Abstract
In 2013, a total of 84,332 patients had undergone extracapsular tonsillectomies (TE) and 11,493 a tonsillotomy (TT) procedure in Germany. While the latter is increasingly performed, the number of the former is continually decreasing. However, a constant number of approximately 12,000 surgical procedures in terms of abscess-tonsillectomies or incision and drainage are annually performed in Germany to treat patients with a peritonsillar abscess. The purpose of this part of the clinical guideline is to provide clinicians in any setting with a clinically focused multi-disciplinary guidance through the surgical treatment options to reduce inappropriate variation in clinical care, improve clinical outcome and reduce harm. Surgical treatment options encompass intracapsular as well as extracapsular tonsil surgery and are related to three distinct entities: recurrent episodes of (1) acute tonsillitis, (2) peritonsillar abscess and (3) infectious mononucleosis. Conservative management of these entities is subject of part I of this guideline. (1) The quality of evidence for TE to resolve recurrent episodes of tonsillitis is moderate for children and low for adults. Conclusions concerning the efficacy of TE on the number of sore throat episodes per year are limited to 12 postoperative months in children and 5–6 months in adults. The impact of TE on the number of sore throat episodes per year in children is modest. Due to the heterogeneity of data, no firm conclusions on the effectiveness of TE in adults can be drawn. There is still an urgent need for further research to reliably estimate the value of TE compared to non-surgical therapy of tonsillitis/tonsillo-pharyngitis. The impact of TE on quality of life is considered as being positive, but further research is mandatory to establish appropriate inventories and standardized evaluation procedures, especially in children. In contrast to TE, TT or comparable procedures are characterized by a substantially lower postoperative morbidity in terms of pain and bleeding. Although tonsillar tissue remains along the capsule, the outcome appears not to differ from TE, at least in the pediatric population and young adults. Age and a history of tonsillitis are not a contraindication, abscess formation in the tonsillar remnants is an extremely rare finding. The volume of the tonsils should be graded according to Brodsky and a grade >1 is considered to be eligible for TT. The number of episodes during 12 months prior to presentation is crucial to indicate either TE or TT. While surgery is not indicated in patients with less than three episodes, a wait-and-see policy for 6 months is justified to include the potential of a spontaneous healing before surgery is considered. Six or more episodes appear to justify tonsil surgery. (2) Needle aspiration, incision and drainage, and abscess tonsillectomy are effective methods to treat patients with peritonsillar abscess. Compliance and ability of the patient to cooperate must be taken into account when choosing the surgical method. Simultaneous antibiotic therapy is recommended but still subject of scientific research. Abscess tonsillectomy should be preferred, if complications have occurred or if alternative therapeutic procedures had failed. Simultaneous TE of the contralateral side should only be performed when criteria for elective TE are matched or in cases of bilateral peritonsillar abscess. Needle aspiration or incision and drainage should be preferred if co-morbidities exist or an increased surgical risk or coagulation disorders are present. Recurrences of peritonsillar abscesses after needle aspiration or incision and drainage are rare. Interval TE should not be performed, the approach is not supported by contemporary clinical studies. (3) In patients with infectious mononucleosis TE should not be performed as a routine procedure for symptom control. TE is indicated in cases with clinically significant upper airway obstruction resulting from inflammatory tonsillar hyperplasia. If signs of a concomitant bacterial infection are not present, antibiotics should not be applied. Steroids may be administered for symptom relief.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of recurrent episodes of acute tonsillitis by means of tonsil surgery was suggested already in the Atharvaveda (700 b.c.) and the Corpus Hippocraticum (400 b.c.). Cornelius Celsus (first century) described a crude procedure using a hook or the index finger to separate the tonsillar tissue from the adjacent structures, hemostais was achieved by application of a vinegar-milk mixture. Due to a lack of proper anesthesia, a variety of tonsillotomes were created in the nineteenth and twentieth century to shorten the operation time. Due to the surgical technique—it was in fact a tonsillotomy—tonsillar remnants were frequently left behind.
George Earnest Waugh from England was the first to use a careful extracapsular dissection method with a complete removal of the palatine tonsils in 1909. His method was increasingly accepted worldwide, supported by further developments including the use of a mouth gag, tongue-depressors, electrosurgery and improvements on anesthesia techniques.
A rapidly increasing number of dedicated tonsil hospitals were established to offer a valid therapy for prevention of sore throats, streptococcal infections and post-streptococcal diseases in an era without antibiotic treatment. The most important promoting factor in the extraordinary widespread of tonsillectomy was the acceptance of the focal infection theory. The belief that multiple diseases such as rheumatic fever, endocarditis, myocarditis, pericarditis, nephritis, pancreatitis, chorea, peptic ulcer, appendicitis, arthritis resulted from the dissemination of pathogens through the bloodstream from a local focus, namely the tonsils and/or teeth.
It is noteworthy to emphasize, that the term “sore throat” summarizes different clinical pictures, which are presumably different entitites: tonsillitis, pharyngitis or combination of both. Moreover, terms like “recurrent acute tonsillitis” and “chronic tonsillitis” are mixed loosely by most authors which impedes direct comparison of contemporary studies. Burton et al. suggested to distinguish between “recurrent acute tonsillitis” (>2 distinct episodes in a 12-month period) and “chronic tonsillitis” (symptoms of tonsillitis for a period longer than 3 months).
The purpose of this part of the clinical guideline is to provide clinicians in any setting with a clinically focused multi-disciplinary guidance through the surgical treatment options to reduce inappropriate variation in clinical care, improve clinical outcome and reduce harm. Surgical treatment options encompass intracapsular as well as extracapsular tonsil surgery and are related to three distinct entities: recurrent episodes of acute tonsillitis, peritonsillar abscess and infectious mononucleosis.
Materials and methods
Details concerning guideline scope and purpose, target audience, various definitions and grade of recommendations are obtainable in part I of this clinical guideline.
Literature review
In July 2014, the keywords of “tonsillitis tonsillectomy review”, “sore throat tonsillectomy review”, and “guideline tonsillectomy review” in combination with the filter of “last 5 years” identified 89 articles in Pubmed of which 85 were excluded due to at least one of the following criteria: no discussion of the surgical indication, exclusively pathophysiological reviews, repetition of the indications of medical societies, no analysis of patient data, reference to outdated data before 1984, or publication not in German or English language. In the library of the Cochrane Collaboration we used “tonsillectomy” as keyword in December 2014 [1].
Extracapsular tonsillectomy (TE)
This procedure aims to remove the entire tissue of the palatine tonsils with different instruments. A simultaneous resection of the lingual tonsil is not included in this intervention. To date, a certain age up to which the tonsils are essential for the immune system cannot be scientifically defined. In general, during dissection the vessels with larger caliber are transected at the exterior of the tonsillar capsule and closed with sutures or electrosurgical measures. “Hot” dissection means that electrosurgical instruments are used, either for dissection and/or hemostasis. These instruments use not only monopolar or bipolar coagulation methods, but also different types of LASER and radiofrequency devices. The so-called “cold” dissection method avoids any application of electrosurgical means for dissection of the tonsils. Intraoperative bleedings may be controlled either by ligature or electro-surgical measures. Despite the different surgical methods, the surrounding pharyngeal muscles are directly damaged during the procedure with exposure of injured vessels and neural ends in the wound. The result of such an exposure is the secondary contact to bacteria- and enzyme-containing saliva, a factor that may contribute to the significant postoperative morbidity in terms of pain and bleeding (4.5 % on average). The intensity of post-tonsillectomy hemorrhage varies and may become life-threatening and even lethal in extremely rare cases. Most authors distinguish between primary (<24 h) and secondary hemorrhage (>24 h) [2, 3], but other classifications are obtainable in the literature [4–7]. The most comprehensive classification was suggested by Sarny et al. [8] and includes onset, intensity and bleeding site. Cold-dissection TE is associated with increased intraoperative bleeding and impaired vision compared to hot techniques. While the latter is associated with an increased risk of secondary hemorrhage and pain, primary hemorrhage occurs more frequently in the former surgical method [9]. Despite these considerations, no particular method is accepted as a gold standard to date [10–15]. According to the meta-analysis of Dhiwakar et al. [16], postoperative pain cannot be significantly reduced by the routine application of antibiotics. Cardozo et al. [17] revealed a significant dose–response relationship between applied intraoperative diathermy energy and postoperative pain. However, postoperative pain therapy is subject of a different guideline, currently under revision [18].
Albeit technically trivialized, TE is potentially associated with a number of complications which have to be included in the informed consent (Table 1).
Intracapsular tonsillectomy (e.g. tonsillotomy; TT)
Patients with tonsillar hypertrophy are potential candidate for this surgical technique which aims to downsize the volume of the tonsils without exposing the tonsillar capsule. This approach is dramatically reduces the postoperative morbidity and will be described in a separate chapter of this guideline.
Results
Recurrent acute tonsillitis
First clinical studies revealing the positive impact of TE—measured in terms of the reduction of sore throat episodes per year—in large patient populations, were published by Kaiser [19], Roydhouse [20], Mawson [21, 22], and McKee [23]. Some of these studies were included in the meta-analyses of Marshall [24] and van Staaij et al. [25]. Marshall focused on the number of throat infections per year as well as the average number of episodes avoided by TE as endpoints of his meta-analysis [24]. Van Staaij evaluated the reduction of the number of episodes but also the days of absence at school, upper airway infections as well as the number of medical consultations because of airway infections. Both meta-analyses, however, included studies (1) neglecting the effect of adenoids on sore throat and upper airway obstruction, (2) not distinguishing between recurrent-acute and chronic tonsillitis, (3) not considering the outcome, (4) accepting heterogeneity of the subgroups, (5) without randomization, (6) with poorly defined inclusion criteria such as age, number, severity, and duration of the throat infections. Therefore, the panelists of this guideline also excluded other studies [26–28] supported by the statement of Burton et al. [29]. The literature review in the Medline [30] identified the following four papers:
1. Barraclough and Anari [31] who reviewed the literature published between 1960 to July 2013 with emphasis on younger patients (≤16 years). Eight studies dealt with the effectiveness of TE (endpoints: number/severity of the episodes), 5 of them dated from 1970 or earlier so that they will not be included in the present paper because of the aforementioned exclusion criteria [21–23, 32, 33]. The remainder included studies published by Paradise et al. [34, 35] and Staaij et al. [36] revealing the superiority of surgical therapy under certain conditions (for details see below). The authors also identified three studies dealing with the costs of therapeutic modalities as endpoint [37–39]: (1) Buskens et al. [38] could not reveal a significant cost reduction by surgical therapy as calculated for children aged between 2 and 8 years and only mild symptoms. (2) Lock et al. conclusions from two studies contrast sharply with the latter study, with reduced costs of therapy in children 4–15 years of age [37]. Barraclough and Anari compiled 16 non-randomized studies, dealing with the parents postsurgical satisfaction, quality of life, psychological changes, and influence of the body growth [40–55]. Only 6 of those 16 studies focused on sore throat, three of them did not specify the findings and thus are not appropriate for further consideration in the current context [56–58]. The remaining 3 studies published by Conlon et al. [49], Goldstein et al. [59], and Fujihara et al. [52] reported exclusively on the success of TE. All parents of 80 children (2–14 years of age) were satisfied with the surgical outcome 1 year after surgery, evaluated by a questionnaire. TE was indicated if more than four episodes within the previous 2 years or more than five within the last year had been treated (endpoints: severity of sore throat, sleeping behavior and general behavior) [49]. Fujihara et al. reported superior results after TE in 25 children (2–15 years of age) as well as 16 adults (endpoints: number of fever episodes, medical consultations, days off at school/work 1 year before and after surgery). TE was indicated according to suggestions of the American Academy (for details, see below). Costs of TE were outweighed after 1.6 (children) and 2.5 years (adults) [52]. Lastly, Goldstein et al. used a validated questionnaire to assess the course of 38 children (2–16 years of age) 1 year after surgery with ≥3 tonsillitis episodes or ≥3 antibiotic therapies or ≥3 months of continuous throat infection in their history. Specific symptoms as well as the quality of life of this patient population were significantly improved after TE [59]. Barraclough and Anari mentioned that the disease is incompletely assessed if only the number of e pisodes is counted even if this is necessary for statistical calculations in a randomized-controlled trial (RCT). Moreover, validated questionnaires are not free of confounding factors and studies reflecting the view of the affected children were still missing [31]. Barraclough and Anari refer to a meta-analysis of Blakeley and Magit [60], stating that TE (with or without adenoidectomy) reduces the number of pharyngitis episodes by 43 %. However, calculation of the moderate effect of surgical therapy was based on the data of four studies [34–36, 61].
2. Andreou et al. [62] reported on the quality of life, 6 and 12 months after TE in patients older than 15 years of age. The authors included eight cohort studies in their meta-analysis with evidence of beneficial surgical therapy based on validated questionnaires [Glasgow Benefit Inventory (GBI) or Short-Form Questionnaire (SF-12)] [63–70] and listed confounding factors like type of randomization, different size of the population (40–217 patients), variable response rate (30–97 %), different age ranges of the patients, application of electro-surgical measures as by Schwentner et al. [65], and statistical deficits (confidence interval not provided). Except in studies with small patient populations, TE was beneficial in terms of an improved quality of life. The effect was related to young age (<30 years), severity of preoperative symptoms and limited in case of co-morbidities.
3. Motta et al. [71] evaluated the impact of the revised national tonsillectomy guideline in Italy by sending questionnaires to 14 hospitals. The authors revealed that the prevalence of surgery had not changed between 2002 and 2008. Moreover, 37.7 % of all interventions did not match the recommendations of the national guideline. One particularity of this publication is that surgery was recommended, when the antistreptolysin-O-titer (ASLO) had doubled. The authors strictly recommended to consider adenoid tissue as a source of upper airway obstruction, mandating adenotonsillectomy (ATE), particularly in sleep-related breathing disorders. This statement is supported by the American Academy of otolaryngology-Head and neck Surgery (AAO-HNS) but ignored by the Scottish Intercollegiate guideline network (SIGN). In contrast to all other national guidelines, the authors emphasize that adeno-tonsillar hyperplasia is significantly associated with middle ear diseases.
4. Senska et al. [68] evaluated the quality of life after TE, based on a standardized questionnaire that was adequately completed by 97 of 114 adult patients (18–62 years; median age: 26 years). At least three episodes of acute tonsillitis in the 12 months preceding TE were an indication for TE. On the day before and 14 months after surgery, the number of sore throat episodes, medical consultations, intake of antibiotics/analgesics as well as disease-related days-off at work were registered. During the postoperative telephone interview, questions from the GBI with three subscales were applied for evaluation of the general condition, the relation with family and friends, and the physical health status. Significant improvements were observed in all endpoints of this study, including GBI.
Bullet point summary
Adults
-
The quality of the studies varies considerably.
-
The long-term effect of TE remains unclear.
-
TE is capable to reduce the number of recurrent acute tonsillitis attacks and thus necessary therapies/medical consultations and increase the quality of life.
-
Co-morbidities reduce the effect of TE.
-
The effect of surgery increases with the severity of preoperative symptoms and a young age of less than 30 years.
Children
-
The impact of TE is mirrored by a high satisfaction rate of the parents but only a moderate reduction of the number of episodes indicating the need of a more sophisticated assessment tool.
-
The effect of TE on the number of episodes correlates with the severity of symptoms.
-
The beneficial effect may be limited in time.
-
In children with mild/moderate symptoms, TE does not outweigh the costs of therapy.
-
Some quality of life inventories are validated (Tonsil and Adenoid Health Status Instrument; Pediatric Throat Disorders Outcome; Glasgow Children’s Benefit Inventory; Child Behavior Checklist) but may encompass limitations, since there are no studies reflecting the children’s points of view.
-
The effect of TE on days-off at school varies significantly and depends on the inclusion criteria of studies.
-
The effect of TE is most clearly seen in the reduction of sore throat episodes and only to a lesser extent in other symptoms.
In the library of the Cochrane Collaboration [72] 21 hits were achieved, two of whom were relevant for this guideline [28, 73]. The first author of both contributions is identical (Martin Burton) who had revised the version of 2009 with a literature update ending by October 31, 2013 [73]. Several issues associated with the analysis were mentioned by the authors. (1) The symptoms may result either from tonsillitis or pharyngitis or tonsillo-pharyngitis-presumably different entities with different etiologies which is commonly neglected; (2) neither the incidence nor the intensity of sore throat in the patient’s history allows to predict the clinical course, i.e. spontaneous healing cannot be excluded; (3) terms like recurrent or chronic tonsillitis were mixed loosely and diagnosis was based at least in part exclusively on clinical symptoms without microbiological confirmation in some studies. The authors distinguished between recurrent tonsillitis (2 separate episodes within 12 months) and chronic tonsillitis (symptom duration for at least 3 months). Patients with or without antibiotic therapy were taken as control groups. Primary endpoints of the meta-analysis were the number and severity of the sore throat episodes, number of days with sore throat, and postoperative morbidity/mortality. Secondary endpoints were the consumption of antibiotics, analgesics, days-off at work/school as well as quality of life.
Pain resulting from the surgical procedure itself was included in statistical calculations only in RCT with children but not with adults. In the revised version of 2014, only 2 additional studies were included in the meta-analysis [37, 74] resulting in a total of 5 RCT with 987 children and 2 RCT with 156 adults (for details, see Table 2). In contrast to the aforementioned review of Barraclough [31], the authors included only 3 quality-of-life-studies [36, 37, 74] without a detailed data analysis. Burton et al. concluded that sufficient information about the effectiveness of TE/ATE was only available for the first year following surgery in children and for a shorter period (5–6 months) in adults. When the days of postoperative pain were included in the statistical calculations, surgically treated children suffered from 3.0 episodes during the first year after surgery in contrast to 3.6 episodes of sore throat in the control group. If limited to moderately affected children the difference was 1.1 in the TE group vs. 1.2 episodes in the control group. Considering exclusively episodes with mild pain intensity, 1.2 episodes of sore throat in the TE group occurred compared to 0.4 episodes in the control group (95 % confidence interval: +0.7 to +0.9). In the first postoperative year, children suffered from sore throat for 18 days (including the days of postoperative pains) compared to 23 days in the control group. Surgically treated children missed 2.3 days less school (95 % confidence interval: −3.4 to −1.2) compared to the children of the control group who were absent an average for 6 days. In this calculation, the surgery-related absences were not taken included.
Burton et al. assessed the data quality in both studies with adults as insufficient for statistical calculations (“low quality evidence”). Within the follow-up time of only 6 months, the number of episodes was reduced by 3.6 (95 % confidence interval: 7.9 more rarely to 0.7 more frequently). The difference between both studies, however, was significant: the reduction of the annual episodes of throat infection was 1.5 (95 % confidence interval: 2.3 fewer to 0.7 fewer) in the study of Alho et al. [61], and it was 5.9 (95 % confidence interval: 7.8 fewer to 0.79 fewer) in the study of Koskenkorva’s et al. [74]. The pooled mean difference for number of days with sore throat for about 6 months of follow-up was 10.6 days fewer in the group receiving surgery (95 % CI −15.5 to −5.8). The difference in the effect sizes reported by the two studies is substantial; the reduction in mean number of days with pain varied from 8.9 days fewer (95 % CI −14.0 to −3.9) in Alho et al. to 35.1 days fewer (95 % CI −54.0 to −16.2) in Koskenkorva et al. It should be noted, that the number of days with sore throat in the immediate postoperative periods was not taken into account in this analysis, which appeared to be 13 days (standard deviation: 4 days) in Alho et al. and 17 days (standard deviation: 6 days) in Koskenkorva et al. Moreover, the preoperative severity of symptoms was not graded. Only Koskenkorva mentioned the absences at work that were reduced by 3.3 days after TE (95 % confidence interval: −7.7 to +1.1), which is not significant.
Bullet point summary
General
-
The benefit of the intervention must be weighed against the disadvantages such as bleeding complications and postoperative pain.
-
It remains unclear if and to what extent exclusively the palatine tonsils are responsible for sore throat.
-
Sore throat may also result from pharyngitis or tonsillo-pharyngitis. Removing the tonsils will always prevent ‘tonsillitis’, but the impact of the procedure on sore throats due to pharyngitis is much less predictable.
-
The relevant literature does not provide a clear cut-off value for repeated episodes of tonsillitis to indicate surgery. However, TE was not suggested in patients with less than three tonsillitis episodes in their history.
-
Regarding the different studies, the diagnosis and quality of documentation of acute tonsillitis episodes and the definition of such episodes required to diagnose “acute tonsillitis” is very heterogeneous.
-
Because of the spontaneous healing rate, surgery may not be indicated any more within an observation time of 6 months.
-
TE was not indicated in patients without previous and repeated antibiotic therapy.
Children
-
TE may certainly reduce the number of severe recurrent acute tonsillitis episodes within the first postoperative year.
-
An unpredictable risk of pharyngitis remains after TE.
-
The current data do not allow statements on the treatment effect of TE for more than 1 year after surgery because too many patients were lost to follow-up and too many patients from the control group underwent TE upon request.
-
The benefit is related to the severity of symptoms, however, there is only one study that deals with severely affected children [34].
-
The moderate effect of TE can partly be explained by the additional episode of sore throat that inevitably is associated with the TE procedure.
-
The impact of adenoidectomy on the incidence and severity of symptoms cannot be assessed, based on the available data.
Adults
-
The efficacy of TE in comparison to conservative therapy of recurrent tonsillitis is low; statements hereupon are limited to the first 5–6 months after TE.
-
TE may be beneficial in patients with pharyngitis, with or without a proven group A beta-hemolytic streptococci (GABHS)-infection.
-
TE has the potential to reduce absences at work due to tonsillitis, with or without pharyngitis.
-
The data quality of both studies is very heterogeneous, pain intensity was specified and pain related to the surgical procedure was not included in the calculation of the number of episodes and absences at work.
-
The data quality of both RCT is insufficient to draw conclusions for recommendations.
-
Further research is needed to clarify, whether or not adults benefit from TE and which criteria should be applied for this purpose. The efficacy will be based on sophisticated selection criteria to identify patients in which the presence of tonsils is responsible for the disease of “sore throat”.
Conclusion: indications of tonsillectomy
Statement on the indication of tonsillectomy
The quality of evidence for tonsillectomy is moderate for children and low for adults. Conclusions concerning the efficacy of tonsillectomy on the number of sore throat episodes per year are limited to 12 postoperative months in children and 5–6 months in adults. The impact of tonsillectomy on the number of sore throat e pisodes per year in children is modest. Due to the heterogeneity of data, no firm conclusions on the effectiveness of tonsillectomy in adults can be drawn |
There is still an urgent need of further research to reliably estimate the value of tonsillectomy compared to non-surgical therapy of tonsillitis/tonsillo-pharyngitis |
The impact of tonsillectomy on the quality of life is considered as being rather positive. But also in this field there is an urgent need for further research to assess the impact of surgical therapy with appropriate inventories and standardized evaluation procedures, especially in children |
The strictness of the indication must be sufficiently assured and does not depend on a certain age of life |
Recommendation of indication of tonsillectomy
Preconditions | |
|---|---|
Decision based on | Number of episodes within the last 12 months |
<3 episodes | Tonsillectomy is no option |
3–5 episodes | Tonsillectomy is a possible option if further episodes occur within the next 6 months and a number of 6 is achieved |
≥6 episodesa | Tonsillectomy is an option of therapy |
Tonsillotomy
The content of this chapter was widely based on a recent review [75].
Classification of the size of the tonsils
The grading system of Brodsky is suggested to assess the volume of the tonsil in relation to the diameter of the pharynx [76].
Brodsky degree | Constriction of the oropharyngeal diameter (%) |
|---|---|
0 | 0 |
1 | <25 |
2 | <50 |
3 | <75 |
4 | >75 |
Classification of the surgical procedures
To reduce the volume of the tonsils, different methods exist that are all characterized by removing only part of the palatine tonsils and to preserve the capsule. Since extracapsular vessels and neural endings are not exposed or injured, postoperative morbidity is less severe compared to TE. The surgical techniques have been classified in the past [77].
Class I: tonsillotomy (TT)
Intratonsillar transection is performed medially to the palatine arches and preserves the tonsillar part located laterally. Since the anterior and posterior palatine arch serve as anatomical landmarks for the transaction line, this technique can be standardized. Different surgical instruments such as LASER, radiofrequency device, surgical scissors, and monopolar needles are applied.
Class II: subtotal/intracapsular/partial tonsillectomy (SIPT)
A piecemeal resection of the tonsillar tissue with a microdebrider from medial to lateral is performed, aiming to reduce 90 % of the tonsil and to spare the capsule. Resection is based according to the surgeon´s decision instead of anatomical landmarks and standardization therefore not possible.
Radiofrequency-induced thermal therapy (RFITT) and tonsillar ablation (TA)
This method consists of applying alternating current of radiofrequency dimension (Megahertz) to the tonsillar tissue directly via electrode contact which induces thermal necrosis that does not include neither the deep tonsillar tissue nor the capsule. Because of secondary shrinking of the tissue, the created lesions in the area of the tonsils lead to a volume reduction of the tonsil. Alternatively, the tonsillar tissue may be removed superficially without injuring the capsule either by LASER or a bipolar Coblation probe based on the coagulation effect.
Review of the literature
Windfuhr et al. [75] analyzed 86 case series with a total of 10,499 patients in study groups and 10,448 patients in control groups. Based on data where the surgical method was mentioned, class I procedures were performed 36 times, class I procedures 37 times, and ablative procedures were applied 13 times. The most frequently used instrument was the microdebrider. A superiority of certain surgical instruments could not be proven. The partial resection of the tonsils was clearly superior to complete TE in relation to the duration of surgery, intraoperative bleeding, return to normal diet, and pain. Postoperative hemorrhage requiring revision surgery occurred in 0.26 % of the cases (0–2.5 %), dehydration and upper airway obstruction were reported for single cases [78–82]. Lethal outcome did not occur in any of the studies but has been reported in the literature [83]. Although TT was most commonly indicated to resolve upper airway obstruction resulting from (adeno)tonsillar hypertrophy, several authors indicated TT also in patients with an exclusive history of tonsillitis (Table 3).
Tonsillar regrowth was reported for 3.05 % of all patients after TT (median; range 0–26.9 %) and the rate of recurrent tonsillitis ranged from 0 to 16.32 % (median: 3.9 %). A secondary TE resulted in 1.54 % after TT (median; range 0–11.9 %) due to tonsillar regrowth or postoperative tonsillitis.
Unfortunately, data concerning operation time, intraoperative bleeding, return to normal diet, postoperative dehydration, intake of analgesics, postoperative tonsillitis, tonsillar regrowth, and secondary TE were not provided in 50–66 % of the case series which impedes a meta-analysis. Moreover, the follow-up varied for class I TT between ≤1 week [84], ≤2 weeks [85–88], 3 weeks [89], 1 month [90], 6 months [91], 12 months [69, 92–96], 18 months [97], 24 months [98–100], 32 months [101], 35 months [102], 36 months [103], 48 months [104–106], 72 months [107–109], 78 months [110, 111], 108 months [112], 132 [113], and 168 months [114]. Class II SIPT were followed for ≤1 week [115–120], ≤2 weeks [121–128], 1 month [129], “more than 4 weeks” [130], 6 weeks [131], 10 weeks [132], 3 months [133], 6 months [134], 7.6 months [135], 12 months [136–141], 18 months [142, 143], 24 months [144], 30 months [145], for a median of 32 months [146], 36.2 months [147], 72 months [148, 149], 77.4 months [150]. Patients having undergone TA, were followed-up for 3 [79, 133], 6 [82, 151], 12 [80, 152], 24 [153, 154], 36 [78, 81, 155], and 48 months [156]. Four studies do not mention a follow-up [157–160] and in 3 other studies, the surgical instruments were not specified [161–163].
Summary
-
In comparison to TE, methods to reduce the volume of the palatine tonsils are less frequently performed.
-
Different surgical instruments are useful to downsize the volume of the palatine tonsils; the superiority of a single procedure cannot be proven by the contemporary studies.
-
Up to now, TT or comparable procedures are not mentioned in national guidelines worldwide as a surgical alternative to treat recurrent tonsillitis or sleep-related breathing disorders resulting from tonsillar hyperplasia.
-
Evidence is given from several studies, that TT or comparable procedures are capable to resolve upper airway obstruction as well as recurrent episode of acute tonsillitis.
-
Tonsillitis in the history is no contraindication for TT.
-
Studies proving that a certain frequency of tonsillitis episodes justifies TE instead of TT do not exist.
-
Indication for TT or comparable procedures is not limited by age.
-
Data concerning operation time, intraoperative blood loss, return to normal diet, intake of analgesics and postoperative complications clearly favor TT or comparable procedures.
-
Tonsillar regrowth or tonsillitis following TT or comparable procedures is rare and occurs most commonly within the first postoperative year.
Conclusion: indication of tonsillotomy in cases of tonsillitis
Statement on the indication of tonsillotomy
In contrast to tonsillectomy, tonsillotomy or comparable procedures are characterized by a substantially lower postoperative morbidity (pain and bleeding) |
Although tonsillar tissue is left behind, a reduction of the sore throat episode per year is observed in young adults that does not differ from the reduction rate after tonsillectomy |
Abscesses in the remaining tonsillar tissue are not typical |
A limitation of the surgical method to a certain age cannot be justified scientifically |
An episodes of acute tonsillitis in the patient’s history cannot be interpreted as contraindication of tonsillotomy |
To perform reduction of the tonsils, no special surgical instruments are required, the superiority of single measures cannot be proven |
Indication for tonsillotomy or comparable procedures
Preconditions | |
|---|---|
Decision based on | Size of the tonsils >Brodsky grade 1, and number of episodes during the previous 12 months |
<3 episodes | Tonsillotomy is no option |
3–5 episodes | Tonsillotomy is a possible option, if further episodes occur within the next 6 months and a number of 6 is achieved |
≥6 episodesa | Tonsillotomy is an option of therapy |
Chapter II: peritonsillar abscess (PTA)
Management of peritonsillar abscess—recommendations
Needle aspiration, incision and drainage, and abscess tonsillectomy (tonsillectomy à chaud) are effective methods of therapy |
Compliance and ability of the patient to cooperate must be taken into account when choosing the surgical method |
Simultaneously, antibiotic therapy should be applied |
Abscess tonsillectomy should be preferred, if complications have occurred or if alternative therapeutic procedures have failed. Simultaneous tonsillectomy of the contralateral side should only be performed if criteria for elective tonsillectomy are matched or evidence of a bilateral peritonsillar abscess |
Needle aspiration or incision and drainage should be preferred, if co-morbidities exist or an increased surgical risk or coagulation disorders are present. Recurrences of peritonsillar abscesses after needle aspiration or incision and drainage are rare |
Interval tonsillectomy should not be performed, the approach offers no advantage |
The Medline [30] review with filters “language” (German and English), “review”, “publication dates” (1964–2014) and “peritonsillar abscess” identified 73 articles. After analysis of the abstracts, 14 articles left over for evaluation the complete papers. A second Medline review with filters “language” (German and English) “publication date” (2009–2014) and “peritonsillar abscess” resulted in 110 matching publications. After analyzing the abstracts, 9 publications remained for evaluation of the complete articles. In the same way, a third Medline review was performed with filters “language” (German and English), publication date (2004–2014) and “peritonsillar abscess bilateral” which resulted in 25 matching articles. Case reports were excluded and after analysis of the abstracts, four papers remained for evaluation. Furthermore, articles were evaluated that had been mentioned in the secondary literature (as of August 2014).
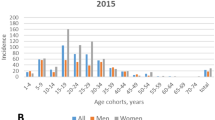
In the literature, PTA is considered as being the most frequent complication of acute tonsillitis. However, a major argument against this statement is that the age peak of PTA is found in young adults while the incidence peak of acute bacterial tonsillitis is in children and adolescence of school age. An alternative hypothesis suggests abscess formation in Weber´s glands at the upper tonsillar pole [168]. With regard to microbiology, often an aerobic-anaerobic mixed infection is found. The aerobic pathogen in this context is mostly Streptococcus pyogenes, typical anaerobes are Fusobacterium necrophorum, peptostreptococci, and Prevotella spp. Smoking, poor oral hygiene and male gender have been identified as risk factors for the development of peritonsillar abscess [169]. Spreading into the retropharyngeal space does not change the diagnosis of PTA. In contrast, a true retropharyngeal abscess derives from the retropharyngeal space. This is a different and rare entity and not within the scope of this guideline.
Options of surgical therapy
-
Needle aspiration (NA): aspiration of pus via a syringe needle, once or repeatedly.
-
Incision and drainage (ID): surgical opening of the abscess and intraoral draining.
-
Tonsillectomy in the interval (ITE): TE after the end of acute therapy with antibiotics and ID or NP, most commonly as bilateral TE.
-
Tonsillectomy à chaud (TAC): abscess tonsillectomy in the acute stage of the disease, either exclusively of the affected side or with simultaneous contralateral TE.
Johnson and Stewart performed a systematic review of the literature published between 2002 and 2004 on the management of PTA. He stated that the effectiveness of NA, ID and TAC was proven by several studies. The procedures were not compared in controlled studies, therefore is no recommendation for a single technique is obtainable. Because NA or ID most commonly requires general anesthesia in children, TAC is suggested for this subgroup of patients [170]. His findings are widely supported by Darrow and Siemens [171] and Powell and Wilson, who recommended further studies in studies with larger sample sizes [172]. According to the review of Federspil, TAC should be accompanied by simultaneous TE on the opposite side only in patients with a history of recurrent episodes of tonsillitis or failure of previous surgical PTA therapy. NA or ID are assessed as valuable procedures with a failure rate ranging between 9 and 20 % [173]. TAC proved to be effective and safe in the study of Page et al. [174]. Without explicit citations of studies, Gysin recommended TAC especially in children because of the higher recurrence rate in this age subgroup [175].
Herzon reported a failure rate of only 5 % in his patient population (n = 123) mandating a second NA. According to his survey, ID was suggested by 54 % of the American otolaryngologists, NA by only 32 %, and TAC only by a minority of 14 %. His literature review revealed a success rate of NA in 94 % of 496 cases from 10 studies and a recurrence rate of 10 % in 884 PTA patients (USA) and 15 % in 1399 PTA cases (outside USA) after NA [176].
His findings are widely supported by Johnson et al. [177], who determined a recurrence rate of 10–15 % after primary NA. While Khan et al. [178] treated 60 PTA successfully with ID, Baldassari and Shah recommended NA even for pediatric patients, if they were cooperative. If general anesthesia is indicated, ID or TAC should be preferred in cases with a history of recurrent tonsillitis or upper airway obstruction [179].
Recurrence rate of PTA after NA or ID
A recurrence rate of 10–15 % after treatment with NA or ID was reported in the literature [176] which compares to rates ranging between 10 % and 22 % [172]. It should be noted, that the rates were calculated from data of older studies. It appears that the relevant literature is not able to provide sufficient information for success rates in the long term of the different modalities.
Bleeding complication after abscess tonsillectomy
It has been repeatedly reported, that bleeding following TAC do not differ from those after elective TE [180–183]. Giger registered a bleeding rate of 13 % after 206 TAC, requiring revision surgery to achieve hemostasis in 6 %. Interestingly, bleeding derived significantly more often from the contralateral side of the PTA [184].
Bilateral abscesses
In cases of a bilateral PTA the characteristic asymmetry of the soft palate may be invisible. An unexpected contralateral PTA can be found, if TAC is routinely accompanied by a contralateral TE which has been identified in 3.88 % of 541 patients [181]. While Segal registered a bilateral PTA in one patient out of 126 children (0.8 %) [185], Giger reported a rate of 5 % in 206 patients [184], Baker 5.4 % in 148 patients [186], Albertz 7.1 % in 112 patients [187], and Watanabe 6.5 % in 371 children [188]. The clinical relevance of bilateral abscesses is not evident from the literature. Interestingly, bilateral abscesses were extremely uncommon in studies with NA or ID.
Antibiotic treatment
The simultaneous therapy with antibiotics is mentioned in all evaluated publications. Different antibiotics were recommended, most commonly based on the recommendations of clinicians. RCTs on the necessity of antibiotic therapy do not exist. According to more recent studies [173, 189], GABHS are involved in about half of the PTA cases and a mixed spectrum a typical finding, including anaerobes. A more detailed information is not obtainable from different national guidelines [190–192]. The necessity of antibiotic treatment as a routine in PTA patients is debatable. Currently, a German guideline concerning antibiotic treatment of infections in the head and neck region is under review.
Chapter III: infectious mononucleosis
Recommendations
Tonsillectomy as a routine procedure for symptom control or reduction of the course of the disease should not be performed |
Tonsillectomy is indicated in cases with clinically significant upper airway obstruction resulting from inflammatory tonsillar hyperplasia |
If signs of a concomitant bacterial infection are not present, antibiotics should not be applied |
Steroids may be administered for symptom relief |
Historically, it has been repeatedly stated that TE is capable to shorten the clinical course in patients suffering from infectious mononucleosis (IM) involving the palatine tonsils. The concept dates back to the 1930ies to 1970ies. Case reports, retrospective studies, and comments described a significantly improved clinical course following TE with an earlier recovery without an increased complication rate [193, 194]. The studies were not randomized nor did they include a control group.
A Medline review was performed for this clinical guideline with filters like “language” (German and English) and keyword “mononucleosis” and “tonsil” (87 hits)/“tonsillectomy” (65 hits). After checking the abstracts on the topic of “tonsillectomy as therapy for mononucleosis”, 16 articles were eligible for this guideline, including 12 papers that were published between 1964 and 1984. Since 1984, only few articles were published on the topic [9, 195–200]. The Cochrane Collaboration published a review article on the therapy of mononucleosis with corticosteroids. The recommendation is given that corticosteroids should be applied for symptom control and reduction of the course of the disease. TE, however, as an option of therapy is not mentioned [201]. Supportive antibiotic therapy is regularly administered in patients presenting with IM, but there are no RCTs or other clinical studies to support this regimen [169].
Summary
References
Randall DA, Hoffer ME (1998) Complications of tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg 118:61–68
Carmody D, Vamadevan T, Cooper SM (1982) Post tonsillectomy haemorrhage. J Laryngol Otol 96:635–638
Windfuhr J, Seehafer M (2001) Classification of haemorrhage following tonsillectomy. J Laryngol Otol 115:457–461
Kang J, Brodsky L, Danziger I, Volk M, Stanievich J (1994) Coagulation profile as a predictor for post-tonsillectomy and adenoidectomy (T + A) hemorrhage. Int J Pediatr Otorhinolaryngol 28:157–165
Handler SD, Miller L, Richmond KH, Baranak CC (1986) Post-tonsillectomy hemorrhage: incidence, prevention and management. Laryngoscope 96:1243–1247
Watson M, Dawes P, Samuel P et al (1993) A study of haemostasis following tonsillectomy comparing ligatures with diathermy. J Laryngol Otol 107:711–715
Sarny S, Ossimitz G, Habermann W, Stammberger H (2012) „Die Österreichische Tonsillenstudie 2010“—Teil 1: Statistischer Überblick. Laryngo- rhino- otologie 91:16–21
Georgalas CC, Tolley NS, Narula A (2009) Tonsillitis. Clin Evid 2009:1–12
Lowe D, van der Meulen J (2004) Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet 364:697–702
Windfuhr JP, Wienke A, Chen YS (2009) Electrosurgery as a risk factor for secondary post-tonsillectomy hemorrhage. Eur Arch Otorhinolaryngol 266:111–116
Sarny S, Ossimitz G, Habermann W, Stammberger H (2011) Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope 121:2553–2560
Neumann C, Street I, Lowe D, Sudhoff H (2007) Harmonic scalpel tonsillectomy: a systematic review of evidence for postoperative hemorrhage. Otolaryngol Head Neck Surg 137:378–384
Pinder D, Hilton M (2001) Dissection versus diathermy for tonsillectomy. Cochrane Database Syst Rev 2001(4):CD002211
Pinder DK, Wilson H, Hilton MP (2011) Dissection versus diathermy for tonsillectomy. Cochrane Database Syst Rev 2011(3):CD002211
Dhiwakar M, Clement WA, Supriya M, McKerrow W (2012) Antibiotics to reduce post-tonsillectomy morbidity. Cochrane Database Syst Rev 12:CD005607
Cardozo AA, Hallikeri C, Lawrence H, Sankar V, Hargreaves S (2007) Teenage and adult tonsillectomy: dose–response relationship between diathermy energy used and morbidity. Clin Otolaryngol 32:366–371
Kaiser AD (1930) Results of tonsillectomy. A comparative study of twenty-two hundred tonsillectomized children with an equal number of controls three and ten years after operation. JAMA 95:837–842
Roydhouse N (1970) A controlled study of adenotonsillectomy. Arch Otolaryngol 92:611–616
Mawson SR, Adlington P, Evans M (1967) A controlled study evaluation of adeno-tonsillectomy in children. J Laryngol Otol 81:777–790
Mawson SR, Adlington P, Evans M (1968) A controlled study evaluation of adeno-tonsillectomy in children. J Laryngol Otol 82:963–979
McKee WJ (1963) A controlled study of the effects of tonsillectomy and adenoidectomy in children. Br J Prev Soc Med 17:133–140
Marshall T (1998) A review of tonsillectomy for recurrent throat infection. Br J Gen Pract 48:1331–1335
van Staaij BK, van den Akker EH, van der Heijden GJ, Schilder AG, Hoes AW (2005) Adenotonsillectomy for upper respiratory infections: evidence based? Arch Dis Child 90:19–25
Clayburgh D, Milczuk H, Gorsek S, Sinden N, Bowman K, Macarthur C (2011) Efficacy of tonsillectomy for pediatric patients with Dysphagia and tonsillar hypertrophy. Arch Otolaryngol Head Neck Surg 137:1197–1202
Naiboglu B, Kulekci S, Kalaycik C, Sheidaei S, Toros SZ, Egeli E (2010) Improvement in quality of life by adenotonsillectomy in children with adenotonsillar disease. Clin Otolaryngol 35:383–389
Stalfors J, Ericsson E, Hemlin C et al (2012) Tonsil surgery efficiently relieves symptoms: analysis of 54 696 patients in the National Tonsil Surgery Register in Sweden. Acta Otolaryngol 132:533–539
Burton MJ, Glasziou PP (2009) Tonsillectomy or adeno-tonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev 2009(1):CD001802
Barraclough J, Anari S (2014) Tonsillectomy for recurrent sore throats in children: indications, outcomes, and efficacy. Otolaryngol Head Neck Surg 150:722–729
McKee WJ (1963) The part played by adenoidectomy in the combined operation of tonsillectomy with adenoidectomy. Second part of a controlled study in children. Br J Prev Soc Med 17:133–140
Roydhouse N (1969) A controlled study of adenotonsillectomy. Lancet 2:931–932
Paradise JL, Bluestone CD, Bachman RZ et al (1984) Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials. N Engl J Med 310:674–683
Paradise J, Bluestone C, Colborn D, Bernard B, Rockette H, Kurs-Lasky M (2002) Tonsillectomy and adenotonsillectomy for recurrent throat infection in moderately affected children. Pediatrics 110:7–15
van Staaij BK, van den Akker EH, Rovers MM, Hordijk GJ, Hoes AW, Schilder AG (2004) Effectiveness of adenotonsillectomy in children with mild symptoms of throat infections or adenotonsillar hypertrophy: open, randomised controlled trial. BMJ 329:651
Lock C, Wilson J, Steen N et al (2010) North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study. Health Technol Assess 14:1–164, iii–iv
Buskens E, van Staaij B, van den Akker J, Hoes AW, Schilder AG (2007) Adenotonsillectomy or watchful waiting in patients with mild to moderate symptoms of throat infections or adenotonsillar hypertrophy: a randomized comparison of costs and effects. Arch Otolaryngol Head Neck Surg 133:1083–1088
Wilson JA, Steen IN, Lock CA et al (2012) Tonsillectomy: a cost-effective option for childhood sore throat? Further analysis of a randomized controlled trial. Otolaryngol Head Neck Surg 146:122–128
Goldstein NA, Fatima M, Campbell TF, Rosenfeld RM (2002) Child behavior and quality of life before and after tonsillectomy and adenoidectomy. Arch Otolaryngol Head Neck Surg 128:770–775
Goldstein NA, Stewart MG, Witsell DL et al (2008) Quality of life after tonsillectomy in children with recurrent tonsillitis. Otolaryngol Head Neck Surg 138:S9–S16
Hopkins C, Fairley J, Yung M, Hore I, Balasubramaniam S, Haggard M (2010) The 14-item Paediatric Throat Disorders Outcome Test: a valid, sensitive, reliable, parent-reported outcome measure for paediatric throat disorders. J Laryngol Otol 124:306–314
Kubba H, Swan IR, Gatehouse S (2004) The Glasgow Children’s Benefit Inventory: a new instrument for assessing health-related benefit after an intervention. Ann Otol Rhinol Laryngol 113:980–986
Schwentner I, Schmutzhard J, Schwentner C, Abraham I, Hofer S, Sprinzl GM (2008) The impact of adenotonsillectomy on children’s quality of life. Clin Otolaryngol 33:56–59
Camilleri A, MacKenzie K, Gatehouse S (1995) The effect of recurrent tonsillitis and tonsillectomy on growth in childhood. Clin Otolaryngol 20:153–157
Papakostas K, Moraitis D, Lancaster J, McCormick MS (2003) Depressive symptoms in children after tonsillectomy. Int J Pediatr Otorhinolaryngol 67:127–132
Afolabi OA, Alabi BS, Ologe FE, Dunmade AD, Segun-Busari S (2009) Parental satisfaction with post-adenotonsillectomy in the developing world. Int J Pediatr Otorhinolaryngol 73:1516–1519
Akgun K, Aktas I, Uluc K (2008) Conservative treatment for late-diagnosed spinal accessory nerve injury. Am J Phys Med Rehabil 87:1015–1021
Conlon B, Donnelly M, McShane D (1997) Improvements in health and behaviour following childhood tonsillectomy: a parental perspective at 1 year. Int J Pediatr Otorhinolaryngol 41:155–161
Faulconbridge R, Fowler S, Horrocks J, Topham J (2000) Comparative audit of tonsillectomy. Clin Otolaryngol 25:110–117
Fox R, Temple M, Owens D, Short A, Tomkinson A (2008) Does tonsillectomy lead to improved outcomes over and above the effect of time? A longitudinal study. J Laryngol Otol 122:1197–1200
Fujihara K, Koltai PJ, Hayashi M, Tamura S, Yamanaka N (2006) Cost-effectiveness of tonsillectomy for recurrent acute tonsillitis. Ann Otol Rhinol Laryngol 115:365–369
Nikakhlagh S, Rahim F, Boostani H, Shirazi ST, Saki N (2012) The effect of adenotonsillectomy on quality of life in adults and pediatric patients. Indian J Otolaryngol Head Neck Surg 64:181–183
Robb PJ, Gowrinath K, Agyeman K, Joseph J (2009) Paediatric tonsillectomy: parental experience and outcomes. J Laryngol Otol 123:103–107
Wolfensberger M, Haury JA, Linder T (2000) Parent satisfaction 1 year after adenotonsillectomy of their children. Int J Pediatr Otorhinolaryngol 56:199–205
Akgun D, Seymour FK, Qayyum A, Crystal R, Frosh A (2009) Assessment of clinical improvement and quality of life before and after tonsillectomy. J Laryngol Otol 123(2):199–202
Robb PJ, Gowrinath K, Agyeman K, Joseph J (2009) Paediatric tonsillectomy: parental experience and outcomes. J Laryngol Otol 123(1):103–107
Schwentner I, Schmutzhard J, Schwentner C, Abraham I, Hofer S, Sprinzl GM (2008) The impact of adenotonsillectomy on children’s quality of life. Clin Otolaryngol 33(1):56–59
Goldstein NA, Stewart MG, Witsell DL et al (2008) Quality of life after tonsillectomy in children with recurrent tonsillitis. Otolaryngol Head Neck Surg 138(Suppl 1):S9–S16
Blakley BW, Magit AE (2009) The role of tonsillectomy in reducing recurrent pharyngitis: a systematic review. Otolaryngol Head Neck Surg 140:291–297
Alho OP, Koivunen P, Penna T, Teppo H, Koskela M, Luotonen J (2007) Tonsillectomy versus watchful waiting in recurrent streptococcal pharyngitis in adults: randomised controlled trial. Clin Otolaryngol 32:285
Andreou N, Hadjisymeou S, Panesar J (2013) Does tonsillectomy improve quality of life in adults? A systematic literature review. J Laryngol Otol 127:332–338
Bhattacharyya N, Kepnes L (2002) Economic benefit of tonsillectomy in adults with chronic tonsillitis. Ann Otol Rhinol Laryngol 111:983–988
Baumann I, Kucheida H, Blumenstock G, Zalaman IM, Maassen MM, Plinkert PK (2006) Benefit from tonsillectomy in adult patients with chronic tonsillitis. Eur Arch Otorhinolaryngol 263:556–559
Schwentner I, Hofer S, Schmutzhard J, Deibl M, Sprinzl GM (2007) Impact of tonsillectomy on quality of life in adults with chronic tonsillitis. Swiss Med Wkly 137:454–461
Richards AL, Bailey M, Hooper R, Thomson P (2007) Quality-of-life effect of tonsillectomy in a young adult group. ANZ J Surg 77:988–990
Koskenkorva T, Koivunen P, Penna T, Teppo H, Alho OP (2009) Factors affecting quality-of-life impact of adult tonsillectomy. J Laryngol Otol 123(9):1010–1014
Senska G, Ellermann S, Ernst S, Lax H, Dost P (2010) Rezidivierende Tonsillitis bei Erwachsenen: Lebensqualität nach Tonsillektomie. Dtsch Arztebl Int 107:622–628
Ericsson E, Ledin T, Hultcrantz E (2007) Long-term improvement of quality of life as a result of tonsillotomy (with radiofrequency technique) and tonsillectomy in youths. Laryngoscope 117:1272–1279
Witsell DL, Orvidas LJ, Stewart MG et al (2008) Quality of life after tonsillectomy in adults with recurrent or chronic tonsillitis. Otolaryngol Head Neck Surg 138:S1–S8
Motta G, Motta S, Cassano P et al (2013) Effects of guidelines on adeno-tonsillar surgery on the clinical behaviour of otorhinolaryngologists in Italy. BMC Ear Nose Throat Disord 13:1
http://onlinelibrary.wiley.com/cochranelibrary/search. Accessed 01 June 2015
Burton MJ, Glasziou PP, Chong LY, Venekamp RP (2014) Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev 11:CD001802
Koskenkorva T, Koivunen P, Koskela M, Niemela O, Kristo A, Alho OP (2013) Short-term outcomes of tonsillectomy in adult patients with recurrent pharyngitis: a randomized controlled trial. CMAJ 185:E331–E336
Windfuhr JP, Savva K, Dahm J, Werner JA (2015) Tonsillotomy: facts and fiction. Eur Arch Otorhinolaryngol 272(4):949–969
Ng SK, Lee DL, Li AM, Wing YK, Tong MC (2010) Reproducibility of clinical grading of tonsillar size. Arch Otolaryngol Head Neck Surg 136:159–162
Windfuhr J, Werner J (2013) Tonsillotomy: it’s time to clarify the facts. Eur Arch Otorhinolaryngol 270:2985–2996
Chatziavramidis A, Constantinidis J, Gennadiou D, Derwisis D, Sidiras T (2007) Volume reduction of tonsil hyperplasia in childhood with a surgical ultrasound device. Laryngo- rhino- otologie 86:177–183
Nelson LM (2000) Radiofrequency treatment for obstructive tonsillar hypertrophy. Arch Otolaryngol Head Neck Surg 126:736–740
Nelson LM (2003) Temperature-controlled radiofrequency tonsil reduction in children. Arch Otolaryngol Head Neck Surg 129:533–537
Palmieri B, Iannitti T, Fistetto G, Rottigni V (2013) The, “Swiss-cheese Doppler-guided laser tonsillectomy”: a new safe cribriform approach to intracapsular tonsillectomy. Lasers Med Sci 28:865–869
Pfaar O, Spielhaupter M, Schirkowski A et al (2007) Treatment of hypertrophic palatine tonsils using bipolar radiofrequency-induced thermotherapy (RFITT). Acta Otol 127(11):1176–1181
Windfuhr JP (2013) Faults and failure of tonsil surgery and other standard procedures in otorhinolaryngology. Laryngo- rhino- otologie 92(Suppl 1):S33–S72
Stelter K, de la Chaux R, Patscheider M, Olzowy B (2010) Double-blind, randomised, controlled study of post-operative pain in children undergoing radiofrequency tonsillotomy versus laser tonsillotomy. J Laryngol Otol 127(1):1176–1181
Hultcrantz E, Ericsson E (2004) Pediatric tonsillotomy with the radiofrequency technique: less morbidity and pain. Laryngoscope 114:871–877
Linder A, Markstrom A, Hultcrantz E (1999) Using the carbon dioxide laser for tonsillotomy in children. Int J Pediatr Otorhinolaryngol 50:31–36
Ericsson E, Wadsby M, Hultcrantz E (2006) Pre-surgical child behavior ratings and pain management after two different techniques of tonsil surgery. Int J Pediatr Otorhinolaryngol 70:1749–1758
Huber K, Sadick H, Maurer JT, Hörmann K, Hammerschmitt N (2005) Tonsillotomy with the argon-supported monopolar needle—first clinical results. Laryngo- rhino- otologie 84:671–675
Havel M, Sroka R, Englert E, Stelter K, Leunig A, Betz CS (2012) Intraindividual comparison of 1,470 nm diode laser versus carbon dioxide laser for tonsillotomy: a prospective, randomized, double blind, controlled feasibility trial. Lasers Surg Med 44:558–563
Moriniere S, Roux A, Bakhos D et al (2013) Radiofrequency tonsillotomy versus bipolar scissors tonsillectomy for the treatment of OSAS in children: a prospective study. Eur Ann Otorhinolaryngol Head Neck Dis 130:67–72
Ericsson E, Lundeborg I, Hultcrantz E (2009) Child behavior and quality of life before and after tonsillotomy versus tonsillectomy. Int J Pediatr Otorhinolaryngol 73:1254–1262
Hultcrantz E, Linder A, Markstrom A (1999) Tonsillectomy or tonsillotomy? A randomized study comparing postoperative pain and long-term effects. Int J Pediatr Otorhinolaryngol 51:171–176
de la Chaux R, Klemens C, Patscheider M, Reichel O, Dreher A (2008) Tonsillotomy in the treatment of obstructive sleep apnea syndrome in children: polysomnographic results. Int J Pediatr Otorhinolaryngol 72:1411–1417
Baharudin A, Shahid H, Rhendra MZ (2006) Laser tonsillotomy in children with tonsillar hyperplasia. Med J Malays 61:377–379
Ericsson E, Hultcrantz E (2007) Tonsil surgery in youths: good results with a less invasive method. Laryngoscope 117:654–661
Stelter K, Ihrler S, Siedek V, Patscheider M, Braun T, Ledderose G (2012) 1-Year follow-up after radiofrequency tonsillotomy and laser tonsillotomy in children: a prospective, double-blind, clinical study. Eur Arch Otorhinolaryngol 269:679–684
Vlastos IM, Parpounas K, Economides J, Helmis G, Koudoumnakis E, Houlakis M (2008) Tonsillectomy versus tonsillotomy performed with scissors in children with tonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 72:857–863
Densert O, Desai H, Eliasson A et al (2001) Tonsillotomy in children with tonsillar hypertrophy. Acta Otolaryngol 121:854–858
Reichel O, Mayr D, Winterhoff J, de la Chaux R, Hagedorn H, Berghaus A (2007) Tonsillotomy or tonsillectomy? A prospective study comparing histological and immunological findings in recurrent tonsillitis and tonsillar hyperplasia. Eur Arch Otorhinolaryngol 264:277–284
Korkmaz O, Bektas D, Cobanoglu B, Caylan R (2008) Partial tonsillectomy with scalpel in children with obstructive tonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 72(7):1007–1012
Celenk F, Bayazit YA, Yilmaz M et al (2008) Tonsillar regrowth following partial tonsillectomy with radiofrequency. Int J Pediatr Otorhinolaryngol 72:19–22
Ericsson E, Graf J, Hultcrantz E (2006) Pediatric tonsillotomy with radiofrequency technique: long-term follow-up. Laryngoscope 72(7):1851–1857
Sedlmaier B, Bohlmann P, Jakob O, Reinhardt A (2010) Outpatient diode laser tonsillotomy in children with tonsillar hyperplasia. Clinical results. HNO 58:244–254
Zagolski O (2010) Why do palatine tonsils grow back after partial tonsillectomy in children? Eur Arch Otorhinolaryngol 267:1613–1617
Hanenkamp U, Helling K, Mann WJ (2008) Die Tonsillotomie mit der bipolaren Koagulationsschere. Laryngo- rhino- otologie 87:870–873
Ilgen F (2005) Laser-assisted tonsillotomy in children with obstructive sleep apnea and adenotonsillary hyperplasia—experiences as an outpatient procedure. Laryngo- rhino- otologie 84:665–670
Hultcrantz E, Linder A, Markstrom A (2005) Long-term effects of intracapsular partial tonsillectomy (tonsillotomy) compared with full tonsillectomy. Int J Pediatr Otorhinolaryngol 69:463–469
Scherer H (2003) Tonsillotomie versus Tonsillektomie. Laryngo- rhino- otologie 82:754–755
Wireklint S, Ericsson E (2012) Health-related quality of life after tonsillotomy versus tonsillectomy in young adults: 6 years postsurgery follow-up. Eur Arch Otorhinolaryngol 269:1951–1958
Eisfeld W, Amler S, Deitmer T (2010) Long-term results following tonsillotomy in children. Laryngo- rhino- otologie 89:466–472
Helling K, Abrams J, Bertram WK, Hohner S, Scherer H (2002) Die Lasertonsillotomie bei der Tonsillenhyperplasie des Kleinkindes. HNO 50:470–478
Unkel C, Lehnerdt G, Metz K, Jahnke K, Dost P (2004) Langzeitverlauf nach Laser-Tonsillotomie bei symptomatischer Tonsillenhyperplasie. Laryngo- rhino- otologie 83:466–469
Unkel C, Lehnerdt G, Schmitz KJ, Jahnke K (2005) Laser-tonsillotomy for treatment of obstructive tonsillar hyperplasia in early childhood: a retrospective review. Int J Pediatr Otorhinolaryngol 69:1615–1620
Eviatar E, Kessler A, Shlamkovitch N, Vaiman M, Zilber D, Gavriel H (2009) Tonsillectomy vs. partial tonsillectomy for OSAS in children—10 years post-surgery follow-up. Int J Pediatr Otorhinolaryngol 73:637–640
Chang KW (2005) Randomized controlled trial of coblation versus electrocautery tonsillectomy. Otolaryngol Head Neck Surg 132:273–280
Nguyen CV, Parikh SR, Bent JP (2009) Comparison of intraoperative bleeding between microdebrider intracapsular tonsillectomy and electrocautery tonsillectomy. Ann Otol Rhinol Laryngol 118:698–702
Park A, Proctor MD, Alder S, Muntz H (2007) Subtotal bipolar tonsillectomy does not decrease postoperative pain compared to total monopolar tonsillectomy. Int J Pediatr Otorhinolaryngol 71:1205–1210
Pruegsanusak K, Wongsuwan K, Wongkittithawon J (2010) A randomized controlled trial for perioperative morbidity in microdebrider versus cold instrument dissection tonsillectomy. J Med Assoc Thail 93:558–565
Chang KW (2008) Intracapsular versus subcapsular coblation tonsillectomy. Otolaryngol Head Neck Surg 138:153–157
Arya AK, Donne A, Nigam A (2005) Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain in children. Clin Otolaryngol 30:226–229
Sobol SE, Wetmore RF, Marsh RR, Stow J, Jacobs IN (2006) Postoperative recovery after microdebrider intracapsular or monopolar electrocautery tonsillectomy: a prospective, randomized, single-blinded study. Arch Otolaryngol Head Neck Surg 132:270–274
Wilson YL, Merer DM, Moscatello AL (2009) Comparison of three common tonsillectomy techniques: a prospective randomized, double-blinded clinical study. Laryngoscope 119:162–170
Gan K, Tomlinson C, El-Hakim H (2009) Post-operative bleeding is less after partial intracapsular tonsillectomy than bipolar total procedure. Int J Pediatr Otorhinolaryngol 73:667–670
Lister MT, Cunningham MJ, Benjamin B et al (2006) Microdebrider tonsillotomy vs electrosurgical tonsillectomy: a randomized, double-blind, paired control study of postoperative pain. Arch Otolaryngol Head Neck Surg 132:599–604
Cohen MS, Getz AE, Isaacson G, Gaughan J, Szeremeta W (2007) Intracapsular vs. extracapsular tonsillectomy: a comparison of pain. Laryngoscope 117:1855–1858
Hall DJ, Littlefield PD, Birkmire-Peters DP, Holtel MR (2004) Radiofrequency ablation versus electrocautery in tonsillectomy. Otolaryngol Head Neck Surg 130:300–305
Koltai PJ, Solares CA, Mascha EJ, Xu M (2002) Intracapsular partial tonsillectomy for tonsillar hypertrophy in children. Laryngoscope 112:17–19
Littlefield PD, Hall DJ, Holtel MR (2005) Radiofrequency excision versus monopolar electrosurgical excision for tonsillectomy. Otolaryngol Head Neck Surg 133:51–54
Derkay CS, Darrow DH, Welch C, Sinacori JT (2006) Post-tonsillectomy morbidity and quality of life in pediatric patients with obstructive tonsils and adenoid: microdebrider vs electrocautery. Otolaryngol Head Neck Surg 134:114–120
Lee KC, Altenau MM, Barnes DR et al (2002) Incidence of complications for subtotal ionized field ablation of the tonsils. Otolaryngol Head Neck Surg 127:531–538
Rakesh S, Anand TS, Payal G, Pranjal K (2012) A prospective, randomized, double-blind study of coblation versus dissection tonsillectomy in adult patients. Indian J Otolaryngol Head Neck Surg 64:290–294
Tunkel DE, Hotchkiss KS, Carson KA, Sterni LM (2008) Efficacy of powered intracapsular tonsillectomy and adenoidectomy. Laryngoscope 118:1295–1302
Friedman M, LoSavio P, Ibrahim H, Ramakrishnan V (2003) Radiofrequency tonsil reduction: safety, morbidity, and efficacy. Laryngoscope 113:882–887
Cantarella G, Viglione S, Forti S, Minetti A, Pignataro L (2012) Comparing postoperative quality of life in children after microdebrider intracapsular tonsillotomy and tonsillectomy. Auris Nasus Larynx 39:407–410
Friedman M, Wilson MN, Friedman J, Joseph NJ, Lin HC, Chang HW (2009) Intracapsular coblation tonsillectomy and adenoidectomy for the treatment of pediatric obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 140:358–362
Koltai P, Solares C, Koempel J et al (2003) Intracapsular tonsillar reduction (partial tonsillectomy): reviving a historical procedure for obstructive sleep disordered breathing in children. Otolaryngol Head Neck Surg 129:532–538
Chan KH, Friedman NR, Allen GC et al (2004) Randomized, controlled, multisite study of intracapsular tonsillectomy using low-temperature plasma excision. Arch Otolaryngol Head Neck Surg 130:1303–1307
Bent JP, April MM, Ward RF, Sorin A, Reilly B, Weiss G (2004) Ambulatory powered intracapsular tonsillectomy and adenoidectomy in children younger than 3 years. Arch Otolaryngol Head Neck Surg 130:1197–1200
Colen TY, Seidman C, Weedon J, Goldstein NA (2008) Effect of intracapsular tonsillectomy on quality of life for children with obstructive sleep-disordered breathing. Arch Otolaryngol Head Neck Surg 134:124–127
Sorin A, Bent JP, April MM, Ward RF (2004) Complications of microdebrider-assisted powered intracapsular tonsillectomy and adenoidectomy. Laryngoscope 114:297–300
Babademez M, Yurekli M, Acar B, Günbey E (2011) Comparison of radiofrequency ablation, laser and coblator techniques in reduction of tonsil size. Acta Otolaryngol 131:750–756
Schmidt R, Herzog A, Cook S, O’Reilly R, Deutsch E, Reilly J (2007) Complications of tonsillectomy: a comparison of techniques. Arch Otolaryngol Head Neck Surg 133:925–928
Schmidt R, Herzog A, Cook S, O’Reilly R, Deutsch E, Reilly J (2007) Powered intracapsular tonsillectomy in the management of recurrent tonsillitis. Otolaryngol Head Neck Surg 137:338–340
Wood JM, Harris PK, Woods CM, McLean SC, Esterman A, Carney AS (2011) Quality of life following surgery for sleep disordered breathing: subtotal reduction adenotonsillectomy versus adenotonsillectomy in Australian children. ANZ J Surg 81:340–344
Divi V, Benninger M (2005) Postoperative tonsillectomy bleed: coblation versus noncoblation. Laryngoscope 115:31–33
Johnston DR, Gaslin M, Boon M, Pribitkin E, Rosen D (2010) Postoperative complications of powered intracapsular tonsillectomy and monopolar electrocautery tonsillectomy in teens versus adults. Ann Otol Rhinol Laryngol 119:485–489
Bitar MA, Rameh C (2008) Microdebrider-assisted partial tonsillectomy: short- and long-term outcomes. Eur Arch Otorhinolaryngol 265:459–463
Mangiardi J, Graw-Panzer KD, Weedon J, Regis T, Lee H, Goldstein NA (2010) Polysomnography outcomes for partial intracapsular versus total tonsillectomy. Int J Pediatr Otorhinolaryngol 74:1361–1366
Solares CA, Koempel JA, Hirose K et al (2005) Safety and efficacy of powered intracapsular tonsillectomy in children: a multi-center retrospective case series. Int J Pediatr Otorhinolaryngol 69:21–26
Doshi HK, Rosow DE, Ward RF, April MM (2011) Age-related tonsillar regrowth in children undergoing powered intracapsular tonsillectomy. Int J Pediatr Otorhinolaryngol 75:1395–1398
Larrosa F, Dura MJ, Jeremias J, Guirao M, Alberti A, Romero E (2013) The cost associated with interstitial thermotherapy for tonsil reduction vs. standard tonsillectomy. Eur Arch Otorhinolaryngol 271(5):1271–1276
Coticchia JM, Yun RD, Nelson L, Koempel J (2006) Temperature-controlled radiofrequency treatment of tonsillar hypertrophy for reduction of upper airway obstruction in pediatric patients. Arch Otolaryngol Head Neck Surg 132:425–430
Andrews PJ, Latif A (2004) Outpatient laser tonsillar ablation under local anaesthetic. Eur Arch Otorhinolaryngol 261:551–554
Nemati S, Banan R, Kousha A (2010) Bipolar radiofrequency tonsillotomy compared with traditional cold dissection tonsillectomy in adults with recurrent tonsillitis. Otolaryngol Head Neck Surg 143:42–47
Tanyeri HM, Polat S (2011) Temperature-controlled radiofrequency tonsil ablation for the treatment of halitosis. Eur Arch Otorhinolaryngol 268:267–272
Remacle M, Keghian J, Lawson G, Jamart J (2003) Carbon-dioxide laser-assisted tonsil ablation for adults with chronic tonsillitis: a 6-month follow-up study. Eur Arch Otorhinolaryngol 260:456–459
Gallagher TQ, Wilcox L, McGuire E, Derkay CS (2010) Analyzing factors associated with major complications after adenotonsillectomy in 4776 patients: comparing three tonsillectomy techniques. Otolaryngol Head Neck Surg 142:886–892
Günzel T, Zenev E, Heinze N, Schwager K (2004) Tonsillektomienachblutungen im Zeitraum von 1985 bis 2001 und Erfahrungen bei der Anwendung der Lasertonsillotomie bei Kleinkindern. Laryngo- rhino- otologie 83:579–584
Stucken EZ, Grunstein E, Haddad J Jr et al (2013) Factors contributing to cost in partial versus total tonsillectomy. Laryngoscope 123:2868–2872
Mixson CM, Weinberger PM, Austin MB (2007) Comparison of microdebrider subcapsular tonsillectomy to harmonic scalpel and electrocautery total tonsillectomy. Am J Otolaryngol 28:13–17
Ahlstav Martensson U, Erling Hasselqvist N, Bostrom B (2012) Differences in pain and nausea in children operated on by Tonsillectomy or Tonsillotomy—a prospective follow-up study. J Adv Nurs 69(4):782–792
Sarny S, Habermann W, Ossimitz G, Schmid C, Stammberger H (2011) Tonsilar haemorrhage and re-admission: a questionnaire based study. Eur Arch Otorhinolaryngol 268:1803–1807
Smith E, Wenzel S, Rettinger G, Fischer Y (2008) Lebensqualität bei kindlichem obstruktiven Schlafapnoesyndrom nach Tonsillektomie. Tonsillotomie und/oder Adenotomie. Laryngo- rhino- otologie 87:490–497
Arya A, Donne A, Nigam A (2003) Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain. Clin Otolaryngol 28:503–506
Cohen MS, Getz AE, Isaacson G, Gaughan J, Szeremeta W (2007) Intracapsular vs. extracapsular tonsillectomy: a comparison of pain. Laryngoscope 117(10):1855–1858
Duarte V, Liu Y, Shapiro N (2014) Coblation total tonsillectomy and adenoidectomy versus coblation partial intracapsular tonsillectomy and adenoidectomy in children. Laryngoscope 124(8):1959–1964
Gan K, Tomlinson C, El-Hakim H (2009) Post-operative bleeding is less after partial intracapsular tonsillectomy than bipolar total procedure. Int J Pediatr Otorhinolaryngol 117(10):667–670
Powell E, Powell J, Samuel J, Wilson J (2013) A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation. J Antimicrob Chemother 68:1941–1950
Lehnerdt G, Senska K, Fischer M, Jahnke K (2005) Smoking promotes the formation of peritonsillar abscess. Laryngo- rhino- otologie 73(5):676–679
Johnson RF, Stewart MG (2005) The contemporary approach to diagnosis and management of peritonsillar abscess. Curr Opin Otolaryngol Head Neck Surg 13:157–160
Darrow D, Siemens C (2002) Indications for tonsillectomy and adenoidectomy. Laryngoscope 112:6–10
Powell J, Wilson JA (2012) An evidence-based review of peritonsillar abscess. Clin Otolaryngol 37:136–145
Federspil P (2009) Therapy options for peritonsillar abscess. HNO 57:223–229
Page C, Chassery G, Boute P, Obongo R, Strunski V (2010) Immediate tonsillectomy: indications for use as first-line surgical management of peritonsillar abscess (quinsy) and parapharyngeal abscess. J Laryngol Otol 124:1085–1090
Gysin C (2013) Indications of pediatric tonsillectomy. ORL 75:193–202
Herzon FS, Harris P (1995) Mosher Award thesis. Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope 105:1–17
Johnson RF, Stewart MG, Wright CC (2003) An evidence-based review of the treatment of peritonsillar abscess. Otolaryngol Head Neck Surg 128:332–343
Khan MI, Khan A (2011) Peritonsillar abscess: clinical presentation and efficacy of incision and drainage under local anaesthesia. J Ayub Med Coll: JAMC 23:34–36
Baldassari C, Shah RK (2012) Pediatric peritonsillar abscess: an overview. Infect Disord Drug Targets 12:277–280
Windfuhr JP, Remmert S (2005) Trends and complications in the management of peritonsillar abscess with emphasis on children. HNO 53:46–57
Lehnerdt G, Senska K, Fischer M, Jahnke K (2005) Bilateral peritonsillar abscesses. Eur Arch Otorhinolaryngol 262:573–575
Matschke RG, Plath P (1987) Clinical, histologic and bacteriologic findings in peritonsillar abscess. Laryngol Rhinol Otol 66:492–493
Simon LM, Matijasec JW, Perry AP, Kakade A, Walvekar RR, Kluka EA (2013) Pediatric peritonsillar abscess: Quinsy ie versus interval tonsillectomy. Int J Pediatr Otorhinolaryngol 77:1355–1358
Giger R, Landis BN, Dulguerov P (2005) Hemorrhage risk after quinsy tonsillectomy. Otolaryngol Head Neck Surg 133:729–734
Segal N, El-Saied S, Puterman M (2009) Peritonsillar abscess in children in the southern district of Israel. Int J Pediatr Otorhinolaryngol 73(8):1148–1150
Baker KA, Stuart J, Sykes KJ, Sinclair KA, Wei JL (2012) Use of computed tomography in the emergency department for the diagnosis of pediatric peritonsillar abscess. Pediatr Emerg Care 28:962–965
Albertz N, Nazar G (2012) Peritonsillar abscess: treatment with immediate tonsillectomy—10 years of experience. Acta Otol 132(10):1102–1107
Watanabe T, Suzuki M (2010) Bilateral peritonsillar abscesses: our experience and clinical features. Ann Otol Rhinol Laryngol 119:662–666
Segal N, El-Saied S, Puterman M (2009) Peritonsillar abscess in children in the southern district of Israel. Int J Pediatr Otorhinolaryngol 73(8):1148–1150
Baugh RF, Archer SM, Mitchell RB et al (2011) Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg 144:S1–S30
Lescanne E, Chiron B, Constant I et al (2012) Pediatric tonsillectomy: clinical practice guidelines. Eur Ann Otorhinolaryngol Head Neck Dis 129:264–271
www.sign.ac.uk/guidelines/fulltext/117. Accessed 1 Feb 2015
Wilke J, Swoboda R (1981) Der Einfluß der Tonsillektomie auf den Verlauf der infektiösen Mononukleose. HNO-Praxis 6:44–47
Mann W, Lange G (1974) Tonsillectomy for the acute anginous type of infectious mononucleosis. Laryngol Rhinol Otol 53:826–830
Walther LE, Ilgner J, Oehme A et al (2005) Infectious mononucleosis. HNO 53:383–392
Windfuhr J, Chen Y, Remmert S (2005) Hemorrhage Following Tonsillectomy and Adenoidectomy in 15.214 Patients. Otolaryngol Head Neck Surg 132:281–286
Wolfensberger M, Mund MT (2004) Evidence-based indications for tonsillectomy. Ther Umsch 61:325–328
Nagler J, Ruebner RL (2007) Suppurative complications and upper airway obstruction in infectious mononucleosis. J Hosp Med 2:280–282
Oddera I (2000) Infectious mononucleosis: when is tonsillectomy indicated? Schweiz Med Wochenschr Suppl 116:80S–82S
Stevenson D, Webster G, Stewart I (1992) Acute tonsillectomy in the management of infectious mononucleosis. J Laryngol Otol 106:989–991
Candy B, Hotopf M (2006) Steroids for symptom control in infectious mononucleosis. Cochrane Database Syst Rev 19(3):CD004402
Acknowledgments
The authors would like to thank Susanne Zapf, Marburg University Hospital, Marburg, Germany, for her invaluable help in translating this clinical guideline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Windfuhr, J.P., Toepfner, N., Steffen, G. et al. Clinical practice guideline: tonsillitis II. Surgical management. Eur Arch Otorhinolaryngol 273, 989–1009 (2016). https://doi.org/10.1007/s00405-016-3904-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-3904-x