Abstract
We report an evidence-based management algorithm for benign lymphoepithelial cysts (BLEC) of the parotid glands in HIV patients based on long-term outcomes after radiation therapy. From 1987 to 2013, 72 HIV-positive patients with BLEC of the parotid glands treated at our institutions were identified and their medical records were reviewed and analyzed. The primary endpoint of our study was to determine a dose response in HIV patients with BLEC. In group A (≤18 Gy), which received a median dose of 10 Gy (8–18), overall response (OvR), complete response (CR), partial response (PR), and local failure (LF) was experienced by 7, 7, 0, and 93 %, respectively. In group B (≥22.5 Gy), which received a median dose of 24 Gy (22.5–30), OvR, CR, PR, and LF was experienced by 88, 65, 23, and 12 %. Logistic regression revealed that higher dose (≥22.5 Gy) predicted for cosmetic control (p = 0.0003). Multiple regression analysis revealed higher dose predicted for cosmetic control (p = 0.0001) after adjusting for confounding variables (age, gender, race, HAART use, BLEC duration, and fractionation size). No patients in either group experienced RTOG grade ≥3 toxicities. A radiation dose of 24 Gy delivered in 12–16 fractions of 1.5–2 Gy per fraction provides long-term cosmetic control in HIV-positive patients with BLEC of the parotid glands.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At this time, approximately 1.2 million people in the United States are living with human immunodeficiency virus (HIV), with an estimated 50,000 new cases being diagnosed every year (CDC [1]). More than half of HIV-positive patients are diagnosed with head and neck pathology including opportunistic infections [2]. Whether benign or malignant, these lesions may lead to discomfort as well as cosmetic and functional problems [3]. In patients with HIV, the most common clinical manifestation of salivary gland involvement is non-specific, usually bilateral, parotid gland swelling [4]. This enlargement is usually secondary to the development of benign lymphoepithelial cysts (BLEC) within the parotid glands, and has been reported to occur in 6 and 10 % of HIV-positive adults and children, respectively [5]. Bilateral parotid enlargement together with CD8 lymphocytosis typically characterizes BLEC, and may also be associated with cervical adenopathy [6–8], Senn et al. [9, 10]. Not only does BLEC occur in salivary glands and their draining lymph nodes but also within the floor of mouth, tonsil, thyroid gland, intrathoracic region, and pancreas [11–15]. While these can be observed, treatment options for BLEC of the parotid glands include close observation, highly active antiretroviral therapy (HAART), aspiration, sclerotherapy, radiation therapy (RT), and surgery. Modern information on the management of BLECs with radiation is scanty [16–22]. We therefore analyzed the experience at our centers to examine if data may provide modern guidelines for this uncommon manifestation of HIV.
Materials and methods
Patients
Utilizing our institutional databases, we identified 72 HIV-positive patients who underwent RT for BLEC at our institution from 1987 to 2013. IRB approval was obtained for this retrospective study. Review of patient information included age, race, gender, age at BLEC diagnosis, BLEC duration, HAART use, RT technique and dose, toxicity, and long-term outcome.
Analysis
Chi-square, log-rank, logistic regression, and multiple regression analyses were performed utilizing SPSS V21.0 (SPSS Inc., Chicago, IL). The Kaplan–Meier method was used to calculate actuarial rates of progression. Both the patient and the treating physician evaluated treatment response. Each patient completed a subjective evaluation of their cosmetic response, and physicians reported their findings following physical examinations. The rationale behind this was to record the patient’s cosmetic satisfaction with their treatment as well as to record the physician’s objective findings. Treatment outcomes were assigned as either complete response (CR), partial response (PR), or local failure (LF). CR was defined as greater than or equal to 75 % reduction in parotid size and complete patient cosmetic satisfaction. PR was defined as less than 75 % reduction in parotid size or moderate cosmetic satisfaction. LF was defined as persistent or enlarged BLEC or cosmetic dissatisfaction. Toxicity was scored based on the Radiation Therapy Oncology Group (RTOG)/European Organization for Research and Treatment of Cancer (EORTC) radiation toxicity grading [20].
Results
Study cohort
The majority of patients were treated in the 1990s (25 patients, 34.7 %) and in the 2000s (26 patients, 36.1 %). Table 1 shows the demographics of the patients in this study based on their treatment outcomes. The median age at radiation treatment was 42 (7–70) years. Fifty patients (69 %) were male and 22 (31 %) were female. The median duration of BLEC prior to RT was 2 (1–6) years, and 48 (67 %) patients received HAART. The median follow-up period for all patients was 11 (1–26) years.
HAART therapy
Major advances in HIV treatment were made during the years over which our patients were treated with RT. HAART became the standard-of-care for treatment of patients infected with HIV but only reached widespread use and availability in late 1996. Prior to this year, 20/34 patients (58.8 %) received HAART while 28/38 patients (73.7 %) received HAART afterwards. Two-thirds of all patients in this study were receiving HAART under the guidance of an infectious disease physician either at the time of initial consultation or, more often, on follow-up. As a large portion of the patient population in this study consisted of underserved and underinsured individuals, patient adherence to HAART was an issue.
Radiation treatment
Nine patients (12.5 %) were treated in the late 1980, and 12 patients (16.7 %) underwent treatment between 2010 and 2012. Three patients underwent treatment with 60Co. Seven patients were treated with 4 MV photons, 54 with 6 MV photons, and 6 with electrons en-face (9, 12, 16 MeV). Two patients received treatment with mixed beams (6 MV + 12/16 MeV). The radiation techniques employed have been previously reported in great detail. Bilateral parotids were treated in all but two patients.
Dose response
Based on the total delivered dose, patients were stratified into two groups: group A consisted of 15 patients (21 %) who received a total dose of ≤18 Gy with a median dose of 10 Gy (8–18), and group B consisted of 57 patients (79 %) who received a total dose of ≥22.5 Gy with a median dose of 24 Gy (22.5–30). Treatment was delivered in 1.5 or 2 Gy fractions per day. Thirty eight (53 %) patients achieved a complete response and 13 (18 %) patients achieved a partial response. Twenty-one (29 %) patients developed a local failure. Fifty seven (79 %) patients comprised group B and received greater than 20 Gy with a median dose of 24 (22.5–30) Gy, while 15 (21 %) patients comprised group A and received less than 20 Gy with a median dose of 10 (8–18) Gy, only one patient received less than 24 Gy in group B. Table 2 shows a comparison of predictive variables and outcomes between groups A and B.
In group B, 38 of 57 patients (65 %) achieved a CR while 13 (23 %) achieved a PR. Thirty of the 38 patients who obtained a CR and ten of the 13 patients who obtained a PR have records of HAART initiation, respectively. In group A, only one response was a CR. Seven of 57 (12 %) patients in group B and 14 of 15 (93 %) patients in group A experienced LF. The three patients treated with 60Co developed LF. Less than half (38 %) of patients who experienced LF received HAART. Chi-square tests showed significant relationships between LF and dose (p = <0.0001), race (p = 0.021), HAART use (p = 0.001), and fractionation size (p = 0.003). Gender (p = 0.146) and duration of BLEC prior to RT (p = 0.22) were not found to be significantly associated with LF. Logistic regression showed higher dose (≥22.5 Gy) to significantly predict for OvR or cosmetic control (p = 0.0003). After adjusting for confounding variables including age, gender, race, HAART use, BLEC duration, and fractionation size, multiple regression analysis revealed only higher dose to significantly predict for cosmetic control (p = 0.0001). The median times in those who failed in groups A and B were 7 and 16 months, respectively, and these were significantly different by log-rank test (p < 0.0001). Figure 1 shows a Kaplan–Meier curve for cosmetic control for both RT groups and clearly demonstrates improved control in group B.
Toxicities
All experienced acute RT toxicities were either RTOG grade 1 or 2, and no patients experienced any RTOG grade 3 or greater toxicities. Specifically, less than half of patients experienced acute grade 1–2 xerostomia, grade 1 dermatitis, and grade 1 altered taste. Less than 10 % of patients experienced late grade 1 xerostomia, and all of these patients received ≥22.5 Gy. We did not find any radiation-induced secondary malignancies in either dose groups. More details regarding radiation toxicity have been previously reported.
Discussion
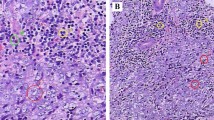
BLEC consists of benign, slowly enlarging multicystic lymphoepithelial lesions that can involve one or, more commonly, both parotid glands. While these lesions are typically soft and painless, they not only cause cosmetic disfigurement and patient distress but can also reveal one’s HIV status [23]. They can also arise in HIV-negative patients who have Mikulicz’s disease, myoepithelial sialadenitis, and Sjögren’s syndrome. Although the exact pathogenesis of BLEC remains unclear, it is thought to result from extra-glandular lymphoid infiltration and/or intra-glandular lymphoid proliferation with either ductal obstruction and/or epithelial entrapment. The consequent obstruction may cause cyst formation, parotid enlargement, and destruction of nearby acinar tissue which may result in xerostomia [24–28]. The diagnostic evaluation for BLEC of the parotids involves history and physical evaluation, HIV serum testing in patients without a confirmed HIV diagnosis, CT and/or MRI revealing multiple thin-walled cysts, and fine needle aspiration (FNA) [29]. Treatment options for BLEC include close observation, repeat aspiration, HAART in those naive to anti-retrovirals, sclerotherapy, radiotherapy, and surgery [29]. While observation has remained an option due to the slowly progressive nature of the disease, any acute enlargement warrants immediate investigation. FNA has been demonstrated as an effective diagnostic tool in monitoring for the development of EBV-associated B cell lymphoma, for which these patients are at increased risk [28, 30]. The current standard of care for treatment of HIV is HAART, regardless of whether the patient has BLEC. Interestingly, HAART alone has been shown to reduce and eliminate BLEC in some patients [31]. Some patients may undergo aspiration, which is quick and can be performed on an outpatient basis [23, 29, 32, 33].
Sclerotherapy with doxycycline or bleomycin has also been used, with studies showing an average reduction in cyst size by 40–100 % without any serious complications such as facial nerve injury or infection [12, 23, 34, 35]. The main disadvantage of both of these procedures, however, is that most treated lesions recur with continued enlargement. Surgical resection is rarely recommended as first-line treatment given the bilateral and progressive nature of the disease. There is also some risk (2–6 % in one study) of facial nerve injury, as well as a high likelihood of the need for multiple surgical procedures following superficial parotidectomy [29].
Previous studies have demonstrated the efficacy and tolerability of radiation therapy in treating HIV-associated BLEC of the parotid glands [16–19, 21, 22]. Goldstein et al. initially showed encouraging response rates following administration of 8–10 Gy; however longer follow-up revealed a median control duration of only 9.5 months [16–18]. As a result, the efficacy of higher dose was investigated. Beitler et al. treated HIV-positive patients with BLEC with 24 in 1.5 Gy daily fractions with results demonstrating excellent local control after a median follow-up of 24 months [21]. Comparison of these updated results with those of the earlier series [17, 18] showed a significant improvement in cosmetic control (p < 0.02 by log-rank test). They concluded that 24 Gy delivered in 1.5 Gy fractions is a safe, well-tolerated regimen that appears to be effective in 70 % of patients. In a later study of 30 patients at BIMC with a median follow-up of 66 months, Mourad et al. found an OvR in 93 % of patients treated with 24 Gy delivered to bilateral parotids in 1.5–2 Gy daily fractions; with no RTOG >2 toxicities [19]. Chi-square test showed a significant relationship between OvR and RT duration (p < 0.001), and there was a trend towards higher CR rate with 2 Gy daily fractions (p = 0.053). In a study of 37 patients, Mourad et al. compared response rates between 15 patients who received ≤18 Gy (median 10 Gy, range 8–18 Gy) and 18 patients who received 24 Gy [19]. At a median follow-up of 35 months, the CR, PR, and LF rates were 7 vs. 55 %, 0 vs. 14 %, and 93 vs. 32 %, respectively, when comparing the lower and higher dose groups. Logistic regression analysis showed that 24 Gy was associated with a decrease in local failure (p < 0.0001). Multiple regression analysis revealed higher dose to predict for OvR after adjusting for age, gender, race, HAART use, BLEC duration, and fractionation size (p = 0.042).
In this combined follow-up study, we examined the medical records of 72 patients treated at our institutions between 1987 and 2013 with a median follow-up of 11 years. We found a significant relationship between LF and dose, race, HAART use, and fractionation size by Chi-square tests. Similarly, to our prior study, higher dose was found to significantly predict for OvR or cosmetic control. In performing multiple regression analysis, only higher dose remained significant in predicting for OvR after adjusting for all examined potentially confounding variables. After reviewing the literature and our experience with HIV-associated BLEC of the parotids, we recommend the diagnostic and treatment algorithm shown in Fig. 2 for these patients. As long as there is no medical contraindication, HAART should be initiated prior to RT. Three-dimensional conformal radiation therapy (3DCRT) or intensity modulated radiation therapy (IMRT) should be employed in the treatment of these patients in order to limit radiation dose to the adjacent structures, with the parotids constrained to a mean dose below 26 Gy [36, 37]. While the importance of HAART in management of patients with HIV regardless of BLEC is unquestionable, compliance with this therapy remains an issue. Our patient population consisted largely of underserved minorities with a lower socioeconomic status and limited patient resources, which likely play a role in determining patient adherence to this therapy [38]. While some research has been conducted examining the relationship between socioeconomic status with patient adherence to radiation therapy, further investigation is warranted [39–42]. In our patient cohort, treatment interruptions were primarily due to psychosocial and logistical issues (such as transportation) rather than medical factors. Thus we believe that all HIV-positive patients with BLEC should be referred to psychosocial services and social work for additional support, which could increase their adherence to both HAART and RT. In treating patients with any dose of radiation, there is always a small but potential risk of inducing a secondary malignancy given that carcinogenesis is believed to be a stochastic effect of RT. We reviewed the literature and did not find any documented case of radiation induced malignancy (RIM) or sarcoma (RIS) after RT for BLEC of the parotids. Nonetheless, as the survival of HIV-positive patients has drastically improved with HAART, all patients with BLEC presenting for evaluation for RT should be informed of this potential risk. Historically, many radiation oncologists have attributed doses in excess of 30 Gy with the development of RIS [43, 44] however, Mourad et al. reported the first case in the American literature of RIS after radiation prophylaxis for benign disease (heterotopic ossification) with doses as low as 7 Gy [45–48].
Given the recent advances in HIV/AIDS medical management and the resultant increase in life expectancy of infected patients, the number of patients with BLEC of the parotid glands is expected to increase (Mills et al. [49, 50]). Thus BLEC of the parotid glands will become a more common presenting diagnosis and will warrant further workup and treatment.
This study represents the largest known review of patients with HIV-associated BLEC of the parotids treated with RT with the longest follow-up and the largest experience utilizing modern planning techniques. The weaknesses of our study include differing RT techniques and the nonrandomized retrospective nature of this analysis with its inherent dependence on pre-existing documentation. Furthermore, approximately 50 % of the patient population represented in this study consisted largely of underserved and underinsured individuals making HAART adherence an issue.
In conclusion, based on our patient experiences, we recommend radiation treatment of HIV-associated BLEC of the parotid glands should consist of 24 Gy delivered in 12 fractions of 2 Gy or 16 once-daily fractions of 1.5 Gy. This regimen is well-tolerated, and results in excellent and durable cosmetic control.
References
CDC (2013) HIV in the United States: at a glance. http://www.cdc.gov/hiv/pdf/statistics_basics_factsheet.pdf. Accessed 21 Mar 2014
Yengopal V, Naidoo S (2008) Do oral lesions associated with HIV affect quality of life? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(1):66–73
Adedigba MA, Ogunbodede EO, Jeboda SO et al (2008) Patterns of oral manifestation of HIV/AIDS among 225 Nigerian patients. Oral Dis 14(4):341–346
Marsot-Dupuch K, Quillard J, Meyohas MC (2004) Head and neck lesions in the immunocompromised host. Eur Radiol 14(3):E155–E167
Mandel L, Reich R (1992) HIV parotid gland lymphoepithelial cysts. Review and case reports. Oral Surg Oral Med Oral Pathol 74(3):273–278
Kreisel FH, Frater JL, Hassan A et al (2010) Cystic lymphoid hyperplasia of the parotid gland in HIV-positive and HIV-negative patients: quantitative immunopathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109(4):567–574
Mandel L, Kim D, Uy C (1998) Parotid gland swelling in HIV diffuse infiltrative CD8 lymphocytosis syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85(5):565–568
Schrot RJ, Adelman HM, Linden CN, Wallach PM (1997) Cystic parotid gland enlargement in HIV disease. The diffuse infiltrative lymphocytosis syndrome. JAMA 278(2):166–167
Senn N, Bron L, Cavassini M (2006) Lymphoepithelial cysts of the parotid gland: a pathology linked to HIV infection. Rev Med Suisse 2(66):1348–1350, 1352
Tripathi AK, Gupta N, Ahmad R, Bhandari HS, Kalra P (2004) HIV disease presenting as parotid lymphoepithelial cysts: a presumptive diagnosis of diffuse infiltrative lymphocytic syndrome (DILS). J Assoc Physicians India 52:921–923
Brudnicki AR, Levin TL, Slim MS, Moser J, Amin N (2001) HIV-associated (non-thymic) intrathoracic lymphoepithelial cyst in a child. Pediatr Radiol 31(8):603–605
Echavez MI, Lee KC, Sooy CD (1994) Tetracycline sclerosis for treatment of benign lymphoepithelial cysts of the parotid gland in patients infected with human immunodeficiency virus. Laryngoscope 104(12):1499–1502
Favia G, Capodiferro S, Scivetti M et al (2004) Multiple parotid lymphoepithelial cysts in patients with HIV-infection: report of two cases. Oral Dis 10(3):151–154
Lustig LR, Lee KC, Murr A et al (1998) Doxycycline sclerosis of benign lymphoepithelial cysts in patients infected with HIV. Laryngoscope 108(8 Pt 1):1199–1205
Weidner N, Geisinger KR, Sterling RT et al (1986) Benign lymphoepithelial cysts of the parotid gland. A histologic, cytologic, and ultrastructural study. Am J Clin Pathol 85(4):395–401
Goldstein J, Rubin J, Silver C et al (1992) Radiation therapy as a treatment for benign lymphoepithelial parotid cysts in patients infected with human immunodeficiency virus-1. Int J Radiat Oncol Biol Phys 23(5):1045–1050
Beitler JJ, Smith RV, Silver CE et al (1995) Cosmetic control of parotid gland hypertrophy using radiation therapy. AIDS Patient Care 9(6):271–275
Beitler JJ, Vikram B, Silver CE et al (1995) Low-dose radiotherapy for multicystic benign lymphoepithelial lesions of the parotid gland in HIV-positive patients: long-term results. Head Neck 17(1):31–35
Mourad WF, Hu KS, Shourbaji RA et al (2013) Radiation therapy for benign lymphoepithelial cysts of parotid glands in HIV patients. Laryngoscope 123(5):1184–1189
Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 31(5):1341–1346
Beitler JJ, Smith RV, Brook A et al (1999) Benign parotid hypertrophy on+ HIV patients: limited late failures after external radiation. Int J Radiat Oncol Biol Phys 45(2):451–455
Mourad WF, Young R, Kabarriti R et al (2013) 25-year follow-up of HIV-positive patients with benign lymphoepithelial cysts of the parotid glands: a retrospective review. Anticancer Res 33(11):4927–4932
Steehler MK, Steehler MW, Davison SP (2012) Benign lymphoepithelial cysts of the parotid: long-term surgical results. HIV AIDS (Auckl) 4:81–86
Elliott JN, Oertel YC (1990) Lymphoepithelial cysts of the salivary glands. Histologic and cytologic features. Am J Clin Pathol 93(1):39–43
Mayer M, Haddad J Jr (1996) Human immunodeficiency virus infection presenting with lymphoepithelial cysts in a six-year-old child. Ann Otol Rhinol Laryngol 105(3):242–244
Patton LL, van der Horst C (1999) Oral infections and other manifestations of HIV disease. Infect Dis Clin North Am 13(4):879–900
Al-Maawali AA, Chacko AP, Javad H et al (2008) HIV disease presenting as a unilateral parotid gland swelling. Indian J Pediatr 75(10):1087–1088
Sperling NM, Lin PT, Lucente FE (1990) Cystic parotid masses in HIV infection. Head Neck 12(4):337–341
Dave SP, Pernas FG, Roy S (2007) The benign lymphoepithelial cyst and a classification system for lymphocytic parotid gland enlargement in the pediatric HIV population. Laryngoscope 117(1):106–113
Sperling NM, Lin PT (1990) Parotid disease associated with human immunodeficiency virus infection. Ear Nose Throat J 69(7):475–477
Syebele K, Butow KW (2011) Comparative study of the effect of antiretroviral therapy on benign lymphoepithelial cyst of parotid glands and ranulas in HIV-positive patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111(2):205–210
Shaha AR, DiMaio T, Webber C et al (1993) Benign lymphoepithelial lesions of the parotid. Am J Surg 166(4):403–406
Terry JH, Loree TR, Thomas MD et al (1991) Major salivary gland lymphoepithelial lesions and the acquired immunodeficiency syndrome. Am J Surg 162(4):324–329
Berg EE, Moore CE (2009) Office-based sclerotherapy for benign parotid lymphoepithelial cysts in the HIV-positive patient. Laryngoscope 119(5):868–870
Monama GM, Tshifularo MI (2010) Intralesional bleomycin injections in the treatment of benign lymphoepithelial cysts of the parotid gland in HIV-positive patients: case reports. Laryngoscope 120(2):243–246
Hey J, Setz J, Gerlach R et al (2011) Parotid gland-recovery after radiotherapy in the head and neck region—36 months follow-up of a prospective clinical study. Radiat Oncol 6:125
Hey J, Setz J, Gerlach R et al (2009) Parotid-gland-sparing 3D conformal radiotherapy in patients with bilateral radiotherapy of the head and neck region—results in clinical practice. Oral Oncol 45(2):e11–e17
Falagas ME, Zarkadoulia EA, Pliatsika PA et al (2008) Socioeconomic status (SES) as a determinant of adherence to treatment in HIV infected patients: a systematic review of the literature. Retrovirology 5:13
Patel UA, Patadia MO, Holloway N et al (2009) Poor radiotherapy compliance predicts persistent regional disease in advanced head/neck cancer. Laryngoscope 119(3):528–533
Patel UA, Thakkar KH, Holloway N (2008) Patient compliance to radiation for advanced head and neck cancer at a tertiary care county hospital. Laryngoscope 118(3):428–432
Sethi RA, Stamell EF, Price L et al (2010) Head and neck radiotherapy compliance in an underserved patient population. Laryngoscope 120(7):1336–1341
Chen AM, Jennelle RL, Grady V et al (2009) Prospective study of psychosocial distress among patients undergoing radiotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys 72:187–193
Arlen M, Higinbotham NL, Huvos AG et al (1971) Radiation-induced sarcoma of bone. Cancer 28(5):1087–1099
Kim JH, Chu FC, Woodard HQ et al (1978) Radiation-induced soft-tissue and bone sarcoma. Radiology 129(2):501–508
Mourad WF, Saad AA, Hussein MA et al (2010) Postradiation therapy sarcoma. J Clin Oncol 28(15):e20523
Mourad WF, Packianathan S, Baird MC et al (2010) Radiation induced malignancy after prophylactic radiation therapy in prevention of heterotopic ossification. Int J Radiat Oncol Biol Phys 78(3):sP610
Mourad WF, Shourbaji RA, Russel G et al (2012) Radiation-induced sarcoma following radiation prophylaxis of heterotopic ossification. Pract Radiat Oncol 2:151–154
Farris MK, Chowdhry VK, Lemke S et al (2012) Osteosarcoma following single fraction radiation prophylaxis for heterotopic ossification. Radiat Oncol 7:140
Mills EJ, Bakanda C, Birungi J et al (2011) Life expectancy of persons receiving combination antiretroviral therapy in low-income countries: a cohort analysis from Uganda. Ann Intern Med 155(4):209–216
Thompson MA, Aberg JA, Hoy JF et al (2012) Antiretroviral treatment of adult HIV infection: 2012 recommendations of the International Antiviral Society–USA panel. JAMA 308(4):387–402
Acknowledgments
The authors thank Dr. Drew Moghanaki, MD, MPH, (Hunter Holmes McGuire Veterans Affairs Hospital, Richmond, VA) for his thoughtful comments and editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors do not have any conflict of interest.
Rights and permissions
About this article
Cite this article
Mourad, W.F., Patel, S., Young, R. et al. Management algorithm for HIV-associated parotid lymphoepithelial cysts. Eur Arch Otorhinolaryngol 273, 3355–3362 (2016). https://doi.org/10.1007/s00405-016-3926-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-3926-4