Abstract
This retrospective review aims to evaluate the postoperative morbidity and mortality of 30 patients with Down syndrome who underwent adenotonsillectomy between June 2012 and December 2015 in a tertiary referral center. Mean age was 7.8 with a range of 3–12. There were 20 (66.6 %) male and ten (33.3 %) female patients. Mean follow-up was 23 months with a range of 7–43 months. 23 (76.6 %) of 30 patients had been operated due to obstructive tonsillar and adenoid hypertrophy, whereas seven (23.3 %) of them operated for chronic recurrent infections. All of the patients had undergone adenotonsillectomy operation; one patient had also bilateral tympanostomy tube insertion. Hospital stay was noted 1.3 days in average with a range of 1–3 days. Anesthetic complications of persistent bradycardia and postextubation respiratory difficulty occurred in two (6.6) patients. Patient who had intraoperative bradycardia necessitated intensive care unit stay and pacemaker implantation during follow-up. 3 (10 %) patients had late onset hemorrhage between days 7 and 10 and required intraoperative bleeding control. We did not experience any other morbidity and mortality except the abovementioned ones. In conclusion, adenotonsillectomy in patients with Down syndrome is a worthwhile operation with certain risks and these operations should better be performed by the tertiary referral centers which have the capacity to deal with the complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Down syndrome (DS) is known as the most common chromosomal abnormality and occurs about 1 in 750 live births [1]. Obstructive sleep apnea (OSA) is seen in high proportion of DS patients, with a tendency for pulmonary artery hypertension and congestive heart failure [2–5]. OSA in DS patients was caused by multiple predisposing factors, including their relatively small mid-face and cranium, narrow nasopharynx, relatively large tongue for their hypoplastic mandibula, preponderance towards obesity, increased secretions, muscular hypotonia, lymphoid hyperplasia [5]. In addition they have relatively small larynx and in some cases severe laryngeal and tracheal abnormalities are seen [3, 5, 6].
Some of the DS patients require adenotonsillectomy (AT) as a remedy for obstruction in upper airway or recurrent infections [2, 7]. Although it is not a complete cure for OSA in DS patients, AT is accepted as the first-step surgical treatment for this situation [8]. We aimed to evaluate the operative complications of AT in this peculiar group of patients and discuss our experience in the light of the literature.
Materials and methods
We reviewed the medical charts and collected data of 30 DS patients who had undergone AT at a tertiary referral center, between June 2012 and December 2015. Medical records were reviewed to note age, sex, diagnosis, past medical history, physical examination findings, type of operation, follow-up duration, duration of hospital stay, postoperative intensive care unit (PICU) admission and length of stay in PICU, anesthetic complications, received anesthetic drugs, respiratory complications, surgery-related complications, required medical and surgical interventions, time to resumption of proper oral intake after the surgery, causes and duration of readmission to the hospital. Descriptive statistics only were used.
Results
Demographics of patients are summarized in Table 1. 30 patients were identified over a 3-year period, with 20 (66.6 %) males and ten (33.3 %) females. Mean age was 7.8 with a range of 3–12. Clinically significant medical history, diagnosis and operations are summarized in Table 2. 23 (76.6 %) of the patients were operated for OSAS whereas seven (23.3 %) of them for recurrent tonsil infections. Clinically significant medical history included hypothyroidism in seven (23.3 %), atrial septal defect (ASD) in seven patients (23.3 %) and ASD and ventricular septal defect (VSD) in one (3.3 %) patient. All of the patients underwent AT and one patient had bilateral tympanostomy tube insertion at the same operation. Hospital course of patients and complications are summarized in Table 3. Anesthetic complications occurred in two (6.6 %) patients. 1 patient with cardiac operation history had bradycardia during and after the operation and also experienced respiratory difficulty after extubation. This patient required an intensive care unit admission without intubation for 14 days because of persistent bradycardia. A temporary pacemaker was placed just after the surgery, since bradycardia did not resolve finally a regular pacemaker was implanted. The second patient had the history of ASD and experienced respiratory difficulty after extubation. Both of the patients were managed with oxygen, ipratropium bromide and albuterol sulfate inhalation aerosols. Mean hospital stay was 1.26 days with a range of 1–3 days. Mean duration for start of oral intake was 1.24 days with a range of 1–2 days. There was no early postop hemorrhage, but three (10 %) patients had late hemorrhage between days 7 and 10 and required bleeding control under anesthesia. Those hemorrhages were mild, patients did not need any blood transfusion and they were discharged within 24 h after the operation. Mean follow-up duration was 23 months with a range of 7–42 months. None of the patients needed reintubation, there were no atlanto-axial subluxation.
Discussion
Our results showed that complications of AT in DS children are not very rare. We found out that 6.6 % of the patients had respiratory difficulty, 3.3 % of patients had bradycardia, 10 % of patients had late bleeding which required surgical intervention. Besides our patients had longer hospital stay and late onset of adequate oral intake when compared to the normal population in the literature [14].
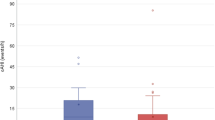
It is known that AT in children with DS has not the same efficacy when compared with normal population [9]. Shete et al. [9] found out that although some parameters in polysomnography (PSG) of DS children have improved, they are not as dramatic as in non-DS children [9]. They have compared 11 DS children with nine non-DS children; on postop PSG DS children’s mean Apnea Hypopnea index (AHI) decreased from 15.3 to 9.1 and non-DS children’s AHI decreased from 21.1 to 1.8 [9]. They also found that 55 % of the DS children required CPAP and BiPAP and 18 % required nocturnal oxygen after AT [9]. In our study, none of the DS children required CPAP or BiPAP during follow-up. This controversy may be a result of associated co-morbidities and patient characteristics.
Upper airway obstruction in children with DS is caused by multiple factors; hypertrophic adenoids and tonsils, relatively large tongue and base of tongue, collapse in soft palate and hypopharynx, abnormal laryngeal and tracheal structures [3]. In a study which evaluated 239 DS patients, it was found that trachea–bronchial pathology is much more common than the general population, especially tracheal problems and subglottic stenosis [6].
Shott and Donnelly [10] evaluated 15 DS children who had abnormal PSG after AT with cine magnetic resonance imaging. They found adenoid regrowth in 53 % of the patients, glossoptosis in 80 % of the patients, nasopharyngeal collapse in 60 % of the patients, hypopharyngeal collapse in 87 % of the patients [10]. These results are indicating the necessity of long-term follow-up and intervention either with reoperation or CIPAP/BiPAP in DS children.
Central sleep apnea (CSA) is somewhat overlooked in DS patients when compared to OSA. It is suggested that there is a vicious cycle between OSA and CSA and increased airway resistance leads to elevated CO2 levels which stimulate central chemoreceptors causing upper airway relaxation and unbalanced respiratory muscle activity [11–13]. In 2015, Thottam et al. [2] demonstrated 41.6 % of DS children with OSA have also CSA. They have also documented that 66.7 % resolution in CSA after AT operation in the same children [2]. They concluded that AT helped resolution of CSA by eliminating obstruction-linked CO2 retention and this has critical value in DS patients which has already narrow airway [2].
Goldstein et al. [14] compared the postoperative complications of AT between 87 DS children and 64 non-DS patients. They have reported that 8 % of DS patients had experienced anesthetic complications whereas non-DS patients had not [14]. Our results are similar with two patients (6.6 %) experiencing anesthetic complications; one patient bradycardia during operation and respiratory distress after extubation and other patient respiratory distress after extubation. They also reported that 25 % of the DS children required postoperative intensive care unit (PICU) admission which is higher than our PICU admission ratio, 3.3 %. They mentioned they use the PICU half electively and half because of perioperative respiratory complications [14]. We did not prefer to use PICU for elective purposes since this may delay start of oral intake and lengthen hospital stay.
Roodman et al. [15] reported bradycardia in three DS patients with sevoflurane. They mentioned that this might be a random occurrence and also might be related to the concentration of sevoflurane [15]. In our series, 90 % of the patients received sevoflurane and none of them had experienced bradycardia. The patient who experienced bradycardia was among our patients who have received desflurane. Bai et al. [16] evaluated 96 DS children during and following inhalation induction of anesthesia with sevoflurane and they found a significantly higher prevalence and degree of bradycardia occurred in children with DS. They have reported that bradycardia was corrected by decreasing the concentration of sevoflurane and airway manipulation [16].
Patients with DS generally need to stay longer than the normal population because of late onset of oral intake and respiratory problems [5, 14]. Bower et al. [5] reported a mean hospital stay of 2.1 days and Goldstein et al. [14] reported 1.4 ± 1.1 days. Mean hospital stay was 1.26 days in our series likewise to the literature. We did not prefer to discharge DS patients same day after the surgery. We believe observation of vitals in this group of patients is critical because of their peculiarity.
Readmission rate to the hospital after AT because of dehydration and bleeding in DS patients was reported as 8 % in the literature [14]. We have a similar readmission rate of 10 %. We have readmitted three patients for late bleeding treatment between postop 7 and 10 days. We did not have to readmit any patient for dehydration. We kept the patients in the hospital until we were pretty sure that they have started oral intake properly and we continued intravenous hydration at the meantime.
DS patients may have postoperative respiratory complications which necessitate oxygen therapy, insertion of airway, positioning, treatment with bronchodilator inhalation aerosols, intravenous corticosteroids, and reintubation [1, 5, 14]. It was reported that 63 % of the DS patients required oxygen to keep their oxygen saturation above 90 % after AT [5]. Goldstein et al. [14] reported that none of their patients required reintubation, CPAP/BiPAP or tracheostomy after AT operation. These results are parallel to our findings; none of our patients required any of those respiratory treatments other than mild precautions such as oxygen supplementation and treatment with bronchodilator inhalation aerosols.
Preoperative evaluation of DS patients should include thyroid function tests, clearance for cardiac diseases and cervical spine stability examination [5]. Hypothyroidism and congenital cardiac diseases are common among DS patients. PSG is an objective tool for assessment of OSAS in DS patients and should be performed when it is available. Atlanto-axial subluxation (Griesel’s syndrome) is likely to happen in DS patients during AT [17, 18]. It is advised that patients with DS should have a preoperative neurologic examination and/or a cervical roentgenogram in the lateral, extension, and flexion positions [19]. We did not perform any radiologic imaging before surgery. Extreme care should be taken to prevent atlanto-axial subluxation. We have performed the AT in neutral position without any back roll. We avoided any flexion or extension to the neck. A mouth retractor is enough and no extension is required for AT in DS patients.
Conclusion
Our review of DS patients after AT revealed the perioperative and postoperative risks, especially bradycardia, respiratory distress and bleeding. AT can be performed in DS patients safely with extreme precaution which includes adequate preoperative evaluation, hospitalization until the onset of oral intake, discharge after maintenance of oxygen saturation over 90 %. Because of associated diseases and abnormal craniofacial anatomy of DS patients AT should be performed by the centers with the capability of intervention to the possible life-threatening complications.
References
Thottam PJ, Trivedi S, Siegel B, Williams K, Mehta D (2015) Comparative outcomes of severe obstructive sleep apnea in pediatric patients with Trisomy 21. Int J Pediatr Otorhinolaryngol 79(7):1013–1016. doi:10.1016/j.ijporl.2015.04.015 (Epub 2015 Apr 28)
Thottam PJ, Choi S, Simons JP, Kitsko DJ (2015) Effect of adenotonsillectomy on central and obstructive sleep apnea in children with down syndrome. Otolaryngol Head Neck Surg 153(4):644–648. doi:10.1177/0194599815587877 (Epub 2015 Jun 4)
Jacobs IN, Gray RF, Todd NW (1996) Upper airway obstruction in children with Down syndrome. Arch Otolaryngol Head Neck Surg 122(9):945–950
Bassell JL, Phan H, Leu R, Kronk R, Visootsak J (2015) Sleep profiles in children with Down syndrome. Am J Med Genet A 167A(8):1830–1835. doi:10.1002/ajmg.a.37096 (Epub 2015 Jun 23)
Bower CM, Richmond D (1995) Tonsillectomy and adenoidectomy in patients with Down syndrome. Int J Pediatr Otorhinolaryngol 33(2):141–148
Hamilton J, Yaneza MMC, Clement WA, Kubba H (2016) The prevalence of airway problems in children with Down’s syndrome. Int J Pediatr Otorhinolaryngol 81:1–4. doi:10.1016/j.ijporl.2015.11.027 (Epub 2015 Dec 07)
Ramia M, Musharrafieh U, Khaddage W, Sabri A (2014) Revisiting Down syndrome from the ENT perspective: review of literature and recommendations. Eur Arch Otorhinolaryngol 271(5):863–869. doi:10.1007/s00405-013-2563-4 (Epub 2013 May 21)
Merrell JA, Shott SR (2007) OSAS in Down syndrome: T&A versus T&A plus lateral pharyngoplasty. Int J Pediatr Otorhinolaryngol 71(8):1197–1203 (Epub 2007 May 29)
Shete MM, Stocks RM, Sebelik ME, Schoumacher RA (2010) Effects of adeno-tonsillectomy on polysomnography patterns in Down syndrome children with obstructive sleep apnea: a comparative study with children without Down syndrome. Int J Pediatr Otorhinolaryngol 74(3):241–244. doi:10.1016/j.ijporl.2009.11.006 (Epub 2010 Jan 25)
Shott SR, Donnelly LF (2004) Cine magnetic resonance imaging: evaluation of persistent airway obstruction after tonsil and adenoidectomy in children with Down syndrome. Laryngoscope 114(10):1724–1729
Baldassari CM, Kepchar J, Bryant L, Beydoun H, Choi S (2012) Changes in central apnea index following pediatric adenotonsillectomy. Otolaryngol Head Neck Surg 146(3):487–490. doi:10.1177/0194599811428118 (Epub 2011 Nov 10)
Ferri R, Curzi-Dascalova L, Del Gracco S, Elia M, Musumeci SA, Stefanini MC (1997) Respiratory patterns during sleep in Down’s syndrome: importance of central apnoeas. J Sleep Res 6(2):134–141
Skatrud JB, Dempsey JA, Badr S, Begle RL (1988) Effect of airway impedance on CO2 retention and respiratory muscle activity during NREM sleep. J Appl Physiol 65(4):1676–1685
Goldstein NA, Armfield DR, Kingsley LA, Borland LM, Allen GC, Post JC (1998) Postoperative complications after tonsillectomy and adenoidectomy in children with down syndrome. Arch Otolaryngol Head Neck Surg 124(2):171–176. doi:10.1001/archotol.124.2.171
Roodman S, Bothwell M, Tobias JD (2003) Bradycardia with sevoflurane induction in patients with trisomy 21. Paediatr Anaesth 13(6):538–540
Bai W, Voepel-Lewis T, Malviya S (2010) Hemodynamic changes in children with Down syndrome during and following inhalation induction of anesthesia with sevoflurane. J Clin Anesth 22(8):592–597. doi:10.1016/j.jclinane.2010.05.002
Welinder NR, Hoffmann P, Håkansson S (1997) Pathogenesis of non-traumatic atlanto-axial subluxation (Grisel’s syndrome). Eur Arch Otorhinolaryngol 254(5):251–254
Bhattarai B, Kulkarni AH, Kalingarayar S, Upadya MP (2009) Anesthetic management of a child with Down’s syndrome having atlanto axial instability. JNMA J Nepal Med Assoc 48(173):66–69
Harley EH, Collins MD (1994) Neurologic sequelae secondary to atlantoaxial instability in Down syndrome. Implications in otolaryngologic surgery. Arch Otolaryngol Head Neck Surg 120(2):159–165
Acknowledgments
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest.
This article does not contain any studies with human participants or animals performed by any of the authors. Study includes only retrospective chart review without any patient identifiable, so no patient participation and informed consent were required.
Additional information
This work was done in Ministry of Health Marmara University Education and Research Hospital.
Rights and permissions
About this article
Cite this article
Yumusakhuylu, A.C., Binnetoglu, A., Demir, B. et al. Is it safe to perform adenotonsillectomy in children with Down syndrome?. Eur Arch Otorhinolaryngol 273, 2819–2823 (2016). https://doi.org/10.1007/s00405-016-4012-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4012-7