Abstract
The objective of this study was to examine the clinical and pathological features of squamous cell carcinoma of the Tongue and Buccal Mucosa and understand their differences. This is a retrospective analysis of prospectively collected data of 735 patients with squamous cell carcinoma of the tongue and 665 cases of carcinoma of the buccal mucosa treated by surgery at our hospital. Statistical analysis was done to examine clinical and pathological differences between carcinoma of the tongue and the buccal mucosa with regards to age, gender, clinical T stage/N stage, pathological T stage/N stage, overall stage, grade, thickness, perinodal extension (PNE), lymphovascular emboli (LVE) and perineural invasion (PNI). Statistically significant differences were found for factors like age (p < 0.001), gender (p < 0.001), clinical T staging (p < 0.001) and pathological stage (p < 0.001), grade of tumor (p < 0.001) and perineural invasion (p < 0.001) between carcinoma of the tongue and the buccal mucosa. Forty-eight percent patients in either subsite had pathologically proven node negative necks (pN0, p = 0.88). Multivariate analysis for occult nodal metastases revealed that predictive factors were different for the two subsites. There are significant differences between cancers of the tongue and buccal mucosa for various clinical and pathological factors. This may be a reflection of the underlying differences in their causation and pathophysiology. Squamous cell carcinoma in these two subsites should therefore be regarded as clinico-pathologically distinct entities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Squamous cell carcinoma of the oral cavity is the sixth most common cancer in the world [1]. It is one of the most common forms of cancer in the Indian subcontinent and in other parts of Asia [2]. The tongue is the commonest site for oral cavity squamous cell cancers (OSCC) in the western literature whereas in Asian countries buccal mucosal cancers are more prevalent [3, 4]. This is generally attributed to the prevalent habits of using smokeless tobacco and betel quid chewing. Most scientific data on tongue cancers report them to be more aggressive tumors with higher propensity for lymph nodal metastases [5]. However, no large clinical study to date has compared clinical and pathological differences between tongue and buccal mucosal cancers. The treatment recommendations are generally uniform, irrespective of the sub site involved. Protocols for postoperative adjuvant therapy and follow-up also do not vary by tumor sub site. We, therefore, decided to study the squamous cell carcinomas in these two subsites of the oral cavity to ascertain any differences in the clinical presentation and pathological features.
Patients and methods
The present study is a retrospective analysis of prospectively collected data of patients with biopsy proven squamous cell carcinoma of the buccal mucosa or the anterior tongue. Inclusion criteria were as follows: (a) biopsy proven squamous cell carcinoma, (b) oral cavity sub site: the tongue or buccal mucosa. Gingivobuccal sulcus cancers were included into buccal mucosa cancers, (c) surgical treatment included excision of the primary tumor and appropriate neck dissection.
All patients received appropriate adjuvant therapy at Tata Memorial Hospital between 2006 and 2010. There were 735 patients with tongue cancer and 665 patients with buccal cancer eligible for inclusion in the study. All patients were evaluated clinically and staged after appropriate clinical and radiological investigations. Staging was documented using the 2002 American Joint committee on Cancer, sixth edition staging criteria (While AJCC and UICC staging manuals are same, only the UICC staging manual is licensed for use outside the USA. Hence, it is appropriate to use the term UICC staging manual). Patients’ demographic and clinical details were prospectively collected. Histopathology details were collected from the hospitals’ electronic medical records.
Statistical analysis
SPSS, Version 16 was used for statistical analysis. For analysis, the clinical variables such as T status and stage of the disease were divided in two groups: early and advanced. T1 and T2 were combined together as early tumors and T3 and T4 combined together as advanced lesions. Similarly, stages I and II were considered together as early disease and stages III and IV grouped together as advanced disease. ‘Chi square test’ was used as a test of significance for comparison between the two subsites. Significant predictive variables of disease outcome on univariate analysis were incorporated into multivariate analysis. Multivariate logistic regression analysis of clinico-pathologic factors was performed to know their predictive value for occult nodal metastases.
Results
The mean age at presentation was found to be significantly lower for patients with oral tongue cancers compared to those with buccal mucosal cancers. The overall mean age at presentation was 49.5 years. Mean age at presentation for oral tongue cancer patients was 48 years (range 20–104) while that for patients with buccal mucosal cancers was 51 years (range 21–85). Tongue cancers were more prevalent in the younger population (<35 years) as compared to buccal cancers (p < 0.001). Squamous cell carcinoma of oral cavity was found to be more prevalent in men compared to women. Overall male: female ratio for was 2.83:1. The male preponderance was slightly higher for buccal cancers (M:F ratio 3.26:1) than for tongue cancer (M:F ratio 2.51:1) (p = 0.1129) (Table 1).
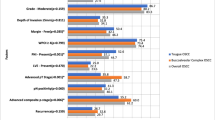
Nearly 60 % of the tongue cancer patients presented with early stage tumors (T1 + T2) as compared to buccal cancers (18 %). With regard to the overall stage, majority of the patients with tongue cancer had early stage cancers on final histopathology (37 %) as compared to patients with buccal mucosa cancers (26 %, p < 0.001). Significantly larger proportions of tongue cancers were poorly differentiated when compared to buccal cancers (p < 0.001).
Forty-eight percent patients in either sub site had pathologically proven node negative necks (pN0, p = 0.88). We did not find any statistically significant difference between the two subsites for lymph node metastases even in early (T1 + T2) tumors (p = 0.24). On univariate analysis thickness, clinical and pathological staging, clinical nodal status, perineural invasion and grade of differentiation were significant predictors of nodal metastases for tongue cancers, whereas those for buccal cancers were thickness, clinical T stage, clinical nodal status, perineural invasion and grade of differentiation (Table 2). On multivariate analysis (Table 3) for tongue cancers clinical nodal status, tumor thickness and grade of tumor were significant predictors of nodal metastases, whereas, those for buccal cancers were age, clinical nodal status, perineural invasion and differentiation of the tumor. Multivariate analysis for occult nodal metastases revealed that thickness, clinical and pathological T stage, LVE and PNI were significant predictors for tongue cancers. For buccal cancers only grade of differentiation was a significant predictor of occult nodal metastases on multivariate analysis. The incidence of ECS was not found to be significantly different between tongue (34 %) and buccal mucosa (38 %). There was no statistically significant difference in the mean tumor thickness between tongue cancers (12.95 ± 7.4 mm; mean ± 2SD) and that for buccal mucosa cancers (13 ± 9 mm; mean ± 2SD). There was no difference in the two subsites with regards to lymphovascular invasion (LVI: 2 and 2.6 %, respectively), whereas perineural invasion (PNI) was significantly higher in tongue cancers (27 vs 16.5 %, p < 0.001).
Discussion
Oral cavity squamous cell carcinoma is one of the leading causes of cancer related death in developing countries, particularly India [6]. The high risk of oral cavity cancers in Indian population is related to the popularity of consumption of tobacco quid (combination of tobacco, betel leaf, areca nut and flavors. Very few studies in literature have directly compared differences between oral cavity squamous cell carcinomas of the tongue and the buccal mucosa. There is data, however, that suggests there is significant difference between clinical behavior of squamous cell carcinoma among the various subsites of oral cavity [7]. Tongue cancers, especially, are known to have an aggressive course and poor prognosis [5]. Yao et al. reported their study of 55 patients who received intensity modulated radiation therapy for oral cavity cancer [8]. In that series, oral tongue cancer was associated with significantly worse 2-year locoregional recurrence free survival compared with floor of mouth cancer (68.8 vs 100 %; p = 0.03), and there was a trend towards a lower rate of locoregional control compared with all oral cavity subsites (p = 0.09). In contrast, another study from the University of Oregon with 233 oral cavity tumors, reported no difference in overall survival (p = 0.8) or disease-free survival (p = 0.7) when comparing cancers of the oral tongue with cancers of other oral cavity subsites [9]. However, both studies were small series and included patients with all stages of disease, making direct survival comparisons between subsites difficult. Another study of patients with stage I and II oral cavity tumors on the SEER database showed 5-year overall and cause-specific survival rates of 60.9 and 83.5 % for oral tongue and 64.7 and 94.1 % for other oral cavity subsites (p < 0.0001). This study also showed that stage I and II oral tongue cancers have a significantly worse cause-specific survival than stage III (HR, 1.70; p < 0.001) and 4 (HR, 1.56; p < 0.001) oropharyngeal cancers [10]. A study from Taiwan reported that although there were no significant differences in overall survival between tongue and buccal mucosal cancers, their failure patterns were significantly different [7]. Molecular markers in tongue and buccal mucosal cancers have also been studied with reports of differences in molecular markers between the tongue and buccal cancers [11, 12]. In the present study we found significant differences in clinical and pathological features between these two subsites.
Age at presentation
United States (SEER) data reported that the large majority of OSCC patients are over 45 years of age, with a median age of first OCSCC diagnosis at 62 years [13]. About 6 % of oral cancers occur in young people under the age of 45 years [14]. In contrast, in our data the mean age of presentation is 50 years which is much lower than the western data. Use of smokeless tobacco from young age could be a reason for this difference. Interestingly, in our study, the mean age at presentation for tongue cancers was significantly lower (48 ± 12.3 years, mean ± 2 SD) when compared to buccal mucosa cancers (51 ± 11 years, mean ± 2 SD). In the younger population (≤35 years), tongue cancers were more prevalent as compared to buccal mucosa (p < 0.001). Similar observations were made in another study focusing on OSCC in patients less than 35 years [15].
Gender
There is an overall male predominance in all intraoral subsites seen in most studies. But some have reported a female predominance in younger age group [16]. In our study we found male preponderance for oral cavity cancer; overall as well as for both the subsites. Buccal cancers had a higher M:F (male:female) ratio than tongue cancers. Overall M: F ratio for was 2.83. The male preponderance was slightly higher for buccal cancers (M:F = 3.26:1) than for tongue cancer (M:F = 2.51:1).
Clinical and pathological T staging
The tumour size has an impact on the choice of primary definitive treatment, adjuvant therapy as well as prognosis [17]. Increased tumour size has been linked to lymph node metastasis high recurrence rate [18] and overall poorer outcomes [19]. We grouped tumors into early tumors (T1 + T2) and advanced tumors (T3 + T4). While majority (60 %) of the tongue cancer patients presented with early stage tumors (clinical T1 + T2), only 18 % buccal cancers presented early (p < 0.001). Similar findings were noted on pathological T staging. Oral Tongue lesions produce early symptoms such as pain, difficulty in speech and swallowing and are also easily visible on self-examination. This could be the reason for early presentation of tongue cancers.
Lymph node metastases
Occult lymph node metastasis in early stage (T1/T2) oral cavity tumors has been reported to be between 27 and 40 % [20]. Lymph node metastasis negatively affects disease-specific survival in HNSCC [21]. Prognosis further worsens with the presence multiple nodal metastases and extracapsular spread [22, 23]. Since there are reports of higher nodal metastasis in tongue cancers [5], we analyzed our own data to compare its incidence in both the subsites. Considering all the T stages together, the overall incidence of nodal metastasis was 48 % for both tongue and buccal cancers. Even in early stage disease (T1/T2), there was no significant difference (p = 0.2) between these subsites. This suggests that the propensity for nodal metastasis is equal for cancers arising in these subsites (Table 4).
Factors predicting lymph node metastases in clinically N0 patients
Various factors reported in literature to predict nodal metastases include primary site, thickness, double DNA aneuploidy, poor differentiation, perineural invasion and infiltrating invasive front [24, 25].
Univariate analysis of clinico-pathological factors and lymph node metastases
On univariate analysis, thickness, clinical and pathological staging, clinical nodal status, perineural invasion and grade of differentiation were significant predictors of nodal metastases for tongue cancers, whereas those for buccal cancers were thickness, clinical T stage, clinical nodal status, perineural invasion and grade of differentiation (Table 2).
Multivariate analysis of clinico-pathological factors and lymph node metastases
On multivariate analysis for tongue cancers, clinical nodal status, tumor thickness and grade of tumor were significant predictors of nodal metastases whereas those for buccal cancers were age, clinical nodal status, perineural invasion and differentiation of the tumor (Table 3).
Multivariate analysis of clinico-pathological factors associated with occult lymph node metastases
Multivariate analysis for occult lymph node metastases revealed that thickness, clinical and pathological T stage, LVE and PNI were significant predictors for tongue cancers. For buccal cancers only grade of differentiation was a significant predictor of occult nodal metastases (Table 5). Although the incidence of occult nodal metastases is similar, the factors predicting them are different for the two subsites. This may be due to difference in biological nature of the subsites. The management of the clinically node negative neck in early oral cancers has been a subject of debate. There is lack of strong evidence to suggest the superiority of elective neck dissection (END) over therapeutic neck dissection. The factors predicting occult nodal metastases identified in this study can help in deciding management of neck for the cancers in the two subsites. Tongue cancers with thicker tumors and poor grade may benefit from elective neck dissection. Similarly buccal mucosal cancers with poor grade may benefit from elective neck dissection.poorly differentiated when
Perinodal extension (PNE)
The incidence of perinodal spread varies in studies between 21 and 85 % [26]. Meta-analyses of perinodal extension in HNSCC strongly suggests that perinodal spread significantly reduces (doubled risk) the five-year-survival [27]. The identification or the exclusion of perinodal spread in HNSCC directly influences treatment. In the case of histopathologically identified metastases with extracapsular tumour growth, adjuvant therapy in the form of concurrent chemoradiation is recommended [28]. Even though it is generally believed that tongue cancers have a higher propensity for lymph nodal metastases as well as perinodal spread [5], we did not observe a significant difference in the presence of PNE between these two subsites.
Tumor thickness
The mean tumor thickness for tongue cancers was 12.95 ± 7.4 mm (mean ± 2SD) and 13 ± 9 mm (mean ± 2SD) for buccal mucosa cancers. The observed difference was not statistically significant. The association of tumour thickness with lymph node metastasis is believed to reflect the aggressiveness of tumour growth [29]. Various studies have shown a strong relationship exists between tumour thickness and cervical metastasis [24, 25]. On univariate analysis, tumor thickness was found to be a significant predictor of lymph node metastases for both tongue as well as buccal mucosal cancers, however, on multivariate analysis tumor thickness was found to be a significant predictor of lymph nodal metastases only for tongue cancers. Similar findings were noted on multivariate analysis for factors associated with occult nodal metastases.
Grade of differentiation
The WHO grading system recommends 3 categories: well differentiated, moderately differentiated and poorly differentiated [30]. It is widely accepted that prognosis is better in early cancers, particularly those that are well differentiated [31]. Conflicting evidence exists with regards to grade of differentiation as a prognostic factor for locoregional failure, recurrence and survival. One study reports it to be a significant predictor of locoregional failure and recurrence [32] while other studies have reported the grading system to be a poor indicator of outcome and response to treatment [31, 33, 34].
Majority of our study population had moderately differentiated cancers (72.78 %). Poorly differentiated cancers were the next most common (19.5 %). Well differentiated cancers were very few (7.71 %). Subsite distribution showed a similar pattern when individual differentiation was considered. A significantly larger proportion of tongue cancers were poorly differentiated when compared to buccal cancers (p < 0.001) (Table 6).
Lymphovascular emboli and perineural invasion
Lymphovascular emboli (LVE) and Perineural (PNI) invasion show a significant association with tumour size, histological grading, nodal involvement, status of the surgical margins, overall prognosis and survival [17]. Lymphovascular emboli increase the likelihood of regional and distant metastasis [18]. In our study 2 % of tongue cancers had presence of Lymphovascular emboli whereas that in buccal cancers was 2.6 %. This difference was not statistically significant (p = 0.3). LVE was not a significant predictor of lymph nodal metastases in either of the subsites in our population. The prognostic value of perineural invasion is uncertain. Some studies have positively linked it to regional recurrence and distant metastasis [35, 36] while others detected no such association [37]. In a recent study multivariate analysis) of perineural invasion of small and large nerves, only invasion of large nerves was associated with local recurrence [38]. In our study 27 % of tongue cancers had perineural invasion compared to the 16.5 % in buccal cancers (p = <0.001). PNI is a significant predictor for lymph nodal metastasis in buccal cancers.
Overall survival and patterns of failure
Though single series have reported inferior outcomes in patients with carcinoma of tongue and floor of mouth [39], others have failed to demonstrate difference between proposed subsites [40]. A study from Taiwan, concluded that although the overall survival for squamous carcinoma of the tongue and buccal mucosa was the same, patterns of failure were significantly different. Tongue cancers had higher incidence of regional failure whereas buccal cancers had higher incidence of distant metastases [7]. We have not included survival analysis in this study. However, a large retrospective study from our institute on patients treated with surgery followed by adjuvant radiotherapy for oral cavity squamous cell carcinoma showed that patients with carcinoma of the Gingivobuccal sulcus, palate and lip (considered together as Group I) had significantly better locoregional control (68 vs 57 %, p = 0.005) and disease-free survival (64 % vs 52 %, p = 0.001) when compared to patients with squamous carcinoma of the tongue and floor of mouth (Group II). They also noted that patients with tongue and floor of mouth cancers had significantly higher nodal failures (11.5 vs 6.8 %, p = 0.003) [41].
Conclusion
Squamous cell carcinoma of the tongue and buccal mucosa have equal propensity for lymph nodal metastases as well as perinodal extension. However, the factors predicting nodal metastasis in these two subsites are different. Thickness, grade of differentiation, clinical and pathological T stage, LVE and PNI are significant predictors of occult nodal metastases in tongue carcinomas whereas for buccal cancers only grade of differentiation is significant. These factors can help in deciding the surgical management of a clinically N0 neck. Squamous carcinoma of the tongue and buccal mucosa have significant differences with regards to clinical and pathological factors such as mean age at presentation, clinical and pathological stage, grade of differentiation and perineural invasion. Patterns of failure have been shown to be significantly different for the individual subsite in various studies. Squamous cell carcinoma of the tongue and the buccal mucosa should therefore be considered as clinico-pathologically distinct entities.
References
Warnakulasuriya S (2009) Global epidemiology of oral and oropharyngeal cancer. Oral Oncol 45(4–5):309–316
Babu KG (2001) Oral cancers in India. Semin Oncol 28:169–173
Paterson IC, Eveson JW, Prime SS (1996) Molecular changes in oral cancer may reflect aetiology and ethnic origin. Eur J Cancer B Oral Oncol 32B:150–153
Landis SH, Murray T, Bolden S, Wingo PA (1998) Cancer statistics, 1998. CA Cancer J Clin 48:6–29
Moore SR, Johnson NW, Pierce AM, Wilson DF (2000) The epidemiology of tongue cancer: a review of global incidence. Oral Dis 6:75–84
Yeole BB, Sankaranarayanan R, Sunny MSL, Swaminathan R, Parkin DM (2000) Survival from head and neck cancer in Mumbai (Bombay), India. Cancer 89:437–444
Liao CT, Huang SF, Chen IH, Kang CJ, Lin CY, Fan KH, Wang HM et al (2010) Tongue and buccal mucosa carcinoma: is there a difference in outcome? Ann Surg Oncol 17(11):2984–2991
Yao M, Chang K, Funk GF et al (2007) The failure patterns of oral cavity squamous cell carcinoma after intensity-modulated radiotherapy—the University of Iowa experience. Int J Radiat Oncol Biol Phys 67:1332–1341
Bell RB, Kademani D, Homer L, Dierks EJ, Potter BE (2007) Tongue cancer: is there a difference in survival compared with other subsites in the oral cavity? J Oral Maxillofac Surg 65:229–236
Kyle R, Ari B, David R (2008) Changhu Chen. Poor prognosis in patients with stage I and II oral tongue squamous cell carcinoma cancer 112:345–351
Sathyan KM, Sailasree R, Jayasurya R et al (2006) Carcinoma of the tongue and buccal mucosa represent different biological subentities of the oral carcinoma. J Cancer Res Clin Oncol 132:601–609
Schwartz JL, Gu X, Kittles RA, Baptiste A, Shklar G (2000) Experimental oral carcinoma of the tongue and buccal mucosa: possible biological markers linked to cancer at 2 anatomic sites. Oral Oncol 36:225–235
Surveillance epidemiology and end results (SEER): SEER Cancer statistics review 1975–2013. http://seer.cancer.gov/statfacts/html/oralcav.html. Accessed 18 Apr 2016
Llewellyn CD, Johnson NW, Warnakulasuriya KAAS (2001) Risk factors for squamous cell carcinoma of the oral cavity in young people—a comprehensive literature review. Oral Oncol 37:401–418
Iype EM, Pandey M, Mathew A, Thomas G, Sebastian P, Nair MK (2001) Oral cancer among patients under the age of 35 years. J Postgrad Med [serial online] 47:171 (cited 18 Mar 2012)
Kuriakose M, Sankaranarayanan M, Nair MK, Cherian T, Sugar AW, Scully C et al (1992) Comparison of oral squamous cell carcinoma in younger and older patients in India. Eur J Cancer B Oral Oncol 28:113–120
Scully C, Bagan J (2009) Oral squamous cell carcinoma overview. Oral Oncol 45(4–5):301–308
Woolgar JA (2006) Histopathological prognosticators in oral and oropharyngeal squamous cell carcinoma. Oral Oncol 42(3):229–239
Platz H, Fries R, Hudec M, Min Tjoa A, Wagner RR (1983) Rhe prognostic relevance of various factors at the time of the first admission of the patient. Retrospective DOSAK study on carcinoma of the oral cavity. J Maxillofac Surg 11(1):3–12
Teichgraeber JF, Clairmont AA (1984) The incidence of occult metastases for cancer of the oral tongue and floor of the mouth: treatment rationale. Head Neck Surg 7:15–21
Greenberg JS, El Naggar AK, Mo V, Roberts D, Myers JN (2003) Disparity in pathologic and clinical lymph node staging in oral tongue carcinoma. Implication for therapeutic decision making. Cancer 98:508–515
Greenberg JS, Fowler R, Gomez J, Mo V, Roberts D, El Naggar AK, Myers JN (2003) Extent of extracapsular spread: a critical prognosticator in oral tongue cancer. Cancer 97:1464–1470
Layland MK, Sessions DG, Lenox J (2005) The influence of lymph node metastasis in the treatment of squamous cell carcinoma of the oral cavity, oropharynx, larynx, and hypopharynx: N0 versus N+. Laryngoscope 115:629–639
Sparano A, Weinstein G, Chalian A, Yodul M, Weber R (2004) Multivariate predictors of occult neck metastasis in early oral tongue cancer. Otolaryngol Head Neck Surg 131:472–476
Lim SC, Zhang S, Ishii G, Endoh Y, Kodama K, Miyamoto S, Hayashi R, Ebihara S, Cho JS, Ochiai A (2004) Predictive markers for late cervical metastasis in stage I and II invasive squamous cell carcinoma of the oraltongue. Clin Cancer Res 10:166–172
Carter RL, Barr LC, O’Brien CJ et al (1985) Transcapsular spread of metastatic squamous cell carcinoma from cervical lymph nodes. Am J Surg 150:495–499
Dunne AA, Muller HH, Eisele DW, Keßel K, Moll R, Werner JA (2006) Meta-analysis of the prognostic significance of perinodal spread in head and neck squamous cell carcinomas (HNSCC) patients. Eur J Cancer 42:1863–1868
Boysen M, Lovdal O, Natvig K et al (1992) Combined radiotherapy and surgery in the treatment of neck node metastases from squamous cell carcinoma of the head and neck. Acta Oncol 31:455–460
Moore C, Kuhns JG, Greenberg RA (1986) Thickness as prognostic aid in upper aerodigestive tract cancer. Arch Surg 121(12):1410–1414
Pindborg JJ, Reichart PA, Smith CJ, van der Waal I (1997) World Health Organisation histological typing of cancer and precancer of the oral mucosa, 2nd edn. Springer, New York
Scully C, Bagan JV (2009) Recent advances in oral oncology 2008; squamous cell carcinoma imaging, treatment, prognostication and treatment outcomes. Oral Oncol 45(6):e25–e30
Larsen SR, Johansen J, Sørensen JA, Krogdahl A (2009) The prognostic significance of histological features in oral squamous cell carcinoma. J Oral Pathol Med 38(8):657–662
Woolgar JA, Rogers S, West CR, Errington RD, Brown JS, Vaughan ED (1999) Survival and patterns of recurrence in 200 oral cancer patients treated by radical surgery and neck dissection. Oral Oncol 35(3):257–265
Po Wing Yuen A, Lam KY, Lam LK, Ho CM, Wong A, Chow TL, Yuen WF, Wei WI (2002) Prognostic factors of clinically stage I and II oral tongue carcinoma: a comparative study of stage, thickness, shape, growth pattern, invasive front malignancy grading, Martinez-Gimeno score, and pathologic features. Head Neck 24(6):513–520
Fagan JJ, Collins B, Barnes L, D’Amico F, Myers EN, Johnson JT (1998) Perineural invasion in squamous cell carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg 124(6):637–640
Rahima B, Shingaki S, Nagata M, Saito C (2004) Prognostic significance of perineural invasion in oral and oropharyngeal carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97(4):423–431
Weijers M, Snow GB, Bezemer DP, van dr Wal JE, van der Waal I (2004) The status of the deep surgical margins in tongue and floor of mouth squamous cell carcinoma and risk of local recurrence; an analysis of 68 patients. Int J Oral Maxillofac Surg 33(2):146–149
Brandwein-Gensler M, Teixeira MS, Lewis CM, Lee B, Rolnitzky L, Hille JJ et al (2005) Oral squamous cell carcinoma: histologic risk assessment, but not margin status, is strongly predictive of local disease-free and overall survival. Am J Surg Pathol 29(2):167–178
Yao M, Chang K, Funk GF et al (2007) The failure patterns of oral cavity squamous cell carcinoma after intensity-modulated radiotherapy—the University of Iowa experience. Int J Radiat Oncol Biol Phys 67:1332–1341
Bell RB, Kademani D, Homer L, Dierks EJ, Potter BE (2007) Tongue cancer: is there a difference in survival compared with other subsites in the oral cavity? J Oral Maxillofac Surg 65:229–236
Murthy V, Agarwal JP, Laskar SG, Gupta T, Budrukkar A, Pai P et al (2010) Analysis of prognostic factors in 1180 patients with oral cavity primary cancer treated with definitive or adjuvant radiotherapy. J Cancer Res Ther 6:282–289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No external funding was received for the present study. The Authors have no conflict of interest to disclose.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Nair, S., Singh, B., Pawar, P.V. et al. Squamous cell carcinoma of tongue and buccal mucosa: clinico-pathologically different entities. Eur Arch Otorhinolaryngol 273, 3921–3928 (2016). https://doi.org/10.1007/s00405-016-4051-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4051-0