and severe OSA (AHI ≥ 30) [18, 19]. The simple snorers according to PSG results (AHI was < 5/h) were excluded from the study.
DISE protocol and obstructive pattern classification
The standardized protocol was employed in all the procedures, as reported in the European position paper on DISE [19, 28]. All the DISE procedures were performed by two of the co-authors of this study (R. G. and G. I).
All DISE procedures were executed in the operating room with an anesthesiologist.
Propofol represented the sedative agent applied during all the DISE procedures and the Target Control Infusion system (TCI) was adopted [28, 29]. No decongestion or topical anesthesia was employed.
The bispectral index (BIS) was employed to monitor the depth of sedation during DISE [28,29,30,31].
At least two or more cycles (snoring, collapse) for each segment of the upper airway were observed.
The VOTE system proposed by Kezirian et al. [32] was applied to classify all DISE procedures (Table 1).
Patients were observed firstly in the standard supine primary position and then in lateral decubitus, for assessing significant modification of the upper airways during the latter position, to identify the positional OSA (POSA) [19, 28, 33, 34]. Finally, the efficacy of mandibular advancement (pull-up manoeuver) was tested in each patient during the DISE.
Statistical analysis
The χ2 test was employed to evaluate the differences between the two groups of patients. The Student t test was used to compare the analyzed factors. A p value of < 0.05 was taken as the threshold of statistical significance. Linear regression was used to correlate AHI and ESS with aging.
This research study was performed in accordance with the principles of the Declaration of Helsinki and approved by the local Ethics Committee. Informed consent was obtained from all individual participants included in the study.
Results
Patient’s characteristics results
Fifty-five patients with an OSA diagnosis and age ≥ 65 years old were enrolled in the study. Fifty patients with age < 65 years old, were enrolled in a control group of younger patients.
Patient characteristics (Age, BMI and ESS) and PSG data (AHI, ODI and LOS) are summarized in Table 2.
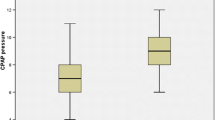
The mean age of patients over 65 years was 68.6 years (range 65–80), whereas the mean age of the control group was 50.7 (range 21–62) years-old (p = 0.0001). The average BMI of the study group was 28.5 while the average ESS was 7.3. The mean BMI of elderly patients was found to be greater that in younger patients (mean BMI 27.2) with a significant statistical difference (p = 0.02). The average ESS of elderly patients was lower than those of younger patients (p 0.0001). Regression analysis showed ESS reduction with aging (p = 0.0001) (Fig. 1).
History of smoking was present in 14 (25.4%) of elderly patients and 17 (34%) of young patients (p = 0.5).
Polysomnographic parameters results
Regarding the severity of OSA, a mean AHI of 37.7 and 31.7 emerged in elderly and young patients respectively. Comparing these two mean values, no statistical difference emerged (p = 0.07). Similarly, no differences emerged in a comparison of the AHI classes of elderly and young patients (p > 0.05 for each sub-class of OSA severity) (Table 3). However, in the entire group of patients studied (both above and below 65 years of age) regression analysis showed an increase in AHI as patients’ age increased (p = 0.03) (Fig. 2).
A statistical difference (p = 0.001) was present between the average LOS value of elderly patients (70.8) and that of younger patients (72.5).
DISE results
No differences in the method of DISE execution were found among elderly and young patients. This is confirmed by the similar average values of BIS and propofol that emerged in both sub-groups of patients (Table 4).
During the DISE procedure, interesting data regarding different sites of obstruction and pattern of collapse emerged in elderly and young patients. The data regarding DISE in elderly and younger patients is summarized in Table 5.
Velum (V) collapse was present in 100% of elderly patients (90.9% grade 2 and 9.1% grade 1); elderly patients showed a higher incidence of total collapse in the velum region compared to younger patients (90.9% vs 70%;); this difference was statistically significant (p = 0.01). No differences in the pattern of velum collapse were found between the two sub-groups of patients (p > 0.05 in each case).
Oropharynx lateral wall (O) collapse was present in 45.4% of elderly patients. The incidence of lateral wall collapse was different in the two groups of patients (p = 0.02). Elderly patients showed a lower incidence of total oropharyngeal lateral wall collapse respect to younger patients, with an incidence of 20% and 50% in the two groups of patients, respectively (p = 0.002).
A total collapse of the tongue base (T) was present in 45.4% of elderly patients and 50% of young patients (p = 0.7). No difference in this type of collapse emerged between the two subgroups of patients.
Epiglottis collapse was present in 49.1% of elderly patients. This subgroup of patients would seem to present most frequently a partial epiglottis collapse, compared to young patients (p = 0.0006).
Finally, during the DISE procedure, elderly patients showed a lower LOS in comparison to younger patients (72.5 vs 78.9, p = 0.001), whereas similar values in terms of POSA and positive mandibular pull-up emerged between the two sub-groups of patients (Table 6).
Discussion
Aging substantially increases the risk of obstructive sleep apnea. Besides, elderly patients may present differences in polysomnographic parameters (AHI, oxygen desaturation index; LOS) with respect to young patients. Despite the fact that the AHI value increases with aging, elderly patients have a reduction in daytime sleepiness [6,7,8,9,10,11,12,13]. George et al. [35] reported higher duration of apnea/hypopnea events, longer hypoxemia, as well as lower oxygen saturation in elderly patients than in their younger counterparts, whereas, Morrell et al. [9], studying 1281 patients affected by sleep disordered breathing, found a significative reverse correlation (p = 0.04) between age and ESS.
Evaluation of AHI and ESS in this study seems to confirm these aspects. Regression analysis showed greater AHI values as patient age increased (p = 0.03). The elderly patients in our study had a lower average ESS compared with the younger ones with a positive inverse correlation (p = 0.0001), confirming the daytime sleepiness reduction in patients > 65 years-old.
The mechanisms underlying the tendency of elderly patients to have a greater incidence/severity of OSA syndrome still remain unclear [10, 16]. Probably, as reported by some authors, the number, site and pattern of upper airway obstructions change throughout time due to alterations in pharyngeal anatomy and biomechanics, or deterioration of the function of pharyngeal dilator muscles [11,12,13,14,15,16].
Given the high incidence and severity of the OSA syndrome in the elderly population and considering the increase in the average age of the world population, is important to understand if changes occur in the pharyngeal anatomy and sites/pattern of obstruction in people over 65 years [7,8,9,10,11].
Imaging studies have demonstrated that, compared to middle-aged subjects, older adults present changes in bony structure and fat deposits in the pharyngeal walls, which result in a greater upper airway collapsibility [15,16,17]. Malhotra et al. [16], demonstrated a significant increase in the size of the pharyngeal fat pads with aging, independently from BMI, and also suggested that soft tissue volume is a risk factor for OSA in older people. Also, Carlisle et al. [14] reported that older males compared with younger patients, had a greater pharyngeal caliber measured using acoustic reflection, a greater combined retro-palatal and retro-glossal pharyngeal length, larger and longer soft palate and increased para-pharyngeal fat measured using MRI. Besides, as reported by some authors, increasing age is related to both velopharyngeal collapsibility (p < 0.01) and an increase in pharyngeal resistance during sleep (p < 0.01), independently from body mass index (BMI) and gender [12,13,14,15,16,17].
However, these studies were based on an analysis of an awake patient population which only allows only a static assessment of upper airways, whereas upper airway obstruction in OSA patients is a dynamic process. This is the main reason why we decided to carry out the upper airway assessment during the DISE procedure, which allows a more effective dynamic analysis of the upper airways in terms of site, pattern and grade of collapse during drug-induced sleep.
In this study, using the DISE, we analyzed the sites and pattern of upper airways collapse present in elderly patients and evaluated the differences that emerged with patients younger than 65 years old.
Our results showed that velum collapse was present in 100% of elderly patients with a statistical difference in the incidence of total collapse compared to younger patients (p = 0.01). This finding could be explained by the greater velopharyngeal collapsibility and increase in the length of the soft palate and uvula, observed in elderly patients [12,13,14,15,16,17].
Collapse of the oropharynx lateral walls (O) during DISE was present in 45.4% of elderly patients of our study. These patients also showed a lower incidence of total oropharyngeal lateral wall collapse respect to younger patients, (20% vs 50%, p = 0.002). The atrophy of the lateral pharyngeal muscle that generally occurs with age could contribute to the reduction of the lateral wall collapse observed in older patients [13,14,15,16, 36].
Similar incidences for total or partial tongue base collapse were observed. This finding could be related to the absence of age-related effects on pathogenetic factors causing tongue base collapse.
Aging is a cause of laxity of the greater laryngopharyngeal muscular structures. This could explain why partial epiglottis collapse was most frequently observed in elderly patients of this study [37].
The knowledge of the sites, grades and patterns of upper airway collapse, which frequently occur in elderly patients, could have implications in the choice of the best therapeutic strategy for these patients [6,7,8,9,10]. Continuous positive airway pressure remains the gold standard therapy for elderly OSA patients. However, this modality of treatment is not tolerated by many elderly patients with OSA, and surgery remains an alternative treatment in these cases [38]. Velum collapse was present in 100% of elderly patients (90.9% grade 2 and 9.1% grade 1). This result could indicate that the velopharyngeal surgery should be considered in the surgical planning of elderly patients. Moreover, because many of elderly patients showed a complete tongue base collapse (45.5%), isolated palatal surgery may not be adequate in these patients and multilevel surgery could be required. The frequent tongue base obstruction observed in these patients could also suggest the use of mandibular advancement devices (MAD), if the dental condition allows it [1,2,3,4,5,6, 39].
In OSA patients the different grade of AHI could influence the different sites and collapse patterns observed during the DISE procedure. In this study the regression analysis showed an increase of the AHI value with aging. However, the average AHI, as well as the incidence of the different sub-classes of OSA severity of the two sub-groups of patients, did not present a statistical difference (p > 0.05 in each cases). This would suggest that the AHI values found in the two patient sub-groups are not to be considered as potential biases of the study. Besides, no differences between propofol concentrations and BIS values in the two groups of patients emerged. This could mean that there is no bias in the DISE execution capable of interfering with the different results obtained in elderly and young patients.
One limitation of this study is that the pathophysiological mechanisms of pharyngeal collapse (pharyngeal critical pressure, oral breathing and negative pressure reflex, etc.), co-morbidities (hypertension, diabetes mellitus, dyslipidemia), underlying health status (renal function or mental function), were not evaluated and analyzed. However, this may be considered as a preliminary observational study to assess the effect of age on the site, severity and pattern of collapse observed during the DISE examination. Further studies to confirm this data and to identify a possible correlation between the sites and pattern of upper airway collapse in elderly patients presenting OSA pathophysiological mechanisms and clinical co-morbidities are under way.
Another limiting factor is the different mean BMI which emerged between the two groups of studied patients. Usually BMI increases with aging and it could influence the severity of the OSA [1,2,3,4,5,6,7,8,9, 39]. BMI variation could also interfere with sites, type and severity of obstructions. However, it should be considered that scarce study about the differences of pharyngeal collapse due to different BMI values has been reported in literature [12,13,14,15,16]. High BMI may be also related to a positional OSA [1,2,3,4, 11,12,13,14,15]. Therefore, BMI differences in the study groups could be considered as a possible bias of the positional OSA results.
Conclusion
DISE is an effective and safe method that allows the evaluation of the sites and pattern of collapse in elderly people. Elderly patients showed a higher incidence of total collapse in the velum and a lower incidence of total oropharyngeal lateral wall collapse with respect to young patients.
Accurate knowledge of the sites and pattern of collapse of elderly patients with OSA is potentially useful for customizing treatment options and/or for improving therapeutic outcomes [38].
References
Bosi M, De Vito A, Gobbi R, Poletti V, Vicini C (2017) The importance of obstructive sleep apnoea and hypopnea pathophysiology for customized therapy. Eur Arch Otorhinolaryngol 274:1251–1261
Magliulo G, de Vincentiis M, Iannella G et al (2018) Eustachian tube evaluation in patients with obstructive sleep apnea syndrome. Acta Otolaryngol 138:159–164
Shochat T, Pillar G (2003) Sleep apnoea in the older adult: pathophysiology, epidemiology, consequences and management. Drugs Aging 20:551–560
Young T, Shahar E, Nieto FJ et al (2002) Predictors of sleep-disordered breathing in community-dwelling adults: the sleep heart health study. Arch Intern Med 162:893–900
Magliulo G, De Vincentiis M, Iannella G et al (2018) Olfactory evaluation in obstructive sleep apnoea patients. Acta Otorhinolaryngol Ital 38:338–345
Yaremchuk K (2018) Sleep disorders in the elderly. Clin Geriatr Med 34:205–216
Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O (1991) Sleep-disordered breathing in community-dwelling elderly. Sleep 14:486–495
Ancoli-Israel S, Kripke DF, Klauber MR et al (1996) Morbidity, mortality and sleep-disordered breathing in community dwelling elderly. Sleep 19:277–282
Morrell MJ, Finn L, McMillan A, Peppard PE (2012) The impact of ageing and sex on the association between sleepiness and sleep disordered breathing. Eur Respir J 40:386–393
McMillan A, Morrell MJ (2016) Sleep disordered breathing at the extremes of age: the elderly. Breathe (Sheff) 12:50–60
Suzuki K, Miyamoto M, Hirata K (2017) Sleep disorders in the elderly: diagnosis and management. J Gen Fam Med 18:61–71
Ahmad N, Srinivasan K, Naicker TR, Moudgil H (2014) Sleep apnoea in the elderly. Lancet Respir Med 2:21
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014
Carlisle T, Carthy ER, Glasser M et al (2014) Upper airway factors that protect against obstructive sleep apnoea in healthy older males. Eur Respir J 44:685–693
Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, Pack AI (1995) Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 152:1673–1689
Malhotra A, Huang Y, Fogel R et al (2006) Aging influences on pharyngeal anatomy and physiology: the predisposition to pharyngeal collapse. Am J Med 119:9–14
Jang MS, Kim HY, Dhong HJ et al (2014) Effect of parapharyngeal fat on dynamic obstruction of the upper airway in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190:1318–1321
Bosi M, De Vito A, Vicini C, Poletti V (2017) The role of compact polysomnography/polygraphy in sleep breathing disorder patients’ management. Eur Arch Otorhinolaryngol 274:2013–2028
De Vito A, Carrasco Llatas M, Ravensloot M et al. (2018) European position paper on drug-induced sleep endoscopy (DISE): 2017 update. Clin Otolaryngol. https://doi.org/10.1111/coa.13213
Charakorn N, Kezirian EJ (2016) Drug-induced sleep endoscopy. Otolaryngol Clin North Am 49:1359–1372
Campanini A, Canzi P, De Vito A, Dallan I, Montevecchi F, Vicini C (2010) Awake versus sleep endoscopy: personal experience in 250 OSAHS patients. Acta Otorhinolaryngol Ital 30:73–77
De Vito A, Agnoletti V, Zani G et al (2017) The importance of drug-induced sedation endoscopy (D.I.S.E.) techniques in surgical decision making: conventional versus target controlled infusion techniques-a prospective randomized controlled study and a retrospective surgical outcomes analysis. Eur Arch Otorhinolaryngol 274:2307–2317
Koo SK, Choi JW, Myung NS, Lee HJ, Kim YJ, Kim YJ (2013) Analysis of obstruction site in obstructive sleep apnea syndrome patients by drug induced sleep endoscopy. Am J Otolaryngol 34:626–630
Ravesloot MJ, de Vries N (2011) One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation. Laryngoscope 121:2710–2716
Golbin D, Musgrave B, Succar E, Yaremchuk K (2016) Clinical analysis of drug-induced sleep endoscopy for the OSA patient. Laryngoscope 126:249–253
Richard B, Berry R, Brooks CE, Gamaldo et al (2015) AASM manual for the scoring of sleep and associated events. American Academy of Sleep Medicine, Darien
Epstein LJ, Kristo D, Strollo PJ Jr et al (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5:263–276
De Vito A, Carrasco Llatas M, Vanni A et al (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18:453–465
De Vito A, Agnoletti V, Berrettini S et al (2011) Drug-induced sleep endoscopy: conventional versus target controlled infusion techniques—a randomized controlled study. Eur Arch Otorhinolaryngol 268:457–462
Lo YL, Ni YL, Wang TY et al (2015) Bispectral index in evaluating effects of sedation depth on drug-induced sleep endoscopy. J Clin Sleep Med 11:1011–1020
Traxdorf M, Tschaikowsky K, Scherl C, Bauer J, Iro H, Angerer F (2016) Drug-induced sleep endoscopy (DISE) with target controlled infusion (TCI) and bispectral analysis in obstructive sleep apnea. J Vis Exp 6:18
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268:1233–1236
Levendowski DJ, Oksenberg A, Vicini C, Penzel T, Levi M, Westbrook PR (2018) A systematic comparison of factors that could impact treatment recommendations for patients with positional obstructive sleep apnea (POSA). Sleep Med 50:145–151
Safiruddin F, Koutsourelakis I, de Vries N (2014) Analysis of the influence of head rotation during drug-induced sleep endoscopy in obstructive sleep apnea. Laryngoscope 124:2195–2199
George E, Katerina V, Maria S, Lambros B, Konstantina N, Dimitrios G (2012) Clinical features and polysomnographic findings in greek male patients with obstructive sleep apnea syndrome: differences regarding the age. Sleep Disord 2012:324
Heinzer RC, Stanchina ML, Malhotra A et al (2006) Effect of increased lung volume on sleep disordered breathing in patients with sleep apnoea. Thorax 61:435–439
Torre C, Camacho M, Liu SY, Huon LK, Capasso R (2016) Epiglottis collapse in adult obstructive sleep apnea: a systematic review. Laryngoscope 126:515–523
Gouveia CJ, Cramer JD, Liu SY, Capasso R (2017) Sleep surgery in the elderly: lessons from the national surgical quality improvement program. Otolaryngol Head Neck Surg 156:757–764
Wilhelm CP, deShazo RD, Tamanna S, Ullah MI, Skipworth LB (2015) The nose, upper airway, and obstructive sleep apnea. Ann Allergy Asthma Immunol 115:96–102
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies were in accordance with the ethical standards of the institutional committee of the Morgagni Pierantoni Hospital and with the 1964 Helsinki declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Vicini, C., De Vito, A., Iannella, G. et al. The aging effect on upper airways collapse of patients with obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 275, 2983–2990 (2018). https://doi.org/10.1007/s00405-018-5163-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5163-5