Abstract
We herein report our experience with the management of laryngoceles using transoral robotic surgery (TORS). A bicentric retrospective study was conducted from November 2009 to September 2015. The inclusion criteria were treatment of a laryngocele by TORS and no malignancy on definitive histopathology. Surgery was performed using the Da Vinci (Intuitive®) surgical robot. Surgical methods and post-operative outcomes were evaluated. Eight patients (four men and four women) presenting with a laryngocele (one bilateral case) were included (mean age 61.8 years). There was one covering tracheotomy. The average post-operative stay was 3.75 days. Three patients treated for a combined laryngocele had a nasogastric feeding tube inserted for 5 days. One patient experienced late laryngeal bleeding that required surgical treatment. TORS may offer an efficient treatment option for laryngoceles. The use of precise and flexible instruments and a three-dimensional camera allow fine dissection of these tumours, preserving the glottic space and vocal function, even for combined laryngoceles extending deep within the neck.
Evidence level: 4.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current indications for transoral robotic surgery (TORS) are stage T1–T2 malignancies and benign tumours of the oropharynx, hypopharynx, and supraglottic larynx [1–3]. Laryngoceles are benign lesions that develop on the laryngeal saccules [4]. They consist of outpouchings of the laryngeal ventricle of Morgagni [5, 6]. There are three types of laryngoceles: internal laryngoceles (IL), which are strictly intra-laryngeal; external laryngoceles; and combined laryngoceles (CL), which extend through the thyrohyoid membrane [7]. The classic presentation includes dysphonia and, sometimes, lateral cervical swelling when the intra-laryngeal pressure increases, as often seen in wind instrument players [8]. Laryngoceles may also occur after laryngeal or cervical surgery [9]. When communication with the intra-laryngeal lumen is absent, the laryngocele fills with mucus to become a laryngomucocoele. Acute dyspnoea can occur in the presence of an infection (laryngopyocoele) [10]. Several surgical techniques have been introduced: marsupialisation, laser endoscopy, cold steel surgery, external surgery, and now TORS. Over time, surgical procedures have shifted toward minimally invasive techniques. The first case of a laryngocele treated with TORS was in 2013 [11]. This new approach provides an excellent view of the tumour and enables the use of flexible instruments to achieve easier dissection. In this study, we present a series of consecutive patients with IL or CL treated by TORS, and discuss the advantages and limitations of this new approach.
Patients and methods
Patients
This retrospective, bicentric study was conducted from 1 November 2009 to 15 September 2015. All patients with a laryngocele treated by TORS were included. TORS operability was evaluated from the start of the procedure, at the time the robotic retractor was inserted. The pre-operative assessment consisted of a clinical examination of the aerodigestive tract by nasal fibroscopy. The radiological assessment included head and neck computed tomography (CT) using a contrast agent (Fig. 1). The biological pre-anaesthetic assessment, consisting of at least a coagulation test, was adjusted with regard to the patient’s comorbidities.
Surgical technique
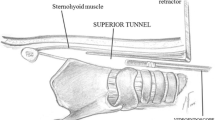
Each patient was placed in the supine position with extension of the neck. All of the procedures were performed under general anaesthesia and nasotracheal intubation. A tracheal tube of small diameter (5.0 or 5.5 mm) was placed in the posterior commissure of the larynx to achieve optimal exposure of the epilarynx. An M retractor (MicroFrance®) was positioned carefully to obtain optimal exposure of the laryngocele. The Boyles–Davis mouth gag was used in one case experiencing exposure difficulties with the M retractor. The retractor was released every 30 min to avoid lingual ischaemia and post-operative oedema. The robot was positioned to the left of the patient; its arms were equipped with a three-dimensional (3D) camera (central arm), a 5-mm monopolar spatula (for cutting), and an 8-mm Maryland bipolar forceps. The endoscope diameter was 8 or 12 mm, with an angle of either 0° or 30°. A 30° angle provided optimum visibility of the anterior portion of the laryngeal vestibule. The time to complete the installation was referred to as the “docking” time. The time which the surgeon spent at the console was considered to be the effective surgical time. The mucosa of the laryngeal vestibule was incised until the wall of the laryngocele was visible (Fig. 2). The vascular pedicle of the right aryepiglottic fold was carefully cauterised using Maryland bipolar forceps before being sectioned. No clamps were used. Dissection of the laryngocele was performed gradually, from top to bottom, up to the laryngeal saccule. For CL, the flexibility of the robotic instruments allowed lateral dissection deep into the neck. In these cases, it was also necessary to burst the cyst and to aspirate its contents to decrease the volume of the tumour. The entire laryngocele pouch was removed, and no simple marsupialisation was performed. The wound was left to heal, and the vocal folds were carefully preserved.
The variables evaluated were demographic characteristics (age and sex), pre-operative assessments (clinical manifestations and imaging assessments), peri-operative assessments (surgical technique, type of retractor, docking time, surgical time, and need for a nasogastric tube or tracheotomy), and post-operative assessments (definitive anatomopathology report, complications, refeeding, and hospitalisation time).
Results
Eight patients were included in this study, three with CL and five with IL. One patient underwent laser surgery 7 years earlier for marsupialisation, and one patient was treated by an external approach and five marsupialisation procedures. Both patients were admitted for laryngocele recurrence. One patient had bilateral IL; to avoid the risk of major laryngeal oedema, the right IL was operated on 6 months after the left one. Among the nine laryngoceles evaluated, six were air-filled (four IL and one CL) and three were laryngomucocoeles (one IL and two CL). The main identifying symptoms were dysphonia (n = 5), laryngeal dyspnoea (n = 3), and dysphagia due to infection (n = 1). The average age was 61.8 (50–84) years. The patients comprised four men and four women (sex ratio 1:1) (Table 1). None of the patients underwent endoscopy under general anaesthesia prior to the procedure. The CT scan was sufficient for characterisation of the tumour and its extension (CL), or lack of extension (IL), through the thyrohyoid membrane.
The average length of the tumour was 2.9 (1.5–6) cm as determined by CT. All tumour excisions were complete. The average docking time was 17.5 (5–45) min. The average time spent at the console was 55 (30–150) min. Tumour exposure using the retractor was consistently satisfactory. The average hospitalisation time was 5 (1–10) days: only 3 days for IL and 6 days for CL. The average follow-up time was 19.7 (1–68) months. One covering tracheotomy was inserted in the patient who experienced five recurrences and then removed on day 4. All patients with IL were fed orally the day of surgery. The three patients with CL were fed via a nasogastric tube for 5 days. One experienced bleeding on day 11 after the operation and required endoscopic coagulation. No recurrence was observed.
Discussion
This study demonstrated the efficiency of TORS for the treatment of laryngoceles in terms of tumour exposure, visibility of the surgical site, and complete removal of the tumour, even a CL. The key to successful resection is adequate exposure. Before scheduling a TORS procedure, an initial endoscopy is recommended to assess the exposure of the pharyngolaryngeal area. We always perform this step for malignant tumours. For patients with benign tumours, such as laryngoceles, we prefer not to perform general anaesthesia twice. The patients were aware that an external approach may be required in the case of exposure difficulty. No such situation occurred in our series. It requires time and patience to position the mouth retractor properly, considering its ability to move in three dimensions and differing anatomies among patients. The choice of the retractor depends on its availability and the surgeon’s preference and practical experience. If exposure is not achieved with one retractor, it may be obtained with another.
IL are usually managed using endoscopic CO2 laser surgery or cold microsurgical instruments, but Zelenik et al. [12] found a higher risk of haemorrhage using cold instruments. The introduction of these procedures has reduced the indications for a cervical approach and the inherent vascular and neurological complications. Endoscopic microsurgery has been adapted for the removal of IL and the marsupialisation of laryngomucocoeles. In our experience, marsupialisation is not considered a sustainable treatment, because it presents a potential risk of early recurrence onset. In our series, two patients were treated for recurrence after marsupialisation had been performed in another hospital. TORS enables removal of IL and CL if exposure of the laryngeal vestibule is adequate. The 30° oriented camera and the flexibility of the instruments allow deep and visually controlled resection of CL. Ciabatti et al. [11] described one case of CL treated successfully by TORS. With regard to bleeding complications, the Maryland bipolar forceps allow very precise cauterisation during the procedure. Unfortunately, we had one patient who required endoscopic cauterisation for late bleeding on day 11. The risk of this complication is comparable between TORS and other techniques. Table 2 includes data from several studies, regarding the laryngocele type, outcome, and follow-up. CL and external laryngoceles are usually managed by a cervical approach, because endoscopic CO2 laser surgery is less suitable for accessing the deep lateral portion of the cyst [13]. Several open techniques are used: thyrotomy with resection of the upper third of the thyroid cartilage, type V thyrotomy, access via the thyrohyoid membrane [12], and lateral thyrotomy [15]. Inevitably, these procedures result in cervical scars and a higher risk of nerve injury. In their meta-analysis of 71 laryngoceles, Zelenik et al. [12] showed that 17.5 % of patients required a tracheotomy (11/63): 5 (8 %) during surgery as a safety procedure and 6 (9.5 %) before excision surgery as a vital procedure.
In our series, the patients were discharged after 5 (1–10) days on average: 6 days for patients with CL and 3 days for those with IL. According to Devesa et al. [15], the duration of hospitalisation after CO2 laser resection of the laryngocele (nine internal, one external, and two combined cases) was 1.8 (1–4) days. Resumption of feeding was prompt, and no nasogastric tubes were used; however, two tracheotomies were performed. In our series, the three patients with CL required nasogastric feeding to limit the post-operative pain experienced with swallowing. In one case, a covering tracheotomy was performed due to the high risk of post-operative laryngeal oedema. The average CL size in our series was 6 cm. To avoid difficulty with swallowing resulting from the large wound, we opted to use a nasogastric tube in these three patients. After the procedures for the six IL cases, the patients resumed eating the same evening, without pulmonary aspiration.
The introduction of TORS has broadened the indications for transoral surgery, particularly for CL inaccessible by laser. In this study, increased exposure of the surgical field was achieved by the specific retractors used and the 3D camera’s magnification capabilities. The precision and flexibility of the instruments are definite assets compared with the other endoscopic techniques.
The limitations of our study are related to the small number of patients. TORS is still expensive and not widely available. Moreover, the robot was not initially designed for ear, nose, and throat surgery; technical improvements and new robotics systems will optimise the use of TORS for such procedures. Multicentre studies are needed to increase patient numbers and confirm these encouraging results.
References
McLeod IK, Melder PC (2005) Da Vinci robot-assisted excision of a vallecular cyst: a case report. Ear Nose Throat J 84:170–172
Haus BM, Kambham N, Le D, Moll FM, Gourin C, Terris DJ (2003) Surgical robotic applications in otolaryngology. Laryngoscope 113(7):1139–1144
Genden EM, O’Malley BW, Weinstein GS, Stucken CL, Selber JC, Rinaldo A et al (2012) Transoral robotic surgery: role in the management of upper aerodigestive tract tumors. Head Neck 34(6):886–893
Hubbard C (1987) Laryngocele—a study of five cases with reference to the radiological features. Clin Radiol 38:639–643
Lacau St Guily J, Susini B, El-Charter P, Torti F, Périé S (2006) Tumeurs bénignes du larynx. Oto-rhino-laryngologie 20-700-A-10. doi:10.1016/S0246-0351(06)41896-1
Matino SE, Martinez VV, Leon VX, Quer AM, Burgues VJ, De JM (1995) Laryngocele: clinical and therapeutic study of 60 cases. Acta Otorrinolaringol Esp 46(4):279–286
Fagan J (2014) Laryngocele: surgical management. Open Access Atlas of Otolaryngology, Head and Neck Operative Surgery. http://www.entdev.uct.ac.za. Accessed 28 June 2016
da Pinho MC et al (2007) External laryngocele: sonographic appearance—a case report. Radiol Bras 40(4):279–282
Marom T, Roth Y, Cinamon U (2010) Laryngocele: a rare long-term complication following neck surgery? J Voice 25(3):272–274
de Paula Felix JA, Felix F, de Mello LFP (2008) Laryngocele: a cause of upper airway obstruction. Rev Bras Otorrinolaringol 74(1):143–146
Ciabatti PG, Burali G, D’Ascanio L (2013) Transoral robotic surgery for large mixed laryngocele. J Laryngol Otol 127(4):435–437
Zelenik K, Stanikova L, Smatanova K, Cerny M, Kominek P (2014) Treatment of laryngoceles: what is the progress over the last two decades? Bio Med Res Int 2014:6
Crozat-Teissier N, Van Den Abbeele T (2005) Malformations congénitales du larynx. Oto-rhino-laryngologie 20-631-1-9. doi:10.1016/S0246-0351(05)23971-5
Saha D, Sinha R, Pai RR, Kumar A, Chakraborti S (2013) Laryngeal cysts in infants and children—a pathologist’s perspective. Int J Pediatr Otorhinolaryngol 77:1112–1117
Curti Thomé D, De La Cortina R (2000) Lateral thyrotomy approach on the paraglottic space for laryngocele resection. Laryngoscope 110:447–450
Devesa PM, Ghufoor K, Lloyd S, Howard D (2002) Endoscopic CO2 laser management of laryngocele. Laryngoscope 112:1426–1430
Acknowledgments
The English version of the manuscript was corrected by a native English speaker: Dylan Owen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
Sylvain Morinière, MD, Ph.D.: development of a TORS-specific retractor with Micro France enterprise.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Inform consent
All the patient in this study had sign an inform consent according to French laws.
This article does not involve any studies using animals.
Rights and permissions
About this article
Cite this article
Villeneuve, A., Vergez, S., Bakhos, D. et al. Management of laryngoceles by transoral robotic surgery. Eur Arch Otorhinolaryngol 273, 3813–3817 (2016). https://doi.org/10.1007/s00405-016-4171-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4171-6