Abstract
Th0 cells differentiate into Th1 or Th2 depending on multiple transcription factors acting on specific time points to regulate gene expression. Th17 cells, a subset of IL-17-producing T cells distinct from Th1 or Th2 cells, have been described as key players in inflammation and autoimmune diseases as well as cancer development. In the present study, 53 patients with hypopharyngeal cancer were included. The expression levels of Th1-, Th2- and Th17-associated cytokines in hypopharyngeal cancer tissues and pericarcinoma tissues were detected. The relationship between Th1, Th2, or Th17 infiltration and metastasis was studied. Our results showed that the mRNA and protein expressions of Th1 cytokines were lower, while the expressions of Th2 and Th17 cytokines were higher in tumor tissues, and the intensity of expression was strengthened with clinical stage increasing. Cancer tissues had higher level expressions of Th2 and Th17 cytokines than that of pericarcinoma tissues. From the above data, we speculated that high expressions of Th2- and Th17-associated cytokines in hypopharyngeal carcinoma may contribute to cancer development and metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer progression is a complex process involving host–tumor interactions through multiple molecular and cellular factors of the tumor microenvironment [1]. Compelling evidence has indicated that inflammation contributed to the proliferation, migration, and survival of cancer cells which could result in tumor invasion and metastasis. However, inflammation in the tumor microenvironment was an important component of the tumor-associated immune response. Inflammatory cells and molecules may have played crucial roles in initiating and maintaining tumor immunity [2, 3]. CD4+ T helper cells (Th), as a high heterogeneity and plasticity population, play critical roles in tumor immunological responses [4]. There are four main subsets of CD4+ T helper cells based on their distinct cytokine repertoire that governs the overall immune response through delicate network. These are Th1, Th2, Th17, and T regulatory (Treg) cells [5]. Th1 cells produce hallmark IFNγ, IL-2, IL-12, and TNFα cytokines involved in cell-mediated pro-inflammatory response, these exert potent anti-tumor effects by activating CD8+ cytotoxic T lymphocytes (CTLs), NK-mediated cytotoxicity, and upregulation of MHC expression on APCs. Conversely, Th2 cells secrete IL-4, IL-5, IL-6, IL-10, and IL-13 which mediate anti-inflammatory humoral response and immune suppression by inhibiting Th1 cytokines production [6]. Th17 cells are characterized as IL-17-producing CD4+ T cells which also produce IL-21, IL-22, and IL-26 [7, 8]. It has been reported that retinoid orphan nuclear receptor (ROR-γt) is a key regulator of Th17 cell lineage differentiation [9], and that Th17 cells play critical roles in the development of autoimmunity and allergic reactions [10, 11]. TGFβ1, a prototype of TGFβ family secreted mainly by Tregs, is another multi-functional cytokine. It promotes tumor progression by inducing mesenchymal transition, tumor escape by antagonizing IL-2 functions and inducing immune suppression [12, 13], tumor invasion, and metastasis [14].
In the present study, we investigated the mRNA and protein expressions of Th1-, Th2-, and Th17-associated cytokines at tissue level by reverse transcriptase polymerase chain reactions (RT-PCR) and Western blot to define the role and clinical significance of Th1, Th2, and Th17 cells in hypopharyngeal carcinoma and the pathogenesis of hypopharyngeal carcinoma.
Materials and methods
Study subjects
The present study involved total 60 subjects including 53 patients with histologically proven hypopharyngeal caicinoma and 7 throat injury patients serving as controls which were age and sex matched to the cases. The patients were registered and recruited for the study at the Second Hospital of Shandong University, Jinan, China, during the period of 2011–2013. Fresh surgical specimens were collected from patients undergoing surgery for different stages of squamous carcinoma of the hypopharynx. The tumor staging of the patients was done in accordance with the American Joint Committee on Cancer (AJCC), tumor-node metastasis (TNM) classification. None of the patients had received chemotherapy or radiation therapy and immunotherapy within 2 months prior to surgery. Control non-neoplastic tissues consisted of samples from the irregular mucous edge rejected among tissue repairation of the larynx and hyporpharynx injury patients (approximately a 1 mm × 1 mm × 2 mm piece of tissue was selected, so it did not cause additional harm to the larynx and hoperpharynx functional regaining). Cancer tissues and pericancerous tissues were identified by stereoscopy and quick frozen sectioning. Two pieces of tissues were collected and snp-frozen for RNA extraction and protein preparation. Patients suffering from any other chronic disease such as diabetes, tuberculosis, any other malignancy or autoimmune disease at the time of specimen collection were excluded. Similarly, normal controls who had got fever or viral infection in the past 1 week, pregnancy, or recent accident were also excluded from the study. The protocol was approved by the Ethics committee of Shandong University School of Medicine, and all participants signed informed consent. Representative samples of tumors and of normal control tissues were collected at surgery, were snap-frozen immediately in Eppendorf tubes and stored at −80 °C to avoid RNA and protein degradation until sectioning for RT-PCR and Western blot analysis.
Main reagents
The total RNA extract kit was prepared by our laboratory. M-MLV reverse transcriptase and Taq DNA polymerase were purchased from Promega Corporation (Madison, WI, USA). PCR primers for detecting mRNAs of IFN-γ, IL-2, IL-4, IL-6, IL-10, IL-17A, and β-actin were obtained using the OLIGO Primer Analysis Software, Version 5.0 (NBA, Software and Research Services for Tomorrow’s Discoveries, National Biosciences, Plymouth, MN). The PCR oligomers were synthesized by a DNA/RNA synthesizer (Applied Biosystems) at BioSune biological technology corporation, Shanghai, China. Primer sequences were listed in Table 1. Mouse anti-human IFN-γ monoclonal antibody, mouse anti-human IL-4 monoclonal antibody, mouse anti-human IL-17 monoclonal antibody, and rabbit anti actin polyclonal antibody were purchased from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA). Horseradish peroxidase-labeled goat anti-mouse and anti-rabbit IgG were purchased from Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd. (Beijing, China).
Reverse transcription polymerase chain reaction (RT-PCR)
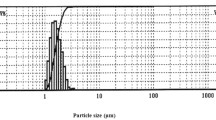
The RT-PCR method was described briefly. RNA was extracted from tissues using the acid-guanidinium phenol–chloroform method. The quality of the RNA yield was assessed by electrophoresis on a 1.5 % agarose gel in 0.5 mol TBE buffer, demonstrating the typical 28S and 18S bands of the total RNA in all RNA yield from the tissues enrolled in this study. Then the amount of each RNA samples was measured by optical density reading, and only RNA samples showing an A260–A280 ratio from 1.8 to 2.0 were used to obtain cDNA. RT-PCR was performed using RNA PCR kit (Perkin-Elmer, Norwalk, CT). Cellular RNA (1 μg) was reversedly transcribed into cDNA in a reaction mixture containing 5 mmol MgCl2, 1 mmol dNTP, 2.5 μmol oligo (dT) primer, 1U RNase inhibitor, and 200U reverse transcriptase (MMLV). After incubation at 37 °C for 60 min, the reaction was terminated by heating at 95 °C for 5 min. PCR was performed using the forward primer and reverse primer listed in Table 1. The PCR reaction buffer (25 μl), consisting 2 mmol MgCl2, 0.5 μmol of each primer, 1U Taq DNA polymerase and 5 μl reverse transcription product. All the items were added to an amplification tube. PCR was run for 33 cycles. Each cycle consisted of 95 °C for l min, 58 °C for l min, and 72 °C for l min. Twenty-microliter aliquots of the amplified product were fractionated on a 1.5 % agarose gel and visualized by ethidium bromide staining. The band intensity of ethidium bromide fluorescence was measured using NIH/1D Image Analysis Software Ver 1.61 (National Institutes of Health, Bethesda, MD). The relative intensity (RI) of each band was determined with the use of the ratio to β-actin. RI = the sum density of the purpose gene/the sum density of β-actin.
Western blotting assay
SDS-PAGE and immunoblotting was performed by standard techniques. In brief, the prepared tissues were lysed at 4 °C for 30 min in lysis buffer [20 mmol Tris-hydrochloric acid (Tris–HCl) (pH 7.5), 1 % Nonidet P-40, 150 mmol Nacl, 1 mmol ethylenediamine tetraacetic acid, 50 U/ml aprotinin, 1 mmol phenylmethylsulfonyl fluoride, and 1 mmol sodium orthovanadate]. The lysates were centrifuged at 15,000 rpm for 20 min at 4 °C to remove nuclei and undisrupted tissues. Protein concentration was determined using Bio-Rad protein assay solution with BSA as standard [15, 16]. The protein samples were boiled for 10 min. The boiled samples were loaded onto a 14 % SDS-PAGE gel and electrophoresis was run for 2 h. Proteins were electrophoretically transferred onto 0.22 µm nitrocellulose membrane and immunoblotted with various primary antibodies (IFNγ, IL-4, IL-17, and β-actin) against different proteins. The immunoblots were visualized using a LAS4000 Chemiluminescence Imager (Fijifilm, Tokyo, Japan) with associated software. For presentation, immunoblots were opened in PhotoShop CS2 (Adobe Systems, Mountain View, CA, USA).
Statistical analysis
To determine each prevalence of Th1, Th2, and Th17 in hypopharyngeal carcinoma, data analysis was performed using SPSS 11.5 (SPSS, Inc., Chicago, IL, USA). Values were expressed as mean ± SD. The Paired-Samples T Test was used to compare the significance of differences between hypopharyngeal carcinoma tissues and pericarcinoma tissues. One-way analysis of variance (ANOVA) analysis was used to compare the significance of differences between groups at different clinical stages. A p value of <0.05 was considered to be statistically significant.
Results
Descriptive features of study groups
Table 2 shows the descriptive characteristics of the study subjects which comprise of 53 hypopharyngeal carcinoma patients with an average age of 60.2 ± 8.74 years (range 47–77 years) and 7 healthy controls with an average age of 45.1 ± 10.35 years (range 32–61 years). Out of total 53 patients 50 (94.3 %) were males and only 3 (5.7 %) were females, giving a sex ratio of 16.7. In accordance with TNM classification, most of the patients were presented with large size tumor (T3 + T4; 67 %) and involving lymph node (N+; 75.5 %). Thus most of the patients were in the advanced stage (III + IV; 86.8 %) of the disease while only 13.2 % had early stage cancer. It was pathologically confirmed that all the patients with squamous cell carcinoma (54.7 %) had poorly differentiated tumors in histological grade.
Th1-associated cytokines present weak expression in hypopharyngeal carcinoma
Total RNA from tissues of 53 hypopharyngeal cancer patients and 7 healthy subjects were prepared, and the cytokine mRNA expression profiles from these tissues were determined by RT-PCR. To exclude the possibility of carry-over contamination, reactions containing all RT-PCR reagents including cytokine PCR primers without sample RNA were used as negative controls. No contamination was detected. Samples of normal supra-glottic mucosa from rejected irregular mucous edge of injury patients were used as controls in 7 cases demonstrated the absence of lympho-mononuclear infiltrates, in which showed almost no Th1-, Th2-, orTh17-associated cytokines expressions (Fig. 1).
The mRNA expressions of Th1-, Th2-, and Th17-associated cytokines in fresh tumor tissues and pericarcinoma tissues from the patients with human hypopharyngeal carcinoma. a Representative mRNA expressions of Th1-, Th2-, and Th17-associated cytokines in tumor tissues of different clinical stages and normal control tissues. The mRNA expressions of IFNγ and IL-2 (Th1) were weaker, and there was no expression in clinical IVstage. Th2-associated cytokine (IL-4, IL-6, and IL-10) showed the main advantage expression. The cytokine expression was strengthened with clinical stage increasing. Th17 cytokine (IL-17A) was in a superiority high level expression, and advanced clinical stage patients had higher level mRNA expression of IL-17A than early clinical stage. There were no expressions of Th1-, Th2-, and Th17-associated cytokines in normal control tissues (1, clinical stage I + II; 2, clinical stage III; 3, clinical stage IV; 4, normal control). b Representative mRNA expressions of Th1-, Th2-, and Th17-associated cytokines in tumor tissues and pericarcinoma tissues. In tumor tissues and pericarcinoma tissues, the expressions of Th1 cytokines were weaker and equivalent level. The expressions of Th2 and Th17 cytokines in tumor tissues were stronger than pericarcinoma tissues (1, tumor tissue; 2, pericarcinoma tissue)
The mRNA expressions of Th1 cytokines IFN-γ and IL-2 in tissues were analyzed. The expressing capacity (measured as relative intensity (RI) to the ratio of β-actin) of patients for Th1 cytokines was in a relatively low level. The results were shown in Figs. 1, 2, 3. In all 53 patients, only 11 cancer tissues (20.7 %) and 17 pericarcinoma tissues (32.1 %) expressed IFN-γ mRNA (RI 0.060 ± 0.122, 0.088 ± 0.134, t = 1.822, p = 0.074); and 8 cancer tissues (15.1 %) and 15 pericarcinoma tissues (28.3 %) expressed IL-2 mRNA (RI 0.051 ± 0.123, 0.075 ± 0.125, t = 1.423, p = 0.161). It was found that patients at the early stage had higher level mRNA expressions of IFN-γ and IL-2 than those at advanced stages. Cancer tissues had lower level mRNA expressions of IFN-γ and IL-2 than pericarcinoma tissues, but did not reach significant difference.
Graphical analysis of relative intensity on mRNA expressions of Th1-, Th2-, and Th17-associated cytokines in hypopharyngeal carcinoma tissues. Th1 cytokines (IFN-γ and IL-2) showed weak expression. It was found that early stage patients had higher level mRNA expressions of IFNγ and IL-2. The mRNA expressions of Th2 cytokines (IL-4, IL-6, and IL-10) and Th17 (IL-17A) were displayed advantage status. The intensity of expression was stronger in later clinical stage than early clinical stage
Graphical analysis of relative intensity on mRNA expressions of Th1-, Th2-, and Th17-associated cytokines in hypopharyngeal carcinoma tissues and pericarcinoma tissues. Th1 cytokines (IFN-γ and IL-2) showed weak expression. Its expression in hypopharyngeal carcinoma tissues was lower than in pericarcinoma tissues. The mRNA expressions of Th2 cytokines (IL-4, IL-6, and IL-10) and Th17 (IL-17A) were displayed advantage status. The intensity of expression was stronger in hypopharyngeal carcinoma tissues than in pericarcinoma tissues. Especially the expression of IL-17A in hypopharyngeal carcinoma tissues and pericarcinoma tissues. It presented significant difference (*P < 0.05)
The dominant expression of Th2-associated cytokines in hypopharyngeal carcinoma
The mRNA expressions of Th2-associated cytokines IL-4, IL-6, and IL-10 in tissues were analyzed. The expressing capacity of patients for Th2 cytokines was in a relatively high level. The results were shown in Figs. 1, 2, 3. In all 53 patients, 32 cancer tissues (60.4 %) and 29 pericarcinoma tissues (54.7 %) expressed IL-4 mRNA (RI 0.317 ± 0.328, 0.272 ± 0.307, t = 1.593, p = 0.117), 26 cancer tissues (49.1 %) and 24 pericarcinoma tissues (45.3 %) expressed IL-6 mRNA (RI 0.292 ± 0.341, 0.258 ± 0.328, t = 1.841, p = 0.071), 37 cancer tissues (69.8 %), and 34 pericarcinoma tissues (64.2 %) expressed IL-10 mRNA (RI 0.420 ± 0.344, 0.370 ± 0.333, t = 1.679, p = 0.099), respectively. It was found that the Th2-associated cytokines showed the main advantage expression in hypopharyngeal carcinoma. The expressions of Th2-associated cytokines tended to go up with increasing of clinical stages. The mRNA expressions of IL-4, IL-6, and IL-10 in cancer tissues were higher than in pericarcinoma tissues, but there was no significant difference.
Th17-associated cytokine IL-17A predominantly expressed in hypopharyngeal carcinoma
The mRNA expression of Th17-associated cytokine IL-17A in tissues was analyzed. The expressing capacity of patients for Th17 cytokines was in a superiority high level. The results were shown in Figs. 1, 2, 3. In all 53 patients, 48 cancer tissues (90.6 %) and 33 pericarcinoma tissues (62.2 %) expressed IL-17A mRNA (RI 0.397 ± 0.259, 0.239 ± 0.203, t = 2.900, P = 0.007). It was found that patients at the advanced clinical stages had higher level mRNA expression of IL-17A. Especially in clinical stage III, its expression was the strongest (RI 0.436 ± 0.247). Cancer tissues had significantly higher level mRNA expression of IL-17A than pericarcinoma tissues.
Immunoblotting detect associated cytokines protein expression in hypopharyngeal carcinoma
The protein expressions of Th1-, Th2-, and Th17-associated cytokines were analyzed by Western blot analysis. We selected IFN-γ as Th1, IL-4 as Th2, and IL-17A as Th17 for the experiment. The results revealed that the protein expressions of IFN-γ, IL-4, and IL-17 were as same as the mRNA expressions in hypopharyngeal carcinoma and pericarcinoma tissues. There were almost no IFN-γ, IL-4 and IL-17 protein expressions in normal control. IFN-γ expression was not detectable or very weak in hypopharyngeal carcinoma or pericarcinoma tissues. IL-4 expression maintained superiority in hypopharyngeal carcinoma tissues. The advanced stage (III or IV) expression was higher than the early stage (I + II). The cancer tissue expression was higher than the pericarcinoma tissue in every stage. IL-17A expression was very strong in hypopharyngeal carcinoma tissues. The advanced stage expression was higher than the early stage. The cancer tissue expression was stronger than the pericarcinoma tissue in every stage (Fig. 4).
The protein expressions of IFN-γ, IL-4, and IL-17 in fresh tumor tissues and pericarcinoma tissues from the patients with human hypopharyngeal carcinoma. A Representative Protein expressions of IFNγ, IL-4, and IL-17 in tumor tissues of different clinical stages and normal control tissues. The IFN-γ expression was weaker, and there was no expression in clinical IV stage. IL-4 and IL-17 showed the main advantage expression. Patients at the advanced clinical stage had higher level protein expressions of IL-4 and IL-17 than those at early clinical stage. There were no protein expressions of IFN-γ, IL-4, and IL-17 in normal control tissues (1, clinical stage I + II; 2, clinical stage III; 3, clinical stage IV; 4, normal control). b Representative protein expressions of IFN-γ, IL-4, and IL-17 in tumor tissues and pericarcinoma tissues. In tumor tissues and pericarcinoma tissues, the expression of IFNγ was weaker and equivalent level. The protein expressions of IL-4 and IL-17 in tumor tissues were stronger than that in pericarcinoma tissues (1, tumor tissue; 2, pericarcinoma tissue)
Discussion
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common cancer in the world and ~500,000 cases are diagnosed every year [17]. Hypopharyngeal cancer is undifferentiated squamous cell carcinoma (HSCC). It represents a distinct clinical entity among other cancers of the head and neck region. It is less prevalent than other head and neck cancers, accounting for 3–5 % of all HNSCC in the region [18, 19]. It is usually difficult to detect hypopharyngeal carcinoma at an early stage because of inconspicuous pharyngeal symptoms [20]. In spite of considerable advances in multimodality therapy, including surgery, radiotherapy, and chemotherapy, the overall survival rate for patients with HSCC is only 15–45 % [21, 22]. It presents unique therapeutic challenges to clinical oncologists as well as ablative and reconstructive surgeons. These patients usually present late, with 60–80 % of the patients having ipsilateral nodal metastasis [23] and up to 40 % of them have contralateral occult nodal tumor deposits on presentation [24]. Furthermore, systemic metastasis is reported to occur in up to 60 % of the patients [25], either at presentation or during follow-up. Patients with HSCC are usually diagnosed at a late stage, and local tumor recurrence and distant metastasis occur quite commonly after conventional therapies, which are the primary cause for poor survival of HSCC [21, 22].
There is a lack of effective strategy for the best treatment [20, 26], therefore it still remains controvertial on treatment regimens [27]. In this study, all the patients were squamous cell carcinoma, involving 75.5 % patients have lymph node metastasis. 86.8 % of the patients were in the advanced clinical stage (III + IV), moderately differentiated and poorly differentiated accounted for 88.7 % of all the patients. The classification of the patients was consistent with the literatures reported previously.
In the recent history, accumulating evidences have directly altered the traditional paradigm of Th1/Th2 cytokine classification to include two new subsets of CD4+ T cells defined by their discrete cytokine profiles. These are referred as Th17 and Treg cells which mainly produce IL-17 and TGFβ family of cytokines, respectively [28]. These cytokines together with other molecules operate in a complex, tightly regulated network controlling immune functions. Perturbations of this network may lead to immune dysfunction, uncontrolled cell growth, chronic inflammation, and ultimately carcinogenesis [12]. In this study, we tried to elaborate the intricate balance between three major arms of cytokines in context with hypopharyngeal carcinoma patients.
Th1 cells that mainly express IL-2 and IFN-γ enhance immunogenic cellular cytotoxicity, induce delayed-type hypersensitivity reaction (DTH), and are responsible for cell-mediated immunity. Th2 cells which principally secrete IL-4, IL-6, and IL-10 are more potent helpers for antibody production, regulate humoral immune responses. The imbalance of Th1/Th2 status in human being may cause infections with microbes such as bacteria and virus, and is involved in allergic disease and autoimmune disorder [29]. Clinical information also suggests that Th1 response is suppressed and Th2 response is elevated systemically in some tumor patients (colon cancer, lung cancer, melanoma et al.), suggesting that Th2 cytokines may mediate immunosuppression [30–33].
Th2-mediated immunosuppression reduced the protective cellular immunity and was found to be associated with tumor progression [34]. Th1 cytokines appear to have a protective function, whereas Th2 cytokines seem to favor tumor growth. In the present study, our data further confirmed that the Th2-associated cytokines showed the main advantage expression in hypopharyngeal carcinoma, which was supported by the finding that IL-4, IL-6, and IL-10 levels, but not IFN-γ and IL-2, were significantly higher in tissues from hypopharyngeal cancer patients. The Th2-associated cytokines expression was strengthened with clinical stage increasing. Cancer tissues had higher level mRNA expressions of IL-4, IL-6, and IL-10 than pericarcinoma tissues in every clinical stage. The expressions of Th1 cytokines were inhibited with a concomitant predominant state of Th2 cytokines produced by tissues from hypopharyngeal cancer patients, which might at least partly explain the suppressed immune response against tumor in these patients.
Furthermore, a newly introduced subset Th17 cells that predominantly produce IL-17 family of cytokines (IL-17A–F) is gaining popularity in context of tumor biology although its specific role remains elusive [28]. It was shown that Th17 cells are involved in tissue inflammation through the induction of the release of the cytokines IL-8, IL-6, COX-2, MMP-1, MMP-3, CXCL1, and NOS-2 by surrounding cells such as fibroblasts, macrophages, endothelial, and epithelial cells [35, 36] which are involved in angiogenesis, tumor invasion, and metastasis [37, 38]. On this account, it is reasonable to propose an impact of Th17 cells on cancer progression and pathogenesis. In ovarian cancer, it was shown that Th17 cells are increased in tumor tissue [39]. In gastric cancer, there were both an elevation of Th17 frequency in peripheral blood and TDLNs the Th17 response increased with advanced gastric cancer [40]. High levels of Th7 cells also appeared in oral squamous cell carcinoma [41], bladder carcinoma [42], Colon cancer [43], and central nervous system tumors such as glioblastoma [44, 45] and cerebellar medulloblastoma [46]. It suggested that Th17 cells infiltration is a common characteristic of malignant tumor. In this study, it was found that advanced clinical stage patients had higher level mRNA expression of IL-17A in hypopharyngeal cancer patients. Especially in clinical stage III, its expression was the strongest. Cancer tissues had higher level mRNA expression of IL-17A than pericarcinoma tissues. It presents significant difference in all clinical stage (P < 0.05). It showed that the hypopharyngeal cancer patients with poor prognosis may be caused by higher expression Th17-associated cytokines in tumor microenvironment.
In this study, we considered the influence of cytokine levels in conjunction with other clinico-pathological parameters. Apparently males with age more than 50 years are more susceptible to hypopharyngeal cancer development. The expressions of Th1-, Th2-, and Th17-associated cytokines were irrelevant to the tumor size, lymph node metastasis, and pathological classification. It may be due to the majority cases are in advanced stage. There were some limitations in this study. The number of cases, especially those with clinical early stages (I + II) was small. We will collect more clinical cases and do more meticulous research in the future.
In conclusion, our study showed a marked shift toward Th2 (IL-4, IL-6, IL-10) and Th17 (IL-17) cytokines in hypopharyngeal cancer patients during disease progression. Since their elevated mRNA and protein levels were associated with increased advanced clinical stages, and their expression levels in cancer tissues were higher than in pericarcinoma tissues. These can be exploited as potential complementary biomarkers with high sensitivities and specificities. The detection of Th1-, Th2-, and Th17-associated cytokines is helpful in diagnosing hypopharyngeal neoplasms and analysing its pathogenesis. Our findings indicate that Th1, Th2, and Th17 lymphocyte differentiation might play critical roles in tumor microenvironment, suggesting that adoptive immunotherapy may be developed through modulation helper T cell population in the future.
References
Tosolini M, Kirilovsky A, Mlecnik B et al (2011) Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, Th2, Treg, Th17) in patients with colorectal cancer. Cancer Res 71:1263–1271
Su Z, Sun Y, Zhu H et al (2014) Th17 cell expansion in gastric cancer may contribute to cancer development and metastasis. Immunol Res 58:118–124
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444
Zhu J, Paul WE (2010) Heterogeneity and plasticity of T helper cells. Cell Res 20:4–12
Hirahara K, Ghoreschi K, Laurence A, Yang XP, Kanno Y, O’Shea JJ (2010) Signal transduction pathways and transcriptional regulation in Th17 cell differentiation. Cytokine Growth Factor Rev 21:425–434
Wei H, Sun R, Xiao W et al (2004) Type two cytokines predominance of human lung cancer and its reverse by traditional Chinese medicine TTMP. Cell Mol Immunol 1:63–70
Dong C (2006) Diversification of T-helper-cell lineages: finding the family root of IL-17-producing cells. Nat Rev Immunol 6:329–333
Bettelli E, Carrier Y, Gao W et al (2006) Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature 441(7090):235–238
Yang XO, Pappu BP, Nurieva R et al (2008) T helper 17 lineage differentiation is programmed by orphan nuclear receptors ROR alpha and ROR gamma. Immunity 28:29–39
Ouyang W, Kolls JK, Zheng Y (2008) The biological functions of T helper 17 cell effector cytokines in inflammation. Immunity 28:454–467
Maruyama T, Kono K, Mizukami Y et al (2010) Distribution of Th17 cells and FoxP3(+) regulatory T cells in tumor-infiltrating lymphocytes, tumor-draining lymph nodes and peripheral blood lymphocytes in patients with gastric cancer. Cancer Sci 101:1947–1954
Gaur P, Singh AK, Shukla NK, Das SN (2014) Inter-relation of Th1, Th2, Th17 and Treg cytokines in oral cancer patients and their clinical significance. Hum Immunol 75:330–337
Wrzesinski SH, Wan YY, Flavell RA (2007) Transforming growth factor-beta and the immune response: implications for anticancer therapy. Clin Cancer Res 13:5262–5270
Jakowlew SB (2006) Transforming growth factor-beta in cancer and metastasis. Cancer Metastasis Rev 25:435–457
Chen XM, Xu XQ, Sun K, Hallett WH, Zhao JD, Zhang DL (2008) NKG2D ligands expression and NKG2D-mediated cytotoxicity in human laryngeal squamous carcinoma cells. Scand J Immunol 67:441–447
Maarof G, Bouchet-Delbos L, Gary-Gouy H, Durand-Gasselin I, Krzysiek R, Dalloul A (2010) Interleukin-24 inhibits the plasma cell differentiation program in human germinal center B cells. Blood 115:1718–1726
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300
Hall SF, Groome PA, Irish J, O’Sullivan B (2008) The natural history of patients with squamous cell carcinoma of the hypopharynx. Laryngoscope 118:1362–1371
Cooper JS, Porter K, Mallin K et al (2009) National Cancer Database report on cancer of the head and neck: 10-year update. Head Neck 31:748–758
Sasaki CT, Jassin B (2001) Cancer of the pharynx and larynx. Am J Med 111:118S–123S
Takes RP, Strojan P, Silver CE et al (2012) Current trends in initial management of hypopharyngeal cancer: the declining use of open surgery. Head Neck 34:270–281
Chan JY, Wei WI (2013) Current management strategy of hypopharyngeal carcinoma. Auris Nasus Larynx 40:2–6
Gourin CG, Terris DJ (2004) Carcinoma of the hypopharynx. Surg Oncol Clin N Am 13:81–98
Buckley JG, MacLennan K (2000) Cervical node metastases in laryngeal and hypopharyngeal cancer: a prospective analysis of prevalence and distribution. Head Neck 22:380–385
Kotwall C, Sako K, Razack MS, Rao U, Bakamjian V, Shedd DP (1987) Metastatic patterns in squamous cell cancer of the head and neck. Am J Surg 154:439–442
Robson A (2002) Evidence-based management of hypopharyngeal cancer. Clin Otolaryngol Allied Sci 27:413–420
Allal AS (1997) Cancer of the pyriform sinus: trends towards conservative treatment. Bull Cancer 84:757–762
Murugaiyan G, Saha B (2009) Protumor vs antitumor functions of IL-17. J Immunol 183:4169–4175
Mosmanm TR, Sad S (1996) The expanding universe of T-cell subsets: Th1, Th2 and more. Immunol Today 17:138–146
Yamamura M, Modlin RL, Ohmen JD, Moy RL (1993) Local expression of antiinflammatory cytokines in cancer. J Clin Invest 91:1005–1010
Oshikawa K, Yanagisawa K, Ohno S, Tominaga S, Sugiyama Y (2002) Expression of ST2 in helper T lymphocytes of malignant pleural effusions. Am J Respir Crit Care Med 165:1005–1009
Chen YM, Yang WK, Whang-Peng J, Tasi CM, Perng RP (2001) An analysis of cytokine status in the serum and effusions of patients with tuberculous and lung cancer. Lung Cancer 31:25–30
Kharkevitch DD, Seito D, Balch GC, Maeda T, Balch CM, Itoh K (1994) Characterization of autologous-specific T-helper 2 cells in tumor-infiltrating lymphocytes from a patient with metastatic melanoma. Int J Cancer 58:317–323
Chtanova T, Mackay CR (2001) T cell effector subsets: extending the Th1/Th2 paradigm. Adv Immunol 78:233–266
Agarwal S, Misra R, Aggarwal A (2008) Interleukin 17 levels are increased in juvenile idiopathic arthritis synovial fluid and induce synovial fibroblasts to produce proinflammatory cytokines and matrix metalloproteinases. J Rheumatol 35(3):515–519
Gu Y, Hu X, Liu C, Qv X, Xu C (2008) Interleukin (IL)-17 promotes macrophages to produce IL-8, IL-6 and tumour necrosis factor-alpha in aplastic anaemia. Br J Haematol 142:109–114
Nabeshima K, Inoue T, Shimao Y, Sameshima T (2002) Matrix metalloproteinases in tumor invasion: role for cell migration. Pathol Int 52:255–264
Li A, Dubey S, Varney ML, Dave BJ, Singh RK (2003) IL-8 directly enhanced endothelial cell survival, proliferation, and matrix metalloproteinases production and regulated angiogenesis. J Immunol 170:3369–3376
Miyahara Y, Odunsi K, Chen W, Peng G, Matsuzaki J, Wang RF (2008) Generation and regulation of human CD4+ IL-17-producing T cells in ovarian cancer. Proc Natl Acad Sci USA 105:15505–15510
Zhang B, Rong G, Wei H et al (2008) The prevalence of Th17 cells in patients with gastric cancer. Biochem Biophys Res Commun 374:533–537
Lee JJ, Chang YL, Lai WL et al (2011) Increased prevalence of interleukin-17-producing CD4(+) tumor infiltrating lymphocytes in human oral squamous cell carcinoma. Head Neck 33:1301–1308
Chi LJ, Lu HT, Li GL et al (2010) Involvement of T helper type 17 and regulatory T cell activity in tumour immunology of bladder carcinoma. Clin Exp Immunol 161:480–489
Su X, Ye J, Hsueh EC, Zhang Y, Hoft DF, Peng G (2010) Tumor microenvironments direct the recruitment and expansion of human Th17 cells. J Immunol 184:1630–1641
Wainwright DA, Sengupta S, Han Y, Ulasov IV, Lesniak MS (2010) The presence of IL-17A and T helper 17 cells in experimental mouse brain tumors and human glioma. PLoS One 5:e15390
Cantini G, Pisati F, Mastropietro A et al (2011) A critical role for regulatory T cells in driving cytokine profiles of Th17 cells and their modulation of glioma microenvironment. Cancer Immunol Immunother 60:1739–1750
Zhou P, Sha H, Zhu J (2010) The role of T-helper 17 (Th17) cells in patients with medulloblastoma. J Int Med Res 38:611–619
Acknowledgments
The present study was supported by grants from the Natural Science Foundation of Shandong Province (No. ZR2013HL028, ZR2010CM067), Shandong Province Outstanding Young Scientist Award Fund (No. BS2009SW007), the Special Research Foundation of Large Scientific Instruments on Upgrading and Technological Transformation of Shandong Province (No. 2013SJGZ09) and the Seed Foundation of the Second Hospital of Shandong University (No. S2013010021).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Chen, X., Wang, J., Wang, R. et al. Th1-, Th2-, and Th17-associated cytokine expression in hypopharyngeal carcinoma and clinical significance. Eur Arch Otorhinolaryngol 273, 431–438 (2016). https://doi.org/10.1007/s00405-015-3779-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3779-2