Abstract
To determine if there was a difference in the inflammatory reaction after tonsil surgery with “traditional” techniques (tonsillectomy and adenoidectomy or TA) compared to partial intracapsular tonsillectomy and adenoidectomy (PITA). Design: Randomized, double-blind study. Setting: tertiary care academic hospital. Children under the age of 16 years with a diagnosis of obstructive sleep disordered breathing were randomly allocated into three study groups: TA with electrocautery (n = 34), PITA with CO2 laser (n = 30) and PITA with debrider (n = 28). All of the children underwent adenoidectomy with a current at the same surgical procedure. Main outcome measure: c-reactive protein level (CRP) was the primary endpoint. In addition, the following were assessed: white blood cells (WBC), neutrophils (NEU), interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). Pre- and post-procedure measurements were compared between the groups. Parents filled out a questionnaire daily during the first postoperative week assessing pain, swallowing and snoring. CRP levels ascended higher in the PITA groups after surgery (p = 0.023), WBC and NEU showed the same pattern, IL-6 levels were higher in PITA group and there was no difference in TNF-alpha levels between the two types of procedures. Postoperative pain and postoperative hemorrhage were significantly lower in the PITA groups as compared to the TA group (p = 0.01 and 0.048). PITA in comparison to TA is associated with lower morbidity; however, the inflammatory response does not differ significantly in the first 24 h after surgery. Additional long-term studies assessing efficacy of PITA are warranted. Level of evidence: Level 1, prospective randomized controlled trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tonsillectomy is one of the most common surgeries performed in children. It is usually performed in children with obstructive sleep disordered breathing (OSDB) [1, 2]. Conventional tonsillectomy (TA) implies the complete removal of the tonsil by anatomic dissection between the tonsillar capsule and the superior constrictor muscle. Until recently this has been the standard procedure used for OSDB.
Lately, many otolaryngologists have begun to perform a partial intracapsular tonsillectomy (PITA) for OSDB, preserving the tonsil capsule and a rim of tonsillar tissue, thus avoiding damage to the pharyngeal muscles. Over the last few years PITA has been advocated as an equally effective and a safer procedure than TA combined with Adenoidectomy in treatment of OSDB [3]. There are several studies showing both short- and long-term effectiveness of PITA, suggesting that patients undergoing PITA experience less pain, with comparable relief of OSDB [3–12] when compared to those underoing TA. Studies evaluating postoperative pain are typically based on questionnaires which are subjective. In addition the pain in younger children is evaluated by the caregivers and hence, may be subject to a misclassification bias.
This study examined the influence of the surgical technique on the postoperative inflammatory processes using inflammatory markers that can provide more objective data regarding pain.
Several studies in other medical disciplines, such as gynecology [13], urology [14] and general surgery [16] have shown a correlation between the extent of surgical intervention and an immediate increase in the level of inflammatory cytokines (IL-6 and TNF-α).
We hypothesized that partial intracapsular tonsillectomy is associated with a minor inflammatory response when compared to that in conventional tonsillectomy, as the muscles of the tonsillar bed are not disturbed. Likewise, we assumed that postoperative pain is an expression of inflammation, and therefore the PITA patients should experience less pain when compared to TA patients.
The main objective of the current study was to evaluate C-reactive protein (CRP) levels after PITA procedure compared with levels after the “traditional” tonsillectomy. The secondary objectives were: (1) to compare the levels of other post-operative inflammatory mediators, i.e. WBC, NEU, IL-6 and TNF-α in between the three groups; and (2) to compare post-operative morbidity and OSDB improvement between the three groups in the short-term postoperative period.
Methods
We conducted a randomized controlled trial (RCT).
The study was double-blind; the patients and caregivers did not know before surgery until the first appointment (7 days after surgery) what type of surgery would be performed and the lab technicians performing the testing were not aware of the group assignment. The study population was defined as children 2–10 years old who underwent surgery for OSDB at the Soroka University Medical Center (SUMC)—the tertiary hospital in the Southern Israel. The children’s caregivers were approached by the study personnel, who provided a full explanation of the study objectives and procedures in their preferred language. Patients were considered eligible if there was a clinical history of OSDB (snoring and apneas) and if physical exam showed tonsil size to be +3 according to Brodsky grading [16] or more (extending past halfway between the anterior pillar and the uvula) with enlarged adenoids as seen either by endoscopy or X-ray. Some of the children underwent polysomnography (PSG) before the operation, as ordered by the treating physician and an attempt was made to obtain a PSG 3–6 months after surgery.
The caregivers signed an informed consent form prior to the procedure. We excluded children with a history of recurrent tonsillitis and peritonsillar abscess, where a partial tonsillectomy may not be appropriate in addition. Patients with craniofacial abnormalities or neuromuscular disorders were also excluded.
Treatment
The eligible patients were randomly assigned into the three study groups: laser partial tonsillectomy with adenoidectomy (LPITA), microdebrider partial tonsillectomy with adenoidectomy (DPITA) and standard tonsillectomy using electrocautery dissection of the tonsils with adenoidectomy (TA). Operation techniques: the operations were performed by four experienced otolaryngologists. Operations in the LPITA group were performed with a hand held CO2 laser (Sharplan 40C, Israel), power of 15–18 W was applied to the tonsil for ablation in a continuous mode. Minor bleeding was treated by lengthening the distance so that the beam was defocused. The tonsillar tissue was ablated laterally, up to the level of the pillars.
DPITA was performed with a microdebrider (Medtronic Xomed, USA). Hemostasis was performed with local pressure and bipolar (15 W) in cases of more significant or refractory bleeding.
In DPITA and LPITA a small part of tonsillar tissue around the tonsillar capsule was left intact.
TA was performed by complete removal of tonsils with the capsule, with monopolar electrocautery dissection, with a maximum intensity of 15 W and hemostasis was achieved with bipolar cautery of 15 W.
Adenoidectomy was performed in the same manner in all children with a curette and hemostasis was achieved by temporary packing of the nasopharynx.
Randomization
The randomization was performed into three groups in four strata of age 2–4, 4–6, 6–8, 8–10.
Endpoints
The primary endpoint was defined as post-procedure measurement of CRP levels. The other inflammatory markers measured in blood were: WBC, NEU, IL-6 and TNF-alpha. These biomarkers were measured prior to, and within 24 h post-procedure.
Data collection
The demographic information was recorded based on the hospital charts. The children’s caregivers received a self-administered questionnaire on the severity of the postoperative pain and snoring, which they were requested to fill out daily during the first week after the procedure. The questionnaire included questions regarding pain, difficulty swallowing, use of analgesics and evaluation of snoring on a scale of 1–5.
Cytokine measures
Samples were analyzed for IL-6 levels (High Sensitivity ELISA kit; R&D Systems, Inc. Minneapolis, MN) and TNF-α levels (High Sensitivity ELISA kit; Ebioscience, San Diego, CA, USA), in the lab directed by one of the authors (AG). All samples were assayed in duplicates, at two dilutions, at plate reader absorbance (450 nm for all assays). Results were analyzed with a 4-parameter logistic curve fit. The intra-assay and inter-assay variability were <10 %; specificity ranged from 94 to 98 %.
C-reactive protein levels (CRP) were measured in the immunology laboratory of SUMC (immunonephelometry method) and the complete blood count (CBC) tests were performed in the hematology laboratory of SUMC.
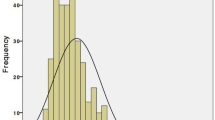
Statistical methods
General approach: continuous variables were presented as mean ± standard deviation (SD), median, minimum and maximum. Comparison between the groups of treatment used analysis of variance (ANOVA) or Wilcoxon test, depending on their distribution. Categorical variables were presented as proportions out of available cases and were compared between the study groups using Chi-square test.
In the primary analysis the post-procedural measurements of CRP levels were compared between the two PITA procedures and TA procedure using the one-sided Wilcoxon test.
The post-procedural measurements of inflammatory mediators were compared between the study groups using linear regression models, with their log-transformed values as a dependent variable and the group indicator and their corresponding baseline log-transformed measurement of CPR, IL6 and TNF alpha levels as independent variables in the model. Besides the primary analysis—all the comparisons were performed with a two-sided test and considered significant at the significance level below 0.05.
Analysis was performed according to the intention to treat (ITT) categories, assigned at randomization.
Sample size calculation
The study was designed to detect the difference of 0.5 (UNITS) in CRP post-procedure measurements between the 2 PITA groups compared with conventional TA technique with 92 evaluable subjects, 58 subjects in the 2 PITA groups and 34 in TA group, assuming the standard deviation of CRP equal 1 [UNITS], the one-sided t test with significance level of 5 % would yield the power of 84.35 %. The power was expected to decrease to 80 % as a result of using the non-parametric Mann–Whitney test in the primary analysis (by an efficiency coefficient equal 0.955) [17]. To ensure 92 subjects eligible for analysis and expecting 8 % of lost-to-follow-up 1 week after procedure, we planned to enroll 100 subjects.
Results
In all 110 children meeting the inclusion and exclusion criteria were defined eligible for the study (see Fig. 1). 100 (90 %) of the screened patients signed the informed consent form prior to enrollment. The treatment was changed intraoperatively in five children. The main reasons for changing the treatment were technical problems either with the debrider or the laser. All children were analyzed according to the designated treatment on as intention to treat analysis.
Out of 92 children enrolled in the study (Table 1) 30 patients were randomly assigned into the LPITA group, 28 to the DPITA group and 34 to the TA group. The mean age was 4.0 ± 1.9 years, with the youngest child enrolled being at the age of two and the oldest 10 years. Sixty-three percent (63 %) of study population were males. These parameters did not vary between the three study groups.
Table 2 presents the assessment of the caregivers during 7 days after surgery. All three items related to pain (pain, swallowing and pain medication) were significantly better in the PITA group. There was no difference between DPITA and LPITA regarding pain parameters. Snoring as reported by the caregiver immediately after surgery did not differ between the groups.
The levels of CRP at baseline varied between the study groups (p value = 0.020) and following the surgery the CRP levels increased in all groups (Table 3). The CRP in the PITA group was on average lower than that in the tonsillectomy group (1.29 ± 1.19 vs. 1.57 ± 1.48; however, this comparison did not show a statistically significant result (p value = 0.171 in the one-sided Wilcoxon test).The difference between the study groups was recorded only after adjustment to baseline CRP levels (p value = 0.023). As seen in Table 3, WBC and neutrophils differed significantly between the PITA groups and the TA group. IL-6 levels on the other hand were higher in PITA group. There was no difference in postoperative TNF-alpha levels between the groups. The degree of immediate postoperative snoring was similar between the groups.
Postoperative bleeding differed significantly between the groups (p = 0.048). No bleeding occurred in the DPITA and LPITA groups (0/60) while three patients from the TA group suffered delayed postoperative bleeding (3/34) (data not shown). All three patients who bled were treated conservatively and did not require repeated surgery.
We were able to obtain PSG after surgery for a small proportion of the patients because many of the caregivers thought it was not necessary after the child was “cured”. Altogether eight patients in the DPITA group, eight in the LPITA group and ten in the TA group had a postoperative sleep study. The preoperative Apnea–Hypopnea Index (AHI) of the DPITA group was lower than that in the other two groups (DPITA, 6.13 ± 4.92/h, TA, 9.16 ± 5.30/h, LPITA, 10.06 ± 6.74/h). All patients, except one in LPITA group and two in TA group, had a final AHI less than 5/h. There were no significant differences between the pre and the postoperative decrease in AHI between the groups (Table 3).
Discussion
We attempted to assess the difference in inflammation, as measured by CRP levels (main objective) between patients undergoing PITA (two variants) and those undergoing TA. The planned univariate analysis showed no statistically significant difference between the two groups as shown in Table 3 (p value = 0.171), whereas an analysis adjusting to the varying baseline levels (linear regression) showed that the CRP levels in the PITA group were 0.87 times less compared to those of the TA group (p value = 0.023). This finding is consistent with a lower degree of inflammation recorded in the PITAs group as estimated by other inflammatory mediators (white blood cells, neutrophis).
Several retrospective studies have been done in the past comparing postoperative complications of tonsil surgery between different surgical methods. To the best of our knowledge this is the only study, prospectively and randomly, comparing both short-term clinical outcomes including bleeding, pain snoring and inflammatory responses after tonsil surgery.
Tonsillectomy carries significant morbidity [3–12]. All patients suffer pain after surgery and often the pain is severe occasionally requiring hospitalization for dehydration.
The use of PITA has become more popular in the last decade. The rationale is that it causes less pain and bleeding post-operatively compared to “traditional” TA with comparable improvement in OSDB [3–12]. In this study we examined this claim prospectively, and attempted to examine in an objective fashion whether this is indeed the case.
The main argument against PITA has been a possible regrowth of the palatine tonsils which requires repeated surgery. The published rate of regrowth ranges from 0.5 to 0.9 % [19, 20] and up to 3.5 % [21]. In this study we did not assess the late results comparing PITA to TA but rather focused on early outcomes and immediate differences, following the use of these different operative techniques.
TA with electrocautery dissection shows a higher post-operative bleeding rate in comparison to cold dissection and it may be as high as 10 % [22]. PITA has been shown to cause less bleeding than TA [23]. It is well known that the most common complication of tonsillectomy is bleeding and up to 2 % of tonsil surgery patients require a second operation to control the bleeding [18]. Severe bleeding may cause shock and even death. When accounting for all bleeding and not just those who needed surgery there was up to 15 % post operative bleeding after tonsillectomy [24]. While keeping in mind the limitation of small groups, our study agrees with the previous reports, with a 9 % bleeding rate using TA versus 0 % in the PITA (p = 0.048). The lower hemorrhage rate of intracapsular tonsillectomy can be explained by the fact that the further one gets from the tonsil capsule into the tonsil the smaller the vessel diameter becomes.
In light of our results it is possible to hypothesize that inflammation may play a role in the higher bleeding rate post TA this may be caused by release of vasodilators.
Parents of the children in the PITA groups also reported less pain, as compared to the TA patients.
This was true in all aspects that we checked with the questionnaires (pain, medications, swallowing difficulty). These results are in line with previous reports [3–12]. There was no difference between patients in the LPITA group and DPITA group in regards to pain. Possible explanations for the differences in pain are: the capsule left intact protects the muscle from inflammation. Alternatively, during TA the muscle may be injured causing a greater degree of inflammatory reaction. Additionally, following TA, the whole tonsil is removed so a larger bare surface is exposed, causing more pain.
During the first postoperative week the questionnaires showed worse snoring in the TA group; however, the difference was not statistically significant. We think this trend is due to postoperative edema, which is more serious after tonsillectomy with electrocautery dissection most likely due to thermal effect on surrounding tissues. We don’t have data regarding snoring for the long term, but other studies did not find a significant difference in snoring after partial tonsillectomy versus total tonsillectomy [3, 10, 12, 21]. Polysomnography before and at 3–6 months after operation, was performed in 28 patients. No significant differences were noticed between the groups with regards to postoperative AHI. We conclude that in the short term there is no difference in the resolution of OSDB between PITA and TA.
Levels of inflammatory mediators (WBC, NEU, CRP) increased, postoperatively, in all three groups with the highest values in the TA group. This may lead one to conclude that in a more conservative operation there is less inflammation than occurs in a wider operation. Studies from gynecology and general surgery show similar patterns with greater increase in levels of inflammatory mediators after open procedures versus laparoscopic surgery [13–15]. However IL-6 increased more in the PITA group and TNF was totally inconclusive.
In a previous study by our department levels of inflammatory mediators were compared in patients undergoing TA with and without the use of fibrin glue applied to the tonsillar fossa [25]. In that study levels of all inflammatory mediators were less elevated when fibrin glue was applied to the tonsillar bed; however, the reduction of pain in these circumstances showed conflicting results. Gross et al. [26] and Stevens et al. [27] found that fibrin glue reduces pain whereas Segal et al. [28] and Stoeckli et al. [29] did not find any difference. Stiller et al. [25] found that inflammation was not correlated with pain or bleeding so it is difficult, to interpret the exact significance of the markers. The current study regarding PITA vs TA again shows that it is difficult to interpret the results of cytokine levels in association with pain after surgery.
Limitations of this study
Firstly, we were unable to perform postoperative PSG for all children, because the caregivers did not feel that repeated examination was necessary after the child was “cured”. This raises the possibility of selection bias which might have caused the spurious differences between the study groups. This difference might have been narrowed or even eliminated had we been able to obtain PSG from all patients.
Another limitation is that that adenoidectomy which was performed in all patients may have influenced the results. Tonsil surgery for OSDB is almost always accompanied by adenoidectomy making it extremely difficult to recruit a large enough study group of patients undergoing only tonsil surgery for their OSBD. In addition adenoidectomy was performed in the same method in all patients.
The groups were different in their baseline CRP values in spite of the randomization, possibly due to the relatively small groups. This made the comparison adjusting to the baseline CRP the only valid analysis to be considered at the study conclusion, as opposed to the primary univariate analysis.
Lastly, levels of the inflammatory mediators were obtained within 24 h of surgery and we did not obtain repeated measurements of these levels. Such levels if assessed 3–7 days after surgery might have been substantially different. The difference between the groups regarding pain is seen from the first postoperative day till at least the 7th day, but whether this is true could be studied in the future.
One more limitation is lack of data regarding additional disease such as allergy or asthma. These were not screened during the study and might have influenced inflammatory markers before and after surgery.
Conclusion
In the current study we showed clear benefits of PITA procedure compared to TA (using monopolar diathermy) in terms of morbidity (pain and bleeding) as shown in previous studies. However, the inflammatory response during the first 24 h after surgery did not differ significantly. Future studies are needed to assess safety and efficacy at the long-term follow-up.
References
Stucken Emily Z, Grunstein Eli, Jr Joseph Haddad et al (2013) Factors contributing to cost in partial versus total tonsillectomy. Laryngoscope 123:2868–2872
Younis RT, Lasar RH (2002) History and current practice of tonsillectomy. Laryngoscope 112:3–5
Koltai PJ, Solares CA, Koempel JA, Hirose K, Aberson TI, Cracovitz PR, Chan J, Xu M, Mascha EJ (2000) Intracapsullar tonsillar reduction (partial tonsillectomy): reviving a historical procedure for obstructive sleep disordered breathing in children. Otolaryngol Head Neck Surg 129(5):532–538
Densert O, Desai H, Eliasson A, Frederiksen L, Andersson D, Olaison J, Widmark C (2001) Tonsillectomy in children with tonsillar hypertrophy. Acta Otolarynol 20(7):854–858
Hultcrantz E, Linder A, Markstom A (1999) Tonsillectomy or tonsillotomy? A randomized study comparing postoperative pain and long term effect. Int J Pediatr Otolaryngol 51(1):171–176
Hultcharntz E, Ericsson E (2004) Pediatric tonsillotomy with radiofrequency technique: less morbidity and pain. Laryngoscope 114(5):871–877
Hultcrantz E, Linder A, Marksrom A (2005) Long-term effects of intracapsular partial tonsillectomy (tonsillotomy) compared with full tonsillectomy. Int J Pediatr Otolaryngol 69(4):463–469
Koempel JA, Solares CA, Koltai PJ (2006) The evolution of tonsil surgery and rethinking the surgical approach to obstructive sleep-disordered breathing in children. J Laryngol Otol 120(12):993–1000
Lister MT, Cunningham MJ, Benjiamin B, Williams M, Tirrell A et al (2006) Microdebrider tonsillotomy vs electrosurgical tonsillectomy: a randomized, double-blind, paired control study of postoperative pain. Arch Otolaryngol Head Neck Surg 132(6):599–604
Bitar MA, Rameh C (2008) Microdebrider assisted partial tonsillectomy: short- and long-term outcomes. Eur Arch Otorhinolaryngol 256(4):459–463
Ericsson E, Hultcrantz E (2007) Tonsil surgery in youth: good results with a less invasive method. Laryngoscope 117(4):654–661
Ericsson E, Ledin T, Hultcrantz E (2007) Long-term improvement of quality of life as a result of tonsllotomy(with radiofrequency technique)and tonsillectomy in youth. Laryngoscope 117(7):1272–1279
Torres A, Torres K, Paszkowski T, Staskievicz GJ, Maciejewski R (2007) Cytokine response in the postoperative period after surgical treatment of benign adnexal masses: comparison between laparoscopy and laparotomy. Surg Endosc 21:1841–1848
Igarashi T, Takahashi H, Tanaka M, Murakami S (1996) Serum interleukin-6 levels after urologic operation. Int J Urol 3:340–342
Buunen M, Gholghesaei M, Veldkamp R, Meijer DW, Bonjer HJ, Bouvy ND (2004) Stress response to laparoscopic surgery: a review. Surg Endosc 18:1022–1028
Brodsky L (1989) Modern assessment of tonsils and adenoids. Pediatr Clin North Am 36(6):1551–1569
Sidney Siegel (1956) Nonparametric statistics for the behavioural sciences, International Student Edition. McGraw-Hill Inc, New York, Toronto, London, p 126
Sarny S, Ossimitz G, Habermann W, Stammberger H (2011) Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope 121(12):2553–2560
Derkay CS, Darrow DH, Welch C, Sinacori JT (2006) Posttonsillectomy morbidity and quality of life in pediatric patients with obstructive tonsils and adenoid: microdebrider vs electrocautery. Otolaryngol Head Neck Surg 134:114–120
Doshi HK, Rosow DE, Ward RF, April MM (2011) Age related tonsillar regrowth in children undergoing powered intracapsular tonsillectomy. Int J Pediatr Otolaryngol 75:1395–1398
Vlastos IM, Parpounas K, Economides J, Helmis G, Koudoumnakis E, Houlakis M (2008) Tonsillectomy versus tonsillotomy performed with scissors in children with tonsillar hypertrophy. Int J Pediatr Otolaryngol 72:857–863
Internet reference: National Prospective Tonsillectomy Audit FINAL REPORT of an audit carried out in England and Northern Ireland between July 2003 and September 2004. Retrieved May 2005. https://www.rcseng.ac.uk/surgeons/research/surgical-research/docs/National%20Prospective%20Tonsillectomy%20Audit%20Final%20Report%202005.pdf. Accessed 11 May 2016
Gan K, Tomlinson C, El-Hakim H (2009) Postoperative bleeding is less after partial intracapsular tonsillectomy than bipolar total procedure. Int J Pediatr Otolaryngol 73:667–670
Sarny S, Ossimitz G, Habermann W, Stammberger H (2011) Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope 121(12):2553–2560
Stiller-Timor L, Goldbart A, Leiberman A et al (2012) Circulating cytocines in patients undergoing tonsillectomy with fibrin glue. Int J Pediatr Otolaryngol 76(3):419–422
Gross CW, Gallagher R, Schlosser RJ et al (2001) Autologous fibrin sealant reduces pain after tonsillectomy. Laryngoscope 11(2):259–263, 33
Stevens MH, Stevens DC (2005) Pain reduction by fibrin sealant in older children and adult tonsillectomy. Laryngoscope 115(6):1093–1096
Segal N, Puterman M, Rotem E et al (2008) A prospective randomized double-blind trial of fibrin glue for reducing pain and bleeding after tonsillectomy. Int J Pediatr Otorhinolaryngol 72(4):469–473
Stoeckli SJ, Moe KS, Huber A, Schmid S (1999) A prospective randomized double-blind trial of fibrin glue for pain and bleeding after tonsillectomy. Laryngoscope 109(4):652–655
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was partially supported by the Israel Science Foundation (ISF 1344/15) recipient Aviv Goldbart.
Conflict of interest
Additional authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Soroka University Medical Center (SUMC) IRB committee. W (#NCT01319058CINICALTRIAL.GOV).
Informed consent
Informed consent was obtained from all caregivers of individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kordeluk, S., Goldbart, A., Novack, L. et al. Randomized study comparing inflammatory response after tonsillectomy versus tonsillotomy. Eur Arch Otorhinolaryngol 273, 3993–4001 (2016). https://doi.org/10.1007/s00405-016-4083-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4083-5