Abstract
The objective of this review is to compare the symptomatological evolution following conservative management (CM) or microsurgery (MS) in patients with intralabyrinthine schwannomas (ILS). A thorough systematic review of the English and French literature from 1948 to February 2014 was performed using Ovid Medline. An ancestor search was also completed. The major inclusion criterion consisted of a diagnosis of ILS with magnetic resonance imaging. Patients with a classic vestibular schwannoma, cases of incidentaloma during surgery or an autopsy were the main exclusion criteria. Thirty-one studies met our selective criteria. Descriptive data were collected from the articles. Clinical outcomes regarding the hearing loss, tinnitus, vertigo, dizziness and aural fullness were stated as improved, unchanged or worse at the last follow-up. All data were then separated into two different groups according to the management option: CM and MS. The data were analyzed using a Pearson χ 2 test and Fisher’s exact test. This meta-analysis suggests that MS has a statistically significant favorable outcome regarding symptom relief compared to CM in patients with ILS suffering from tinnitus, vertigo and dizziness. Hearing level was not compared between treatment groups, as MS leads to anacusis. An indicative bias was the main limitation of this study, as patients suffering from intractable vertigo with moderate-to-severe hearing loss were referred to MS. Therefore, in the presence of a serviceable hearing, we suggest that CM should be the treatment of choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intralabyrinthine schwannomas (ILS) are rare benign tumors originating from the Schwann cells of the cochlear and vestibular nerve terminal ends [1]. They represent a different entity from the vestibular schwannoma (VS), in which the tumor arises from the vestibular nerve in the medial internal auditory canal (IAC) or at the lateral cerebellopontine angle (CPA) [2]. ILSs are further subdivided according to their location within the inner ear. In 2004, Kennedy et al. proposed a classification system of seven subtypes, reviewed in 2013 by Van Abel et al. who added three more subtypes, in order to adopt a more explicit nomenclature regarding the anatomical location of the tumor (Table 1) [3, 4]. Moreover, Van Abel et al. have suggested renaming ILS to primary inner ear schwannomas (PIES).
Controversy remains over the origin of these tumors. Namely, the nomenclature PIES implies a vestibular or cochlear origin, differentiating them from VS with or without inner ear invasion [5–9]. With this perspective, it is reasonable to expect that some VS can be wrongly labeled as PIES.
In order to facilitate the understanding, ILS will be used for all schwannomas and isolated ILS will be used when the tumor is restricted to the labyrinth such as intracochlear (IC), intravestibular (IV) and intravestibulocochlear (IVC) schwannomas.
IC schwannoma seems to be the most common subtype of ILS [4, 9]. However, there is an inconsistency concerning this information [4, 10–13]. SCCs are less frequently involved [14]. Surprisingly, clinical manifestations do not significantly vary with the tumor location [9, 15].
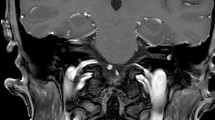
ILS are challenging to diagnose because they induce unspecific symptoms, such as hearing loss, tinnitus, dizziness, vertigo and aural fullness. Before 1990, ILS were incidentally found during otologic surgeries for what was believed to be Meniere’s disease or during autopsies [16]. Since the advent of MRI, an increased number of ILS are diagnosed during the investigation of unilateral hearing loss or vertigo. To date, a little over 340 cases of ILS have been reported [4, 9]. High-resolution MRI with gadolinium enhancement is the gold standard for ILS diagnosis and manages to identify tumors as small as 2 mm [17]. However, a high index of suspicion for ILS is still needed as some cases remain undiagnosed during the screening of the CPA or IAC [7–9, 18].
Since ILS have a low incidence, no guidelines about the management options are yet available. Multiple case-reports or small case-series have suggested interesting avenues such as conservative management (CM), microsurgery (MS), stereotactic radiotherapy, chemical labyrinthectomy and intratympanic steroid treatment [19, 20]. Also, two different algorithm approaches have been proposed, depending on the IAC involvement [5].
Conservative management, or watch-and-scan, is a good option for patients complaining of serviceable hearing loss without other disabling symptoms, as MS would likely lead to anacusis. Also, even if the tumor size progresses over time, it does not inevitably lead to symptom aggravation [21].
Indications for MS have included diminished residual hearing with or without incapacitating tinnitus, intractable vertigo, or involvement of the IAC, CPA or middle ear. In 1972, both Karlan and Wanamaker accomplished the two first IC schwannoma excisions, reported in two independent articles [22, 23].
Stereotactic radiotherapy is less indicated for ILS, as MS for ILS has less complications than MS for VS [19].
Chemical labyrinthectomy has been used in rare cases when patients were suffering from vestibular symptoms without auditory complaints. As stated by Van Abel et al. [4] in 2013, this strategy may reduce symptoms, but it does not prevent tumor growth.
Finally, Schutt and Kveton [24] have suggested a cochlear implantation after an ILS resection, which can lead to symptom relief associated with a significant hearing improvement.
Overall, ILS management remains controversial [19, 25] as this slow-growing tumor continues to cause vestibulocochlear symptoms. Nevertheless, CM and MS remain the two most common treatment options. Thus, the aim of this study is to conduct a meta-analysis to compare the symptomatological evolution following a CM or MS in patients with ILS.
Methods
Data sources and search strategy
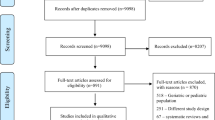
A thorough systematic review of the English and French literature from 1948 to February 2014 was performed using Ovid Medline. The following keywords alone and in various combinations were used: intralabyrinthine schwannomas, intracochlear schwannomas, intravestibular schwannomas, inner ear tumor, hearing loss, vertigo, dizziness, tinnitus, aural fullness, magnetic resonance imaging, conservative management, wait and see, follow-up and surgery. An ancestor search was also completed. An outline of the study selection process is depicted in Fig. 1.
Data collection
When available, data extraction included: total number of patients, patient characteristics (sex, age at diagnosis), tumor characteristics (tumor location according to the Modified Kennedy Classification System [4], tumor subsite, tumor size), hearing level at initial presentation and if tinnitus, vertigo, dizziness and aural fullness were present, management option, post-operative complications, duration of follow-up and clinical outcomes. Clinical outcomes were stated as improved, unchanged or worse for each of the five symptoms (hearing level, tinnitus, vertigo, dizziness and aural fullness). Since hearing level was not uniformly reported by all the authors, the same equivalence hearing scale previously used by our group was used to describe patient hearing level (Table 2) [26, 27]. When needed, authors of the selected studies were contacted to complete the missing data. All data were then separated into two different groups according to the treatment choice: CM and MS. Three different subgroups were also formed to allow further analysis: isolated ILS, schwannomas exceeding the labyrinth/SCCs and CM patients having undergone MS.
Statistical analysis
All data were tabulated using Microsoft Excel. Continuous variables were described with mean, median and range. Nominal features were summarized with frequency and percentage. Association between management type and clinical outcomes was evaluated with Pearson χ 2 test and Fisher’s exact test. Statistical analyses were run using SPSS 21.0 (IBM Co., Armonk, NY). Statistical significance was considered at a p value <0.05.
Results
Thirty-one articles met the selective criteria and were included in this meta-analysis, yielding 66 patients [1, 4, 5, 10, 14, 15, 17–21, 28–47] (Table 3). Descriptive data of both groups are shown in Table 4. Initial symptomatology occurrence is shown in Fig. 2a, b. Tinnitus was associated to IC schwannoma in CM group and to IV schwannoma in MS group (48.4 and 31.3 %, respectively). Vertigo was most often associated to IV schwannoma in both groups (77.8 and 40 % in CM and MS groups, respectively). Finally, dizziness was equally associated to IC and IV schwannomas (42.9 and 33.3 % in CM and MS groups, respectively). The correlation between treatment options and patients’ age at diagnosis is shown in Fig. 3.
ILS: symptom outcomes
Sixty-six patients were included in these analyses. There was a statistically significant difference in tinnitus outcome, with an improvement in 50.0 % of cases in the MS group compared to none in the CM group (p < 0.001) (Fig. 4a). Tinnitus was unchanged and worse in 87.1 and 12.9 % of CM cases, respectively, and was unchanged and worse in 42.9 and 7.14 % of MS cases, respectively. The outcome of vertigo was also statistically significantly better in MS patients, showing improvement in 100 % of cases, compared to 22.2 % in the CM cases (p < 0.001) (Fig. 4a). Vertigo was unchanged in 66.7 % and worse in 11.1 % of patients in the CM group. Concerning dizziness, all MS patients showed an improvement, compared to none in the CM group (p = 0.001) (Fig. 4a). Stable dizziness at the last follow-up was found in all CM cases.
Hearing outcomes were not compared between the two groups, as MS leaves no residual hearing. Hearing status outcomes in the CM group were the following: 1 (2.3 %) patient reported an improvement with a follow-up of 15 months, 31 (70.5 %) had stable hearing levels with a mean follow-up of 31.67 months and 12 (27.3 %) noted a hearing loss progression with a mean follow-up of 24.08 months. The improvement was reported in a patient who received an intratympanic steroid treatment. Unfortunately, not all the patients of the MS group had their hearing outcome evaluated. Thus, of the available data, 18 patients (90.0 %) had a class D hearing level pre- and post-operatively and 2 patients (10.0 %) had a class C at initial presentation worsening to class D postoperatively (Fig. 4b).
At the last follow-up, no patients have reported a new-onset tinnitus or dizziness. However, six patients of the CM group (17.1 %) reported a new onset of vertigo, compared to 1 MS patient (3.3 %), which was not statistically significantly different (p = 1.000).
Overall symptomatology pre- and post-CM and MS
Disregarding hearing loss, the number of symptoms at the initial presentation and at the last follow-up for the CM and MS groups are reported in Fig. 5. Initially, no patient suffered from the four symptoms simultaneously. Postoperatively, eight patients had one symptom: seven cases (87.5 %) still suffered from tinnitus and one case (12.5 %) reported a new onset of vertigo.
Overall symptoms at initial presentation (a) and last follow-up (b). Conservative management group patients with 0, 1, 2 and 3 symptoms had a mean follow-up time of 18.5, 32.2, 31.0 and 24.0 months, respectively. Microsurgery group patients with 0 or 1 symptom had a mean follow-up time of 15.9 and 15.9 months, respectively
Isolated ILS: symptom outcomes
Fifty-six patients of the 66 previous patients composed a subgroup of isolated ILS: 29 (50.9 %) IC schwannomas, 21 (38.2 %) IV schwannomas and 6 (10.9 %) IVC schwannomas. Forty-two patients had CM (24 IC; 14 IV; 4 IVC) and 14 patients had MS (5 IC; 7 IV; 2 IVC). Concerning tinnitus, an improvement was seen in 33.3 % of MS cases, compared to none in the CM group (p = 0.011). CM patients reported unchanged tinnitus in 85.7 % of cases and worse tinnitus in 14.3 % of cases. Again, not all the patients had their complete symptomatology evaluated during the last follow-up. Of the available data in the MS group, 4 patients (44.4 %) had stable tinnitus and 2 patients (22.2 %) reported tinnitus worsening. There was also a statistically significant difference between both groups in the vertigo outcome: 100.0 % of patients in the MS group compared to 25.0 % of the CM group reported an improvement (p = 0.002). Unchanged and worse vertigo was reported in 62.5 and 12.5 % of CM cases, respectively. Dizziness at the last follow-up showed a statistically significant difference between the two groups with an improvement reported in all cases of MS group compared to 0 % in the CM group (p = 0.018). All cases in the CM group reported unchanged dizziness (Fig. 6).
Schwannomas exceeding the labyrinth and the SCCs
Ten of the total 66 patients comprised this subgroup: 5 TMOD, 1 TMAC, 1 Tlab and 3 + CPA. Eight patients underwent MS (4 TMOD; 1 Tlab; 3 + CPA) and 2 had CM (TMOD; 1 TMAC) (Fig. 6).
MS salvage following CM
Among the 44 patients in the CM group, 8 patients (5 IC; 1 IV; 2 IVC) underwent MS following a mean follow-up duration of 18.5 months. The latter patients failed CM due to: tumor progression (n = 3), hearing loss progression (n = 3), tinnitus aggravation (n = 1), new onset of vertigo (n = 4), vertigo aggravation (n = 1), new onset of dizziness (n = 4) and new onset of facial weakness (n = 1). Postoperative symptom outcomes showed vertigo and dizziness improvement in all cases, whereas tinnitus and facial weakness remained unchanged in two different cases (Fig. 6 c, d).
Discussion
Since the first discovered ILS in 1917 [48], different management options and algorithms have been proposed to alleviate patients’ symptomatology [3–5, 8, 12, 15, 18, 19, 21, 33, 44, 49–52]. However, because ILSs are infrequent, no study has evaluated the difference between treatment options and their outcomes. Thus, the aim of this meta-analysis is to compare the effectiveness of CM versus MS on the clinical evolution in order to shed light on the best available treatment for ILS.
The initial presenting symptoms, from the most to the least prevalent, consisted of hearing loss, tinnitus, vertigo, dizziness and aural fullness. Both groups were not initially comparable, especially for vertigo, as a statistical difference was found between CM and MS. This finding suggests that an indicative bias may have differentiated both groups, as patient suffering from intractable vertigo were referred to MS. It is interesting to note that all of these patients also had a class D hearing level. Thus, MS is not indicated for patients with serviceable hearing, even when they suffer from tinnitus, vertigo, dizziness or aural fullness as these symptoms seem less incapacitating and more acceptable. Consequently, the treatment choice is influenced by the hearing level and the patients’ age, as older patients had more morbidity and their tumor growth is relatively slower. Also, hearing preservation remains debatable following stereotactic radiotherapy and it may induce facial palsy [4, 10, 21, 47, 53].
Hearing loss was worse in the MS group than the CM group, with Class D hearing loss counting for 95.2 % of cases with MS, compared to 55.3 % with CM. Van Abel et al. [4] estimated that 84 % of patients suffering from ILS have a class D hearing loss at initial presentation. In their multicenter ILS study, Dubernard et al. [9] stated that profound hearing loss was found in one-third of cases. It has been reported that the clinical symptoms of ILSs are more severe than those of VS, since the former may transmit an altered stimulus to an intact nerve [9, 41, 54]. Finally, initial presentation with facial palsy has been rarely reported and may be consider as a sign of severity of the disease [9].
The association between tumor location and symptomatology were not always predictable [9, 15]. The tumor compression does not only produce a local effect, but may produce endolymphatic hydrops, nerve compression or vascular supply impairment, which could explain the unspecific otologic complaints of ILS [14, 35, 55]. The vertigo characteristics related to ILS are those of a peripheral one, with intermittent attacks lasting a few minutes to several hours, accompanied with nausea and vomiting [10, 19, 39, 43, 49, 56–62]. Considering the rarity of ILS, association between tumor location and symptomatology remains speculative. Surprisingly, the PSCC was never exclusively affected, compared to the two other SCCs. This may suggest that the origin of the ILS does not involve the inferior vestibular nerve.
Although MS is an invasive treatment, facial palsy and other morbidity have a low incidence following the procedure [5, 49]. Three different approaches have been described: translabyrinthine, transotic and a labyrinthectomy. The first two were the most often reported. The translabyrinthine approach is a good option when the schwannoma involves the vestibule. However, since the latter does not allow for a proper access to the cochlea, a cochlear involvement usually requires the transotic approach [8, 18, 46, 63].
ILS: symptom outcomes
Tinnitus, vertigo and dizziness were compared in both groups, while hearing loss was excluded as MS automatically lead to deafness. Aural fullness was also not included in our analyses due to an important lack of data. Regarding tinnitus, the MS group showed a statistically significant improvement compared to the CM group. This result is somewhat surprising, since tinnitus is often related to hearing loss as it is proposed by the central theory [64]. Also, tinnitus is a highly subjective symptom, limiting its reliability. However, this information bias remains a non-differential misclassification as both group had the same limitation. Since single-blind trials are not feasible, this result may have a considerable placebo effect or a participant response bias. Unchanged tinnitus was observed in the majority of cases in the CM group.
Vertigo was resolved in all patients having undergone MS. It can be suggested that the tumor resection allows the abolition of the atypical peripheral signal. In the CM group, there were also some cases (22.2 %) that showed vertigo improvement. This improvement may be related to an adaptation response of the vestibular system over time [9]. Nevertheless, the majority of patients had no change in their vertigo, as expected. A similar conclusion can be made about dizziness; all patients of the MS group had an improvement, while all patients of the CM group had no change in their dizziness.
Even if hearing status was not compared between CM and MS, it is interesting to note that 72.8 % of cases in the CM group showed a preserved hearing. Since expected growth of ILS is similar to VS, estimated to be 1.8–2.4 mm/year [15], and that the mean follow-up time in CM group was only 2.4 years, it may not be long enough to represent the natural history of these tumors [19]. However, this observation may be erroneous, as our study had a limited number of patients. A previous study of our group has shown that hearing preservation in CM for VS is obtained in 58.5 % of cases with a 5-year follow-up. Also, as hearing loss is categorized in 4 different classes, it may lack finesse to described a true hearing loss variation. Thus, the term unchanged hearing loss may in fact imply a significant hearing status change for the patient. The Hearing Classification of Consensus Meeting Guidelines has suggested another classification system with six classes, which may demonstrate a more specific difference among the hearing levels [65]. Finally, one patient in the CM group regained hearing function after receiving 5 doses of intratympanic corticosteroids with a 15-month follow-up. As it was stated, the improvement was likely attributed to the reduction of the inflammatory component [20]. Thus, this intervention may be adopted to improve the hearing loss due to ILS.
We also evaluated the overall symptomatology pre- and post-treatment option. Once again, hearing loss was not considered since almost every patient suffered from this symptom. In the CM group, the majority of patients had one symptom at initial presentation and still showed one symptom at the last follow-up. Three cases had no symptoms initially, except for hearing loss, and suffered from 2 at their last follow-up. Therefore, with CM, the best result that can be expected is an unchanged overall symptomatology, while the number and severity of the symptoms can increase with time. In the MS group 12 patients suffered from 2 or more symptoms at diagnosis while no patient had more than 1 symptom following MS. In fact, postoperatively, the majority of these 12 patients had no symptoms altogether. Overall, 8 patients remained with one symptom at their last follow-up, of which 7 complained of tinnitus. Therefore, our study shows that patients who undergo MS will likely have little to no symptom following their surgery, with tinnitus being the hardest to relieve following MS [12].
Overall, MS has a better outcome than CM, regarding tinnitus, vertigo and dizziness. However, it must be noted that the follow-up length is short, the total number of cases analyzed is not optimal and an indicative bias is likely present, as seen with vertigo.
Isolated ILS
Since the true anatomical origin of ILS is debatable in the literature, a subgroup of ILS arising de novo in the labyrinth was analyzed. This subgroup revealed the same results as those of the ILS group.
Schwannomas exceeding the labyrinth and SCCs
Due to the small number of patients with schwannomas exceeding the labyrinth and SCCs (n = 15), no statistical analyses were performed.
Salvage MS
Eight patients from the CM group had symptom or tumor progression that required MS. Microsurgery remains the only treatment option that offers symptom relief with a low recurrence rates [5, 18, 19, 40]. Although tinnitus did show a statistically significant improvement in MS compared to CM patients, half of these MS patients still suffered from this symptom postoperatively. Therefore, additional treatments for tinnitus should be considered, such as tinnitus retraining therapy, cognitive behavioral therapy or neuromodulation [66].
Limitations and literature critique
This current analysis tends to promote MS over CM in tinnitus, vertigo and dizziness improvement. As previously mentioned, confounding by indication was one of the major limitations of this study.
Furthermore, important information on patient and tumor characteristics were missing from several studies, such as tumor size, information that would allow us to have a better understanding of the relation between size and symptomatology, or size and the proper treatment option. Unfortunately, follow-up data were more often than not missing in the current literature. With the short follow-up lengths in the current study, the CM group’s outcome results might have been overestimated considering the natural evolution of the disease [67]. We therefore suggest that authors use the same guidelines proposed by the Committee of Hearing and Equilibrium for VS [68] when reporting data on ILS. Hearing status, tumor size, facial nerve function, treatment type and surgical approach should be described as raw data and symptom outcomes should be stated as unchanged, improved or worse. Follow-up lengths should minimally be of 3 months after the treatment and annual intervals afterward.
About the controversy regarding tumor appellation, it did not affect our collecting data, since all of the authors clearly described the tumor location. However, we agree with Bouchetemble et al., Zbar et al., Falcioni et al. and Di Lella et al. [5–8] that ILSs are different than isolated ILSs, since the only thing that differentiates VS to isolated ILSs is the initial location which may be impossible to determine, when the tumor occupies both the medial and lateral parts of the cochleovestibular nerve.
Conclusion
Intralabyrinthine schwannomas are a rare finding with few cases reported in the literature. Through this study we have been able to show that MS has a considerably more favorable outcome regarding symptom relief as compared to CM in patients with severe hearing loss suffering from tinnitus, vertigo or dizziness. In the absence of these symptoms, CM is the best option. In order to improve the quality of the studies available in the literature, we suggest the use the same guidelines proposed by the Committee of Hearing and Equilibrium for VS. This standardized approach will be beneficial to further understand the true pathophysiology of ILS.
References
Zhu AF, McKinnon BJ (2012) Transcanal surgical excision of an intracochlear schwannoma. Am J Otolaryngol 33:779–781
Johnson J, Lalwani AK (2012) Vestibular Schwannoma (Acoustic Neurinoma). In: Diagnosis and treatment in otolaryngology—head and neck surgery, McGraw-Hill, New-York
Kennedy RJ, Shelton C, Salzman KL et al (2004) Intralabyrinthine schwannomas: diagnosis, management, and a new classification system. Otol Neurotol 25:160–167
Van Abel KM, Carlson ML, Link MJ et al (2013) Primary inner ear schwannomas: a case series and systematic review of the literature. Laryngoscope 123:1957–1966
Bouchetemble P, Heathcote K, Tollard E et al (2013) Intralabyrinthine schwannomas: a case series with discussion of the diagnosis and management. Otol Neurotol 34:944–951
Falcioni M, Taibah A, Di Trapani G et al (2003) Inner ear extension of vestibular schwannomas. Laryngoscope 113:1605–1608
Zbar RI, Megerian CA, Khan A, Rubinstein JT (1997) Invisible culprit: intralabyrinthine schwannomas that do not appear on enhanced magnetic resonance imaging. Ann Otol Rhinol Laryngol 106:739–742
Di Lella F, Dispenza F, De Stefano A et al (2007) Management of intralabyrinthine schwannomas. Auris Nasus Larynx 34:459–463
Dubernard X, Somers T, Veros K et al (2014) Clinical presentation of intralabyrinthine schwannomas: a multicenter study of 110 cases. Otol Neurotol 35:1641–1649
Maseda E, Ablanedo ABlanco R et al (2007) [Intra-labyrinthine schwannoma: two-cases report. Acta otorrinolaringologica espanola 58:70–72
Dubrulle F, Kohler R, Vincent C et al (2010) Differential diagnosis and prognosis of T1-weighted post-gadolinium intralabyrinthine hyperintensities. Eur Radiol 20:2628–2636
Tieleman A, Casselman JW, Somers T et al (2008) Imaging of intralabyrinthine schwannomas: a retrospective study of 52 cases with emphasis on lesion growth. AJNR 29:898–905
Salzman KL, Childs AM, Davidson HC et al (2012) Intralabyrinthine schwannomas: imaging diagnosis and classification. AJNR 33:104–109
Gordts F, Van Der Veken P, Topsakal V et al (2011) A pilot with an intravestibular schwannoma: to fly or not to fly? Otol Neurotol 32:326–329
Jia H, Marzin A, Dubreuil C, Tringali S (2008) Intralabyrinthine schwannomas: symptoms and managements. Auris Nasus Larynx 35:131–136
Ohtani I, Suzuki C, Aikawa T (1990) Temporal bone pathology in intracochlear schwannoma with profound hearing loss. Auris Nasus Larynx 17:17–22
Hegarty JL, Patel S, Fischbein N et al (2002) The value of enhanced magnetic resonance imaging in the evaluation of endocochlear disease. Laryngoscope 112:8–17
Green JD Jr, McKenzie JD (1999) Diagnosis and management of intralabyrinthine schwannomas. Laryngoscope 109:1626–1631
Neff BA, Willcox TO Jr, Sataloff RT (2003) Intralabyrinthine schwannomas. Otol Neurotol 24:299–307
Iseri M, Ulubil SA, Topdag M, Oran A (2009) Hearing loss owing to intralabyrinthine schwannoma responsive to intratympanic steroid treatment. J Otolaryngol Head Neck Surg (Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale) 38:E95–E97
Jiang ZY, Kutz JW Jr, Roland PS, Isaacson B (2011) Intracochlear schwannomas confined to the otic capsule. Otol Neurotol 32:1175–1179
Karlan MS, Basek M, Potter GB (1972) Intracochlear neurilemmoma. Arch otolaryngol 96:573–575
Wanamaker HH (1972) Acoustic neuroma: primary arising in the vestibule. Laryngoscope 82:1040–1044
Schutt CA, Kveton JF (2014) Cochlear implantation after resection of an intralabyrinthine schwannoma. Am J Otolaryngol 35:257–260
Green JD Jr, Beatty CW, Czervionke LF et al (2000) Intracochlear vestibular schwannoma: a potential source for recurrence after translabyrinthine resection. Otolaryngol Head Neck Surg 123:281–282
Maniakas A, Saliba I (2012) Microsurgery versus stereotactic radiation for small vestibular schwannomas: a meta-analysis of patients with more than 5 years’ follow-up. Otol Neurotol 33:1611–1620
Maniakas A, Saliba I (2014) Neurofibromatosis Type 2 vestibular schwannoma treatment: a review of the literature, trends, and outcomes. Otol Neurotol 35:889–894
Donnelly MJ, Daly CA, Briggs RJ (1994) MR imaging features of an intracochlear acoustic schwannoma. J Laryngol Otol 108:1111–1114
Ozluoglu L, Jenkins HA (1994) Intralabyrinthine schwannoma. Arch Otolaryngol Head Neck Surg 120:1404–1406
Saeed SR, Birzgalis AR, Ramsden RT (1994) Intralabyrinthine schwannoma shown by magnetic resonance imaging. Neuroradiology 36:63–64
Weed DT, Teague MW, Stewart R, Schwaber MK (1994) Intralabyrinthine schwannoma: a case report. Otolaryngol Head Neck Surg 111:137–142
Gersdorff MC, Decat M, Duprez T, Deggouj N (1996) Intracochlear schwannoma. Eur Arch Otorhinolaryngol 253:374–376
Boutin P, Guth A, Bouccara D et al (1998) Intra-labyrinthine schwannomas: a report of two cases. Annales d’oto-laryngologie et de chirurgie cervico faciale: bulletin de la Societe d’oto-laryngologie des hopitaux de Paris 115:35–41
Deux JF, Marsot-Dupuch K, Ouayoun M et al (1998) Slow-growing labyrinthine masses: contribution of MRI to diagnosis, follow-up and treatment. Neuroradiology 40:684–689
Roland PS, Gilmore J (1998) Intracochlear schwannoma. Otolaryngol Head Neck Surg 119:681–684
Montague ML, Kishore A, Hadley DM, O’Reilly BF (2002) MR findings in intralabyrinthine schwannomas. Clin Radiol 57:355–358
Khurana VG, Link MJ, Driscoll CL, Beatty CW (2003) Evolution of a cochlear schwannoma on clinical and neuroimaging studies. Case report. J Neurosurg 99:779–782
Jackson LE, Hoffmann KK, Rosenberg SI (2003) Intralabyrinthine schwannoma: subtle differentiating symptomatology. Otolaryngol Head Neck Surg 129:439–440
Machner B, Gottschalk S, Sander T et al (2007) Intralabyrinthine schwannoma affecting the low but not high frequency function of the vestibulo-ocular reflex: implications for the clinical diagnosis of chronic peripheral vestibular deficits. J Neurol Neurosurg Psychiatry 78:772–774
Shin SH, Chun YM, Lee HK (2008) A cochlear schwannoma presenting with sudden hearing loss. Eur Arch Otorhinolaryngol 265:839–842
Nishimura T, Hosoi H (2008) Progressive hearing loss in intracochlear schwannoma. Eur Arch Otorhinolaryngol 265:489–492
Shin YR, Choi SJ, Park K, Choung YH (2009) Intralabyrinthine schwannoma involving the cochlea, vestibule, and internal auditory canal: ‘canalolabyrinthine schwannoma’. Eur Arch Otorhinolaryngol 266:143–145
Magliulo G, Colicchio G, Romana AF, Stasolla A et al (2010) Intracochlear schwannoma. Skull base 20:115–118
Yoshida T, Sone M, Naganawa S, Nakashima T (2011) Accuracy of 3.0 Tesla magnetic resonance imaging in the diagnosis of intracochlear schwannoma. Auris Nasus Larynx 38:551–554
Choi JS, Kim YH, Han CD, Kim KS (2012) Intravestibular space occupying lesions of lipoma and schwannoma. Auris Nasus Larynx 39:431–433
Kim YH, Jun BC, Yun SH, Chang KH (2013) Intracochlear schwannoma extending to vestibule. Auris Nasus Larynx 40:497–499
Carlson DN, Voth SE, Sataloff RT (2013) Intracochlear Schwannoma. J Case Rep Med 2:1–5
Mayer O (1917) Ein fall von multiplen tumoren in den Endausbreitungen des Akustikus. ZOhrenheilkd 75:95–113
Fitzgerald DC, Grundfast KM, Hecht DA, Mark AS (1999) Intralabyrinthine schwannomas. Am J Otol 20:381–385
Miyamoto RT, Isenberg SF, Culp WM, Tubergen LB (1980) Isolated intralabyrinthine schwannoma. Am J Otol 1:215–217
Doyle KJ, Brackmann DE (1994) Intralabyrinthine schwannomas. Otolaryngol Head Neck Surg 110:517–523
Lee SK, Choe (2013) The Ct and magnetic resonance imaging features of transotic schwannoma: a case report. J Korean Soc Radiol 68:281–284
Yang I, Aranda D, Han SJ et al (2009) Hearing preservation after stereotactic radiosurgery for vestibular schwannoma: a systematic review. J Clin Neurosci 16:742–747
Sataloff RT, Roberts BR, Feldman M (1988) Intralabyrinthine schwannoma. Am J Otol 9:323–326
DeLozier HL, Gacek RR, Dana ST (1979) Intralabyrinthine schwannoma. Ann Otol Rhinol Laryngol 88:187–191
Miller ME, Moriarty JM, Linetsky M et al (2012) Intracochlear schwannoma presenting as diffuse cochlear enhancement: diagnostic challenges of a rare cause of deafness. Ir J Med Sci 181:131–134
Vernick DM, Graham MD, McClatchey KD (1984) Intralabyrinthine schwannoma. Laryngoscope 94:1241–1243
Wolf JS, Mattox DE (1999) Imaging quiz case 2. Intralabyrinthine schwannoma. Arch Otolaryngol Head Neck Surg 125:107–109
Huang TS (1986) Primary intralabyrinthine schwannoma. Ann Otol Rhinol Laryngol 95:190–192
Wanamaker HH (1972) Acoustic neuroma: primary arising in the vestibule. Laryngoscope 82:1040–1044
Weymuller EA Jr (1975) Unsuspected intravestibular schwannoma. Arch Otolaryngol 101:630–632
Karlan MS, Basek M, Potter GB (1972) Intracochlear neurilemmoma. Arch Otolaryngol 96:573–575
Grayeli AB, Fond C, Kalamarides M et al (2007) Diagnosis and management of intracochlear schwannomas. Otol Neurotol 28:951–957
Langguth B, Kreuzer PM, Kleinjung T, De Ridder D (2013) Tinnitus: causes and clinical management. Lancet Neurol 12:920–930
Kanzaki J, Tos M, Sanna M et al (2003) New and modified reporting systems from the consensus meeting on systems for reporting results in vestibular schwannoma. Otol Neurotol 24:642–648 (discussion 648–649)
Vander Ghinst M, Verbeurgt C, Hassid S, Choufani G (2013) Tinnitus management in 2013. Rev Med Brux 34:245–250
Lee JD, Park MK, Kim JS, Cho YS (2014) the factors associated with tumor stability observed with conservative management of intracanalicular vestibular schwannoma. Otol Neurotol 35:918–921
Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma) (1995) American Academy of Otolaryngology–Head and Neck Surgery Foundation, Inc.. Otolaryngol Head Neck Surg: official journal of American Academy of Otolaryngology-Head and Neck Surgery 113:179–180
Acknowledgments
The following are acknowledged for giving specifications on their data: Kathryn M. Van Abel, M.D.; Lance E. Jackson, M.D.; Brandon Isaacson, M.D.; Robert T. Sataloff, M.D.; Karen Salzman, M.D.; Clough Shelton, M.D. and Jan Casselman, MD. No funding was received for this work from any of the following organizations: NIH, Welcome Trust, HHMI or other.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gosselin, É., Maniakas, A. & Saliba, I. Meta-analysis on the clinical outcomes in patients with intralabyrinthine schwannomas: conservative management vs. microsurgery. Eur Arch Otorhinolaryngol 273, 1357–1367 (2016). https://doi.org/10.1007/s00405-015-3548-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3548-2