Abstract
Age-related hearing loss (ARHL) is postulated to affect dementia. Our study aims to investigate the relationship between ARHL and the prevalence, and 10-year incidence of dementia in the Taiwan National Health Insurance Research Database (NHIRD). We selected patients diagnosed with ARHL from the NHIRD. A comparison cohort comprising of patients without ARHL was frequency-matched by age, sex, and co-morbidities, and the occurrence of dementia was evaluated in both cohorts. The ARHL cohort consisted of 4108 patients with ARHL and the control cohort consisted of 4013 frequency-matched patients without ARHL. The incidence of dementia [hazard ratio (HR), 1.30; 95% confidence interval (CI 1.14–1.49); P = 0.002] was higher among ARHL patients. Cox models showed that being female (HR, 1.34; 95% CI 1.07–1.68), as well as having co-morbidities, including chronic liver disease and cirrhosis, rheumatoid arthritis, hypertension, diabetes mellitus, stroke, head injury, chronic kidney disease, coronary artery disease, alcohol abuse/dependence, and tobacco abuse/dependence (HR, 1.27; 95% CI 1.11–1.45), were independent risk factors for dementia in ARHL patients. We found ARHL may be one of the early characteristics of dementia, and patients with hearing loss were at a higher risk of subsequent dementia. Clinicians should be more sensitive to dementia symptoms within the first 2 years following ARHL diagnosis. Further clinical studies of the relationship between dementia and ARHL may be necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hearing loss is common in older adults, but the relationship between dementia and age-related hearing loss (ARHL) is unclear. Deficits in peripheral hearing and central auditory processing can be attributed to ARHL [1, 2]. The prevalence of hearing loss increases with patient age; approximately 1 in 3 people over 65 years of age have disabling hearing loss (http://data.worldbank.org/). Dementia is one of the most common health problems among older adults. The World Alzheimer Report estimated that 35.6 million people were living with dementia worldwide in 2010, and that this figure may reach 65.7 million by 2030, and 115.4 million by 2050 [3]. Notably, central auditory dysfunction is prevalent in Alzheimer dementia, but the mechanism has not been established [4, 5]. Several population-based studies have determined the association of hearing loss and cognitive decline [4–6]. Previous studies even proved some conflicting results of gene influence in dementia and hearing loss [7, 8]. However, a statistically significant relationship between dementia and ARHL was reported in some published cross-sectional studies [9–12] and several supportive longitudinal studies [13–16] while some only focus on central auditory dysfunction [17]. More focused research is needed to understand the mechanism and association between ARHL and dementia. To our knowledge, no large-scale nationwide population-based longitudinal study has ever investigated this association.
Alzheimer’s disease (AD) is the most common subtype of dementia. The increasing prevalence of AD is a serious public health problem [3]. Early diagnosis of dementia or AD enables the progression of the disease to be managed. Nonetheless, because of the insidious onset of AD, it is difficult to differentiate between normal aging-related cognitive decline and the pathologic dysfunction of the early stages of AD. We hypothesized that ARHL is an early sign of dementia and could be used as a marker for early diagnosis.
In this 10-year nationwide population-based cohort study, we explored the relationship between ARHL and the incidence of dementia in Taiwan by comparing patients with and without ARHL.
Methods
Data source
The National Health Insurance (NHI) program, established in 1995, is a mandatory, state-run health insurance program that provides comprehensive medical care coverage for outpatient, inpatient, emergency, and traditional Chinese medicine treatments to all residents of Taiwan (23.72 million people). The coverage rate is more than 99% (http://www.nhi.gov.tw/english/index.aspx). The National Health Research Institutes (NHRI) is responsible for managing all reimbursement claim data in the National Health Insurance Research Database (NHIRD); patient confidentiality is maintained in accordance with the directives of the National Health Insurance Administration. To protect the privacy of all insures, the NHRI anonymizes the identification numbers of all NHIRD records. Data for this population-based retrospective study were taken from the 2000 Longitudinal Health Insurance Database (LHID2000), which is a subset of the NHIRD. The LHID2000 contains claims data of 1 million people randomly selected from the 2000 Registry of Beneficiaries. All clinical diagnoses were recorded using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes.
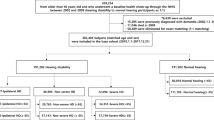
Sampled participants
We collected data on patients who had at least three diagnoses of ARHL (ICD-9-CM codes 389.10–389.12 and 388.01) within 4 months during the period of 2010–2012 for the ARHL cohort. The dates of ARHL diagnosis were used as the index date. Patients who had a history of dementia (ICD-9-CM codes 290, 294.1 and 331.0–331.2) before the index date, were younger than 50 years of age, had other types of hearing loss(388.2, 389.0, 389.2), sudden hearing loss, conductive hearing loss, mixed conductive and sensorineural hearing loss or had incomplete age or gender information were excluded. Moreover, dementia patients were only enrolled with at least 3 times dementia diagnosis within 4 months and confirmed by psychiatrist. Control patients without dementia or ARHL at the baseline were randomly selected from the LHID2000 and frequency-matched with each dementia case by age (every 5-year span), gender, and year of dementia diagnosis. The controls were subject to the same exclusion criteria as the ARHL group.
Outcome and comorbidities
All patients were followed until they were diagnosed with dementia, were censored for failure to follow-up, withdrew from the NHI, or until December 31, 2011. The comorbidities examined for were the following: chronic liver disease and cirrhosis (CLD; ICD-9-CM code 571), rheumatoid arthritis (RA; ICD-9-CM code 714), hypertension (HTN; ICD-9-CM codes 401–405), diabetes mellitus (DM; ICD-9-CM code 250), stroke (ICD-9-CM codes 430–438), head injury (ICD-9-CM codes 850–854), chronic kidney disease (CKD; ICD-9-CM code 585), coronary artery disease (CAD; ICD-9-CM codes 410–414), alcohol abuse/dependence (ICD-9-CM codes 305.0 and 303), tobacco abuse/dependence (ICD-9-CM codes 305.1), and chronic obstructive pulmonary disease (COPD; ICD-9-CM codes 490–492, 494, and 496). All comorbidities were defined before the index date. To increase the credibility of dementia diagnosis, only those patients with at least 3 times of dementia diagnosed in psychiatric clinics within 4 months were enrolled in our data.
Data availability statement
All data and related metadata were deposited in an appropriate public repository. The data from the NHIRD on the study population (http://w3.nhri.org.tw/nhird//date_01.html) were maintained in the NHIRD (http://nhird.nhri.org.tw/). The NHRI is a nonprofit foundation established by the government of Taiwan.
Statistical analysis
We tested the categorical variables of the ARHL cohort, and control cohort by performing Pearson’s chi-squared test and 2-sample t tests to test continuous variables such as age distribution. We calculated the incidence density rate of dementia (person-years) for each subgroup and conducted univariate and multivariate Cox proportional hazard regression analyses to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) of the risk of dementia. The multivariate models were adjusted for age, gender, and comorbidities (see subsection 2.3). We used the Kaplan–Meier method to assess the cumulative incidence of dementia between the two cohorts, and the log-rank test to test the differences.
Results
We enrolled 4108 ARHL patients and 4013 controls. Frequency matching ensured that age and sex distribution was similar in both groups. The prevalence of dementia, CLD, RA, HTN, DM, stroke, head injury, and CKD was higher in the ARHL cohort than in the control cohort (Table 1).
Table 2 lists the incidences and HRs for dementia and related risk factors. Risk of dementia increased with age [range of adjusted HR (aHR) = 1.00–7.00]. Compared with the control cohort, the risk of dementia was significantly higher in the ARHL cohort (aHR = 1.30, 95% CI 1.14–1.49). Patients with comorbidities exhibited a 3.57-fold higher risk of developing dementia compared with patients without comorbidities (95% CI 2.18–5.87). ARHL remained independently associated with dementia after adjustment for multiple dementia risk factors, including age, sex, and comorbidities (Table 2). Our results also revealed that female patients with ARHL were at higher risk of dementia than were male patients (aHR = 1.17, 95% CI 1.01–1.34).
The overall incidence rate of dementia was approximately 1.33 per 100 person-years for the control group and 1.76 per 100 person-years for the ARHL group (Table 3). In the multivariate analysis, age was treated as a continuous variable. We found that the risk of dementia was significantly higher in the ARHL cohort (adjusted HR = 1.29, 95% CI 1.13–1.48). The incidence rate of dementia increased with age. In the stratifications by sex and comorbidities, the risk of developing dementia was always higher in the ARHL cohort.
Figure 1 illustrates the Kaplan–Meier analysis results. The cumulative incidence curves for dementia were significantly higher in the ARHL cohort than in the control cohort (log-rank test P < 0.001).
Discussion
This study is considered the first nationwide population-based study using a matched cohort with a 10-year follow-up period to examine ARHL as a risk factor for dementia. The major discovery of our study was a higher incidence of subsequent dementia among the patients with ARHL, while oppositely in the first 2.5 years after diagnosis than among the patients with ARHL. In addition, we suggest that hearing impairments in older adults should be used as a marker for the early diagnosis of cognitive disorders such as dementia.
In a previous study, the incidence of dementia was found to double with every 5.9-year increase in age, from 3.1 per 1000 person-years at age 60–64 years to 175.0 per 1000 person-years at age >95 years [18]. An epidemiological study reported that women have higher rates of AD than men do [19]. Age, as well as diabetes, smoking, and cardiovascular disease are also known risk factors [20]. A longer-term cohort study found raised cholesterol and hypertension in midlife to be related to the onset of AD in later life [21]. In our study, female patients were at higher risk of developing dementia regardless of hearing loss, and comorbidities, such as CLD, RA, HTN, DM, stroke, head injury, and CKD, were potential risk factors for dementia in the ARHL group, but not in the control group (Table 1).
In the older population, hearing loss contributes relatively less to dementia than did well-known risk factors such as comorbidities and unmodifiable factors such as age (Table 2). However, the effect of hearing impairment on people with dementia is likely to be substantial combined with the frequency of other sensory impairments. Visual impairment has been shown to be associated with AD [6, 22]. The combined effect of visual and hearing impairments could have a severe debilitating effect on functional status.
Previous longitudinal studies have also shown a relationship between dementia and hearing loss. Peters et al. [15] found that, in patients with dementia, the decline in cognitive function was greater for those with impaired hearing. Further analyzing the diagnoses revealed that only in subjects with AD could hearing impairment be used to predict more rapid cognitive decline at follow-up [15]. In another longitudinal study, 836 older adults with hearing loss manifested an increased rate of dementia and more rapid decline on the mini-mental state examination scores than their non-hearing impaired counterparts [13]. Another investigation also revealed a clinically significant relationship between central auditory function and cognition test scores [5]. Hearing loss in older adults was found to be independently associated with poorer cognitive function, incident dementia, and falls. These findings suggest that hearing impairment may be an indicator for declined cognitive function in adults aged 65 years and older.
ARHL affects most people aged 65 years and older and represents the predominant neurodegenerative disease of aging. According to the World Health Organization, 278 million people worldwide experience moderate-to-profound hearing loss bilaterally (WHO 2010). There are currently 360 million people with disabling hearing loss (5.3% of the world’s population), and 91% of them are adults (http://data.worldbank.org/). Disabling hearing loss is currently defined as a loss of hearing greater than 40 dB HL (0.5–4 kHz) in the better-hearing ear. The following findings were drawn from a representative sample of older people in the Blue Mountains Hearing Study [23]: (1) According to four-frequency pure tone audiometry (PTA) testing, 39% of adults aged 55 or older have hearing loss; (2) the frequency of hearing loss almost doubles every 10 years of age among older adults, increasing from 10.5% in those aged under 60 years to approximately 80% in those aged 80 or older; and (3) Hearing loss occurs more frequently in men. Most people with hearing loss do not seek help. Risk factors for hearing loss include age, sex (male), DM, noise-exposure history, smoking, and impaired vision. In a cross-sectional study, a history of falls, HTN, broken hips, and heart disease were common among both hearing and visual impairment groups [24]. Age has the highest association with declining hearing loss [25]. Men decline as early as at the age of 30, while in women it occurs somewhat later [26]. Hearing levels differ between the sexes, with men having significantly poorer hearing at higher frequencies than women do [27].
Our results in Table 1 demonstrate that age, sex (male), DM, HTN, CLD, and stroke are risk factors for ARHL, whereas smoking (though higher in the ARHL group) is not a significant risk factor. Although one cross-sectional study found cardiovascular disease to be significantly related with the hearing status of older adults, the significance was stronger among women and for low frequencies [28]. Low-frequency presbycusis is typically associated with microvascular disease leading to atrophy of the stria vascularis [29]. Endothelial dysfunction and cardiovascular risk factors were reported highly related to sensory hearing loss [30].
The strengths of our study stem from the representative population-based cohort and large data sets. In the current longitudinal analysis, we found that ARHL may be used to predict the incidence of dementia in this population (Fig. 1). Our results revealed that, compared with the risk of patients without hearing loss, the patients diagnosed with hearing loss had, in the first 2.5 years after diagnosis, a significantly lower chance of dementia. This effect is probably related to delayed diagnosis of dementia in ARHL patients, and not to a lower risk of developing dementia. These findings have not been previously reported, which suggests that patients in the early stages of dementia may be ignored, neglected, or confused after hearing loss was noted in advance. Early signs of dementia, such as memory impairment, slow reaction time, and mild cognitive dysfunction, may be mistaken as a consequence of ARHL in outpatient clinic. Obvious symptoms of dementia as the illness progresses are easier to identify and diagnose. Our findings must be interpreted with caution because the small sample of patients with dementia at follow-up limited the statistical power of our results. In addition, because we used a survivor cohort, there could have been an underestimation of the number of new cases with impaired hearing.
We hypothesized that the processes of dementia and hearing loss are closely related; age-related changes in circulating levels of glucocorticoid and the hypothalamus–pituitary–adrenal (HPA) axis could act in combination with the processes underlying ARHL, thus resulting in the further worsening of dementia. In particular, hippocampal damage may cause HPA axis disturbances, which have been reported in patients with dementia [31, 32]. Furthermore, dementia has been associated with chronic neuroinflammation [33–35]. Neuroinflammation induces glucocorticoid resistance [36, 37]. Notably, HPA and glucocorticoid resistance have been associated with sensorineural hearing loss [38, 39]. Thus, ARHL may increase the risk of dementia by disturbing the HPA axis and glucocorticoid resistance. We found that age was the most crucial risk factor for dementia (Table 2), followed by comorbidities, hearing loss, and gender.
However, the relatively small number of patients in the matched 10-year follow-up cohort presented a limitation. Therefore, changes in dementia over time could have been underestimated due to the lack of statistical power. Another limitation was that our study was a longitudinal study with diagnoses collected only from the NHIRD, risking potential bias resulting from differing diagnosis standards among individual clinicians. We identified patients with hearing loss in the NHIRD according to ICD-9-CM codes and pure tone audiometry (PTA) results were not available in NHIRD. Thus, the actual severity of hearing loss as a risk factor for subsequent dementia was not explored. An additional limitation was the lack of other demographic variables such as socioeconomic status, years of education, mood status, living arrangement, occupation, noise-exposure history, lifestyle, and family medical history, which could have provided useful information regarding other potential risk factors for hearing loss and dementia. Diagnosis of dementia has been known a big challenge for clinicians due to some unspecified symtpoms and different etioloigies. The disease is usually finally confirmed in specialist clinics. Since Data like MMSE and CDR are not available in NHIRD. In our study, we therefore narrowed the group and only selected dementia patient (ICD-9-CM codes 290, 294.1 and 331.0–331.2) with at least 3 times within 4 months and diagnosed by psychiatrists. Finally, this study used an observational design rather than an experimental one. Data on the relationship between the severity of dementia and severity (and frequency range) of hearing loss were unavailable.
Conclusion
Current recommendations for patients with ARHL include regular exams to monitor changes in PTA. As our study indicates, evidence of a possible link between ARHL and dementia exists. Physicians should be more alert of early signs of dementia which may be mistaken as a sequence for ARHL following the first 2 years of diagnosis and pay more attention to those constituing the group of high-risk dementia. These findings can potentially be used to modify the treatment of patients suffering from ARHL, especially in the first 2 years following diagnosis. Clinicians may inquire about cognitive function during preventive care protocol and could refer patients to a cognitive specialist for further evaluation and maintain their cognitive ability if a cognitive decline is reported.
References
Cappe C, Rouiller EM, Barone P (2009) Multisensory anatomical pathways. Hear Res 258:28–36
Roth TN (2015) Aging of the auditory system. Handb Clin Neurol 129:357–373
Reitz C, Mayeux R (2014) Alzheimer disease: epidemiology, diagnostic criteria, risk factors and biomarkers. Biochem Pharmacol 88:640–651
Gates GA, Gibbons LE, McCurry SM, Crane PK, Feeney MP, Larson EB (2010) Executive dysfunction and presbycusis in older persons with and without memory loss and dementia. Cogn Behav Neurol 23:218–223
Gates GA, Anderson ML, Feeney MP, McCurry SM, Larson EB (1996) Central auditory dysfunction, cognitive dysfunction, and dementia in older people. Arch Otolaryngol–Head Neck Surg 122:161–167
Kerbage C, Sadowsky CH, Jennings D, Cagle GD, Hartung PD (2013) Alzheimer’s disease diagnosis by detecting exogenous fluorescent signal of ligand bound to Beta amyloid in the lens of human eye: an exploratory study. Front. Neurol 4:62
Dubno JR, Ahlstrom JB, Horwitz AR (2008) Binaural advantage for younger and older adults with normal hearing. J Speech Lang Hear Res 51:539–556
Kurniawan C, Westendorp RG, de Craen AJ, Gussekloo J, de Laat J, van Exel E. (2012) Gene dose of apolipoprotein E and age-related hearing loss. Neurobiol Aging 33:2230 e2237–2230 e2212.
Lin FR (2011) Hearing loss and cognition among older adults in the United States. J Gerontol A Biol Sci Med Sci 66:1131–1136
Teipel S, Fritze T, Ovari A, Buhr A, Kilimann I, Witt G, Pau HW, Doblhammer G (2015) Regional pattern of dementia and prevalence of hearing impairment in Germany. J Am Geriatr Soc 63:1527–1533
Uhlmann RF, Larson EB, Rees TS, Koepsell TD, Duckert LG (1989) Relationship of hearing impairment to dementia and cognitive dysfunction in older adults. JAMA 261:1916–1919
Granick S, Kleban MH, Weiss AD (1976) Relationships between hearing loss and cognition in normally hearing aged persons. J Gerontol 31:434–440
Gurgel RK, Ward PD, Schwartz S, Norton MC, Foster NL, Tschanz JT. (2014) Relationship of hearing loss and dementia: a prospective, population-based study. Otol Neurotol 35:775–781.
Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, Satterfield S, Ayonayon HN, Ferrucci L, Simonsick EM; Health ABC Study Group (2013) Hearing loss and cognitive decline in older adults. JAMA Intern Med 173:293–299.
Peters CA, Potter JF, Scholer SG (1988) Hearing impairment as a predictor of cognitive decline in dementia. J Am Geriatr Soc 36:981–986
Gates GA, Beiser A, Rees TS, D’Agostino RB, Wolf PA (2002) Central auditory dysfunction may precede the onset of clinical dementia in people with probable Alzheimer’s disease. J Am Geriatr Soc 50:482–488
Gates GA, Anderson ML, McCurry SM, Feeney MP, Larson EB (2011) Central auditory dysfunction as a harbinger of Alzheimer dementia. Arch Otolaryngol–Head Neck Surg 137:390–395
Kaplan W, Wirtz, V.J., Mantel-Teeuwisse, A. (2013) A Public Health Approach to Innovation. Priority medicines for Europe and the World. 2013 Update: World Health Organization 2013.
Alzheimer’s A. (2014) Alzheimer’s disease facts and figures. Alzheimer’s Demen 10:e47–92.
Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM (1999) Diabetes mellitus and the risk of dementia: the Rotterdam Study. Neurology 53:1937–1942
Kivipelto M, Helkala EL, Laakso MP, Hänninen T, Hallikainen M, Alhainen K, Soininen H, Tuomilehto J, Nissinen A (2001) Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ 322:1447–1451
Chang LY, Lowe J, Ardiles A, Lim J, Grey AC, Robertson K, Danesh-Meyer H, Palacios AG, Acosta ML (2014) Alzheimer’s disease in the human eye. Clinical tests that identify ocular and visual information processing deficit as biomarkers. Alzheimer’s Demen 10:251–261.
Mitchell P, Gopinath B, Wang JJ, McMahon CM, Schneider J, Rochtchina E, Leeder SR (2011) Five-year incidence and progression of hearing impairment in an older population. Ear Hear 32(2):251–257
Crews JE, Campbell VA (2004) Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health 94:823–829
Cruickshanks KJ, Tweed TS, Wiley TL, Klein BE, Klein R, Chappell R, Nondahl DM, Dalton DS (2003) The 5-year incidence and progression of hearing loss: the epidemiology of hearing loss study. Arch Otolaryngol Head Neck Surg 129:1041–1046
Pearson JD, Morrell CH, Gordon-Salant S, Brant LJ, Metter EJ, Klein LL, Fozard JL (1995) Gender differences in a longitudinal study of age-associated hearing loss. J Acoust Soc Am 97:1196–1205
Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, Nondahl DM (1998) Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin. The Epidemiology of Hearing Loss Study. Am J Epidemiol 148:879–886
Gates GA, Cobb JL, D’Agostino RB, Wolf PA (1993) The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Arch Otolaryngol–Head Neck Surg 119:156–161
Schuknecht HF. (1964) Further observations on the pathology of presbycusis. Arch Otolaryngol 80:369–382.
Ciccone MM, Cortese F, Pinto M et al (Dec 2012) Endothelial function and cardiovascular risk in patients with idiopathic sudden sensorineural hearing loss. Atherosclerosis 225(2):511–516
Bao AM, Meynen G, Swaab DF (2008) The stress system in depression and neurodegeneration: focus on the human hypothalamus. Brain Res Rev 57(2):531–553
Leonard BE (2007) Inflammation, depression and dementia: are they connected? Neurochem Res 32:1749–1756
Zhang J (2015) Mapping neuroinflammation in frontotemporal dementia with molecular PET imaging. J Neuroinflammation 12:108
Holmgren S, Hjorth E, Schultzberg M, Lärksäter M, Frenkel D, Tysen-Bäckström AC, Aarsland D, Freund-Levi Y (2014) Neuropsychiatric symptoms in dementia-a role for neuroinflammation? Brain Res Bull 108:88–93
Reale M, Brenner T, Greig NH, Inestrosa N, Paleacu D. (2010) Neuroinflammation, AD, and dementia. Int J Alzheimers Dis 2010: 974026.
Marques AH, Silverman MN, Sternberg EM (2009) Glucocorticoid dysregulations and their clinical correlates. From receptors to therapeutics. Ann N Y Acad Sci 1179:1–18
Silverman MN, Sternberg EM (2012) Glucocorticoid regulation of inflammation and its functional correlates: from HPA axis to glucocorticoid receptor dysfunction. Ann N Y Acad Sci 1261:55–63
Simoens VL, Hebert S (2012) Cortisol suppression and hearing thresholds in tinnitus after low-dose dexamethasone challenge. BMC Ear Nose Throat Disord 12:4
Choung YH, Park K, Shin YR, Cho MJ (2006) Intratympanic dexamethasone injection for refractory sudden sensorineural hearing loss. Laryngoscope 116:747–752
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study is supported by grants of from the Ministry of Science and Technology of Taiwan (MOST103-2314-B-715-001-MY2, MOST104-2314-B-715 -003 -MY3), Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW104-TDU-B-212-113002), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM104010092), NRPB Stroke Clinical Trial Consortium (MOST 103-2325-B-039 -006), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. Part of this article was prepared on the basis of our studies supported by intramural research grants from Mackay Medical College (MMC1012A10, MMC1012B13).
Conflict of interest
Every author declares that he/she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. The NHIRD contains only encrypted patient information; it provides anonymous identification numbers and corresponding claims information, including gender, date of birth, administered medical services, and prescriptions given. Patient consent is not required to access the data stored in NHIRD. This study was approved by the Institutional Review Board (IRB) of China Medical University Hospital (CMUH104-REC2-115). The IRB waived the consent requirement.
Rights and permissions
About this article
Cite this article
Su, P., Hsu, CC., Lin, HC. et al. Age-related hearing loss and dementia: a 10-year national population-based study. Eur Arch Otorhinolaryngol 274, 2327–2334 (2017). https://doi.org/10.1007/s00405-017-4471-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4471-5